
What cells are involved in graft rejection?
Are memory cells responsible for tissue graft rejection? Because of their capacity to rapidly generate effector immune responses upon rechallenge, memory T cells appear to be particularly efficient at mediating allograft rejection. In addition, memory T cells are less sensitive than naïve T cells to many immunosuppressive strategies.
Why do memory T cells mediate allograft rejection?
· Also, are memory cells responsible for tissue graft rejection? Because of their capacity to rapidly generate effector immune responses upon rechallenge, memory T cells appear to be particularly efficient at mediating allograft rejection. In addition, memory T cells are less sensitive than naïve T cells to many immunosuppressive strategies.
Can non-self graft tissue avoid rejection?
Are memory cells responsible for tissue graft rejection? Because of their capacity to rapidly generate effector immune responses upon rechallenge, memory T cells appear to be …
Do B cells play a role in allograft rejection?
T cells and B cells mainly control the antigen-specific rejection and act either as effector, regulatory, or memory cells. On the other hand, nonspecific cells such as endothelial cells, NK …
Which cell is responsible for tissue graft rejection?
Mechanisms of rejection. The immune response to a transplanted organ consists of both cellular (lymphocyte mediated) and humoral (antibody mediated) mechanisms. Although other cell types are also involved, the T cells are central in the rejection of grafts.
What's responsible for graft rejection?
So, the correct answer is 'T-Lymphocytes Mediated'.
What is responsible for graft rejection during transplantation?
It is caused by the presence of pre-existing antibodies in the recipient that recognize antigens in the donor organ. These antigens are located on the endothelial lining of blood vessels within the transplanted organ and, once antibodies bind, will lead to the rapid activation of the complement system.
What two cell types are mainly responsible for graft rejection?
T cells and B cells mainly control the antigen-specific rejection and act either as effector, regulatory, or memory cells. On the other hand, nonspecific cells such as endothelial cells, NK cells, macrophages, or polymorphonuclear cells are also crucial actors of transplant rejection.
What factors cause transplant rejection?
Certain cancers (in some people who take strong immune-suppressing medicines for a long time) Infections (because the person's immune system is suppressed by taking immune-suppressing medicines) Loss of function in the transplanted organ/tissue. Side effects of medicines, which may be severe.
What exactly is the role of T cells?
T cells are a part of the immune system that focuses on specific foreign particles. Rather than generically attack any antigens, T cells circulate until they encounter their specific antigen. As such, T cells play a critical part in immunity to foreign substances.
Which substances produced in the body are directly responsible for the rejection of a transplanted organ?
Antibodies binding at the time of transplantation can cause hyperacute rejection, and antibodies produced after transplantation can cause acute vascular rejection (also called humoral rejection and antibody-mediated rejection) or chronic rejection.
What are the types of graft rejection?
There are three major types of allograft rejection: Hyperacute, acute, and chronic rejection.
When the organ is transplanted and rejected by the body the cells responsible are?
lymphocytesWhen an organ is transplanted and is rejected by the body, the lymphocytes are produced byQuestionWhen an organ is transplanted and is rejected by the body, the lymphocytes are produced byChapter NameHealth And DiseaseSubjectBiology (more Questions)Class12thType of AnswerVideo & Image4 more rows•Apr 17, 2022
What is the purpose of memory cells?
Memory cells are long-lived immune cells capable of recognizing foreign particles they were previously exposed to (thus, the memory in their name).
Which type of immune response is responsible for the rejection of tissue organs in the patient's body post?
So, the correct answer is 'Cell-mediated immune response'
What are the three types of graft rejection?
There are three major types of allograft rejection: Hyperacute, acute, and chronic rejection.
Which type of immune response is responsible for the rejection of tissue organs in the patient's body post?
So, the correct answer is 'Cell-mediated immune response'
What is the role of T cells in transplant rejection?
T cells are central to the process of transplant rejection through allorecognition of foreign antigens leading to their activation, and the orchestration of an effector response that results in organ damage.
How are memory T cells generated?
