Common Causes
difficile colitis includes:
- correction of dehydration and electrolyte (mineral) deficiencies,
- discontinuing the antibiotic that caused the colitis, and
- using antibiotics to eradicate the C. difficile bacterium.
Related Conditions
C. diff (also known as Clostridioides difficile or C. difficile) is a germ (bacterium) that causes severe diarrhea and colitis (an inflammation of the colon).. It’s estimated to cause almost half a million infections in the United States each year.
What is the treatment for C diff colitis?
Keflex has fewer serious side effects than Cipro, for example, anaphylaxis, a type of severe allergic reaction. Cipro and Keflex both can cause a serious infection with C. difficile, which causes severe, chronic diarrhea and may lead to pseudomembranous colitis.
What is severe C diff?
Clostridium difficile infection (C diff) is a bowel infection caused by toxin-producing bacteria. C diff is a serious infection that can range from mild diarrhea to severe inflammation of your colon that can be life threatening. C diff is not caused by anything you eat and you can’t cure it with diet changes.
Does Keflex cause C diff?
What is chronic C diff?

What is the most common cause for developing pseudomembranous colitis?
Pseudomembranous colitis, a severe inflammation of the inner lining of the large intestine, manifests as an antibiotic-associated colonic inflammatory complication. The disease most commonly results from a serious Clostridium difficile infection, an increasing nosocomial issue over the last two decades.
Can C. diff cause colitis?
C. diff (also known as Clostridioides difficile or C. difficile) is a germ (bacterium) that causes diarrhea and colitis (an inflammation of the colon). It's estimated to cause almost half a million infections in the United States each year.
What is the most common infection caused by Clostridium difficile?
Clostridium difficile is the most common cause of nosocomial infectious diarrhea. The incidence of C difficile infection (CDI) is increasing in both inpatients and outpatients, and outbreaks caused by a hypervirulent strain of C difficile are resulting in more severe disease.
What complications are associated with C. diff?
Complications of C. difficile infection include:Dehydration. Severe diarrhea can lead to a significant loss of fluids and electrolytes. ... Kidney failure. ... Toxic megacolon. ... A hole in your large intestine (bowel perforation). ... Death.
Can C. diff cause permanent damage to colon?
diff toxins can irritate the lower part of the intestines (a condition called colitis). The colon then swells and becomes inflamed. If this gets bad enough, the intestines can rupture. 8 In those cases, the damaged intestines need to be removed in surgery and can leave scars and longer-term gut problems.
When should you suspect pseudomembranous colitis?
Pseudomembranous colitis is an inflammatory condition of the colon characterized by elevated yellow-white plaques that coalesce to form pseudomembranes on the mucosa. Patients with the condition commonly present with abdominal pain, diarrhea, fever, and leukocytosis.
What are the warning signs of C. diff?
Clostridium Difficile (C. diff) SymptomsDiarrhea more than 10 times a day.Severe cramping.Fever.Nausea.Loss of appetite/weight loss.Dehydration.Rapid heart rate.
What organs are affected by C. diff?
diff., is a bacteria spread by microscopic spores. Clostridium difficile is the former name. The bacteria cause inflammation of the gut or colon – colitis. This can lead to moderate-to-severe diarrhea, and sometimes sepsis, which can develop as the body tries to fight the infection.
What antibiotic has the highest risk for C difficile infection?
The primary risk factor for C difficile colitis is previous exposure to antibiotics; the most commonly implicated agents include the cephalosporins (especially second and third generation), the fluoroquinolones, ampicillin/amoxicillin, and clindamycin.
Can C. diff have long term effects?
However, data on the long-term consequences of CDAD are scarce. Among other infectious diseases (Shigella, Salmonella, and Campylobacter), long-term consequences such as irritable bowel syndrome (IBS), chronic dyspepsia/diarrhea, and other GI effects have been noted.
Can C. diff damage your intestines?
The C difficile bacterium produces toxins (poisonous substances) that attack the lining of the colon and can cause severe damage to the colon itself. More commonly, C difficile toxins produce diarrhea and abdominal discomfort.
What happens if C. diff doesn't go away?
At first, your symptoms may include diarrhea and cramping. The later stages are flu-like symptoms, including weakness, dehydration, fever, nausea, vomiting, and—in advanced stages—blood in your stool/feces. If a patient is left untreated, he/she can die from it. C.
How long does colitis last after C. diff?
Although in about 20% of patients, CDI will resolve within two to three days of discontinuing the antibiotic to which the patient was previously exposed, CDI should usually be treated with an appropriate course (about 10 days) of treatment, including oral vancomycin or fidaxomicin.
Can C. diff colitis be cured?
People with Clostridium difficile infections typically recover within two weeks of starting antibiotic treatment. However, many people become reinfected and need additional therapy. Most recurrences happen one to three weeks after stopping antibiotic therapy, although some occur as long as two or three months later.
How many people are infected with C. difficile?
It most commonly affects older adults in hospitals or in long-term care facilities. In the United States, about 200,000 people are infected annually with C. difficile in a hospital or care setting. These numbers