Memory T cells can also be generated through homeostatic proliferation in a lymphopenic environment, including potentially alloreactive and pathogenic T cells ( 13 – 15 ). Such homeostatically expanded memory T cells can impair tolerance induction to allografts ( 15 – 17 ).
What are memory T cells?
Memory T cells are characterized by their low activation threshold, robust effector functions, and resistance to conventional immunosuppression and costimulation blockade. Unlike their naïve counterparts, memory T cells reside in and recirculate through peripheral non-lymphoid tissues.
What are the functions of memory T cells?
Memory T cells have been traditionally divided into two major subsets with largely overlapping functions but distinct trafficking patterns (Figure 1 ). Central memory T cells (Tcm) express lymphoid homing markers CCR7 and CD62L, whereas effector memory T cells (Tem) are CCR7 − CD62L − but instead express molecules that promote migration into peripheral tissues ( 20 – 23 ). In humans, but not in mice, some memory T cells [terminally differentiated effector memory T cells (Temra)] re-express naive T cell surface marker CD45RA, while downregulating expression of CCR7, CD62L, and CD28, and represent a terminal stage of effector differentiation ( 21, 24, 25 ). Recent studies demonstrated that some T cells in peripheral tissues do not circulate and represent a distinct subset of tissue-resident memory T cells (Trm) ( 24, 26 – 28 ). Trm cells express early activation marker CD69 and αEβ7 integrin CD103 along with a number of tissue-specific chemokine receptors ( 26, 29 – 32 ). There is accumulating evidence that Trm cells play an important role in host protection against infections. It is conceivable that Trm cells of both donor and recipient origins may influence transplant outcome by facilitating GVHD or allograft rejection, respectively. However, the proportion of alloreactive T cells among Trm subset and the potential contribution of such cells following transplantation remain to be addressed. Another important type of memory T cells relevant to transplantation is CD4 + CXCR5 hi follicular helper (Tfh) cells that reside in B cell follicles within secondary lymphoid organs and are essential for optimal B cell responses and antibody generation ( 33 ). As memory T cells in secondary lymphoid and non-lymphoid peripheral tissues are spared by antibody-mediated lymphoablation ( 34) Trm cells may be harder to control compared to circulating memory T cells.
What are the costimulatory pathways for T cells?
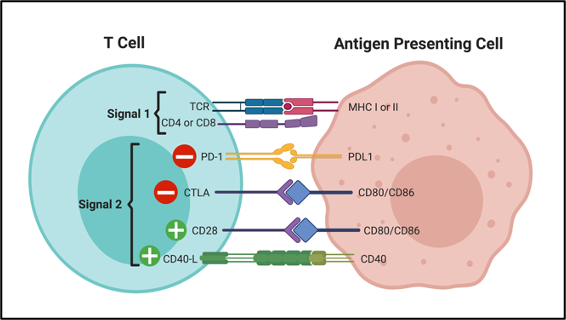
In addition to CD28/B7 and CD40/CD154 costimulation, several other costimulatory pathways may play a role in effector/memory T cell functions. Inhibition or genetic lack of ICOS/B7RP-1, CD134/CD134L, CD70/CD27, or CD137/CD137L improved allograft survival even in donor-sensitized recipients, or after delayed administration which allowed initial priming of donor-reactive T cells [reviewed in Ref. ( 129 )]. It was revealed that these costimulatory pathways might control distinct aspects of the alloimmune response. For example, blocking anti-CD134L mAb inhibits proliferation of effector T cells while supporting the survival of Tregs ( 71, 130 ). Conversely, signaling through CD134 inhibits immunosuppressive properties of FoxP3 + Tregs and promotes allograft rejection ( 131, 132 ). ICOS/B7RP-1 blockade of resting memory CD4 + T cells inhibits their helper functions and decreases alloantibody production. In contrast, circulating memory CD8 + T cells are ICOS lo, but rapidly upregulate ICOS surface expression upon graft infiltration. These examples demonstrate that the complexity of costimulatory pathways governing alloimmune responses must be considered when costimulatory blockade is used as part of immunosuppression regimen.
Where are T cells found in monkeys?
Our laboratory showed that a sizable proportion of endogenous memory T cells found in peripheral blood, and secondary lymphoid organs of naïve cynomolgus monkeys are allospecific. Most Tem were CD8 + CD95 + CD28 − IFNγ-producing cells located in the spleen, peripheral blood, and bone marrow while IL-2-producing Tcm were primarily CD4 + CD95 + CD28 + and limited to the lymph nodes and spleen ( 12 ). Based upon this observation, we studied the influence of pretransplant memory T cell alloreactivity on rejection versus tolerance of kidney allografts in monkeys ( 61 ). A series of cynomolgus monkeys were conditioned [whole body and thymic irradiations + horse antithymocyte globulin (ATG) treatment] and received a combined kidney and bone marrow transplantation from the same allogeneic donor ( 62 ). The animals then received a short-term immunosuppression treatment comprised of anti-CD40L antibodies and cyclosporine A ( 62 ). This procedure resulted in a transient multilineage hematopoietic chimerism and achieved long-term survival of kidney allografts (>1 year) after withdrawal of immunosuppression in 70% of the monkeys ( 62 ). On the other hand, approximately 30% of the treated monkeys rejected their allograft in an acute fashion within 100–200 days posttransplantation ( 61 ). In this model, we observed that the vast majority of tolerant animals displayed low frequencies of donor-reactive memory T cells ( 61 ). It is noteworthy that no differences between homeostatic expansion of memory T cells were observed between monkeys which rejected or accepted kidney allografts ( 61 ).
Why are trm cells important?
There is accumulating evidence that Trm cells play an important role in host protection against infections. It is conceivable that Trm cells of both donor and recipient origins may influence transplant outcome by facilitating GVHD or allograft rejection, respectively.
Do endogenous T cells prevent tolerance?
In laboratory rodents, endogenous memory T cells generated through heterologous immunity have little ability to prevent tolerance induction given that hematopoietic chimerism and/or costimulation blockade regularly achieve tolerance of fully allogeneic transplants ( 53 – 55 ). In contrast, mice that have been sensitized to allogeneic MHC through transplantation or multiple viral infections become resistant to tolerance induction ( 11, 39, 56, 57 ). Moreover, naïve mice adoptively transferred with alloreactive memory T cells display similar resistance to tolerogenesis via hematopoietic chimerism or costimulation blockade ( 11, 39, 56, 57 ). Therefore, in laboratory rodents, antigen-induced rather than endogenous memory T cells prevent transplant tolerance. It is still unclear whether this difference relies on the low frequency of endogenous memory T cells or on the fact that these two subsets of memory T cells are different in nature.
What is the process of rejection of an allograft?
Rejection of solid organ allografts is the result of a complex series of interactions involving coordination between both the innate and adaptive immune system with T cells central to this process. The ability of recipient T cells to recognize donor-derived antigens, called allorecognition, initiates allograft rejection. Once recipient T cells become activated, they undergo clonal expansion, differentiate into effector cells, and migrate into the graft where they promote tissue destruction. In addition, CD4 T cells help B cells produce alloantibodies. Here, we will review the components of an anti-allograft adaptive immune response.
What is the stimulus for rejection in MHC-identical transplantation?
The stimulus for rejection in this situation is donor minor antigen peptide MHC class I and class II complexes. These complexes can theoretically be produced by donor cells themselves or by recipient phagocytes after engulfing donor cells or debris. The magnitude of the T cell response would be small at first because the frequency of T cell clones reactive to processed peptides from donor MHC proteins presented by recipient DC is orders of magnitude lower than the frequency of T cells specific for allogeneic MHC molecules [52]. However, a recent study demonstrated that the frequency of graft-specific T cells activated via the indirect pathway influences the ability of the costimulatory blockade to be effective in promoting graft survival [53].
How do T cells recognize MHC?
The indirect pathway of allorecognition describes the ability of T cells to recognize donor MHC molecules that are processed and presented as peptides by self-MHC molecules (Fig. 1b). The recognition of intact donor MHC mole cule(s) elicits a potent anti-graft immune response while processed MHC peptides and minor histocompatibility antigens elicit a slower tempo, less intense immune response.
What are the two pathways of allorecognition?
Two distinct pathways of allorecognition. aDirect pathway of allorecognition. Dendritic cells migrate from the graft to secondary lymphoid tissues to activate T cells. bIndirect pathway of allorecognition. Graft proteins are processed by recipient dendritic cells and presented to T cells. APCAntigen-presenting cell, TCRT cell receptor, MHCmajor histocompatibility complex
Which T cells are more sensitive to antigens?
Memory T cells can be divided into central memory and effector memory subsets based on their circulation pattern and functional responsiveness. Memory T cells have been shown to be more sensitive to antigen, function more rapidly, produce effector cytokines, survive longer, and show less dependence on CD28 costimulation than their naïve counterparts [124–129].
Do T cells respond to MHC?
T cells will respond vigorously when mixed in culture with MHC-disparate stimulator cells, i.e. the mixed lymphocyte reaction [8]. This in vitro response is thought to reflect the propensity for acute rejection [9], and the ability to detect an alloresponse with the mixed lymphocyte culture is generally believed to be due to the high precursor frequency of alloreactive T cells within the periphery. Mature, naïve T cells in circulation survive a selection process in the thymus that ensures that their TCR has a low but significant affinity for a self-peptide/MHC molecule but a high affinity for foreign peptides associated with self-MHC molecules [10, 11]. Recent studies have shown that the weak interaction between self-MHC and the TCR is required for the survival of naive T cells in the periphery [12]. The inherent affinity of the TCR on mature T cells for self peptide-MHC complexes probably explains the high frequency of T cells within any individual that cross react with high affinity to a closely related allo-MHC molecule [13, 14].
Does renal allograft injury cause rejection?
Activation of the innate immune response can initiate acute rejection and contribute to the development of chronic allograft nephropathy. The mechanism by which ischemia reperfusion injury promotes rejection is likely to be multifactorial. Studies have shown that reperfusion injury activates both a cellular response and humoral factors of the innate immune system.
What is the role of T cells in graft rejection?
Role of T cells in graft rejection and transplantation tolerance. Transplantation is the most effective treatment for end-stage organ failure, but organ survival is limited by immune rejection and the side effects of immunosuppressive regimens. T cells are central to the process of transplant rejection through allorecognition ...
Why are T cells important?
T cells are central to the process of transplant rejection through allorecognition of foreign antigens leading to their a …. Transplantation is the most effective treatment for end-stage organ failure, but organ survival is limited by immune rejection and the side effects of immunosuppressive regimens. T cells are central to the process of ...
What is graft movement?
Grafts are typically moved without their attachments to the circulatory system and must reestablish these, in addition to the other connections and interactions with their new surrounding tissues. There are different types of grafts depending on the source of the new tissue or organ.
Why is it important to match the HLAs of the host and donor as closely as possible in bone marrow
To minimize the risk of GVHD, it is critically important to match the HLAs of the host and donor as closely as possible in bone marrow transplants. In addition, the donated bone marrow is processed before grafting to remove as many donor APCs and T cells as possible, leaving mostly hematopoietic stem cell s.
What is the purpose of genetic modification in pigs?
An alternative approach that is gaining renewed research interest is genetic modification of donor animals, such as pigs, to provide transplantable organs that do not elicit an immune response in the recipient . The approach involves excising the genes in the pig (in the embryo) that are most responsible for the rejection reaction after transplantation. Finding these genes and effectively removing them is a challenge, however. So too is identifying and neutralizing risks from viral sequences that might be embedded in the pig genome, posing a risk for infection in the human recipient.
Can SLE be cured?
SLE cannot be cured , but there are various therapies available for reducing and managing its symptoms. Specific therapies are prescribed based on the particular symptoms presenting in the patient. Kerry's rheumatologist starts her therapy with a low dose of corticosteroid s to reduce her rashes.
Do T cells kill grafts?
Cytotoxic T cells then target and kill the grafted cells through the same mechanism they use to kill virus-infected cells; helper T cells may also release cytokines that activate macrophages to kill graft cells. Types of Tissue and Organ Grafts and Their Complications. Graft. Procedure.
Can non-self tissues be transplanted?
Nonetheless, the practice of transplanting non-self tissues may soon become obsolete. Scientists are now attempting to develop methods by which new organs may be grown in vitro from an individual’s own harvested cells to replace damaged or abnormal ones. Because organs produced in this way would contain the individual’s own cells, they could be transplanted into the individual without risk for rejection.
Can MHC be used to graft tissue?
Because of this, no non-self grafted tissue is likely to completely avoid rejection. However, the more similar the MHC gene match, the more likely the graft is to be tolerated for a longer time. Most transplant recipients, even those with tissues well matched to their MHC genes, require treatment with immunosuppressant drug s for the rest of their lives. This can make them more vulnerable than the general population to complications from infectious diseases. It can also result in transplant-related malignancies because the body’s normal defenses against cancer cells are being suppressed.

Introduction
Basic Biology of Alloreactive Memory T Cells
- Origins of Alloreactive Memory T Cells
Laboratory rodents display low frequencies of memory T cells (5–10% of all T cells). In the absence of prior exposure to alloantigens, 1–10% of these memory T cells can react to allogeneic major histocompatibility complex (MHC) molecules in vitro (5). In mice, these cells called endog… - Location of Memory T Cells
Memory T cells have been traditionally divided into two major subsets with largely overlapping functions but distinct trafficking patterns (Figure 1). Central memory T cells (Tcm) express lymphoid homing markers CCR7 and CD62L, whereas effector memory T cells (Tem) are CCR7−…
Contribution of Memory T Cells to Allograft Rejection and Tolerance
- Role in Allograft Rejection
During the past decade, studies investigating CD4+ versus CD8+ memory T cells revealed that these subsets contribute to allograft rejection through distinct mechanisms. Indeed, memory CD4+ T cells not only become effector cells upon reactivation, but also provide help for the robu… - Influence of Memory T Cells on Allograft Tolerance
In laboratory rodents, endogenous memory T cells generated through heterologous immunity have little ability to prevent tolerance induction given that hematopoietic chimerism and/or costimulation blockade regularly achieve tolerance of fully allogeneic transplants (53–55). In co…
Recent Developments in Targeting Alloreactive T Cell Memory
- Lymphoablation
Induction therapy is widely used in clinical transplantation to overcome the deleterious effects of preexisting donor-reactive immunity. Antibody-mediated lymphocyte depletion is most commonly used induction strategy, particularly in highly sensitized patients and in patients receiving margi… - Costimulatory Blockade
Belatacept, a second generation of CTLA4-Ig, is currently used in clinical transplantation to prevent allograft rejection and minimize the toxic side effects of calcineurin inhibitors (97). Despite reduced side effects and improved graft survival, belatacept-treated patients have highe…
Concluding Remarks
- While other types of immunologic memory lymphocytes such as memory B cells, preexisting alloantibodies, and “innate memory” described for NK cells and macrophages can impact transplant outcomes, in this review, we focused exclusively on T cell memory. It is now firmly established that alloreactive memory T cells accelerate allograft rejection and prevent transplan…
Author Contributions
- GB, AV, BG, JM, and KA wrote portions of the manuscript; GB and AV edited the manuscript and prepared it for submission.
Conflict of Interest Statement
- The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
- This study was supported by NIH grants R21AI111191 and R21AI117466 to GB and R01AI113142 and 2PO1 AI087586-06 to AV.
Abbreviations
- MHC, major histocompatibility complex; APC, antigen-presenting cell; Treg, regulatory T cell; IFNγ, gamma interferon; TNFα, tumor necrosis factor alpha; CTL, cytotoxic T lymphocyte; DC, dendritic cell; DSAs, donor-specific antibodies.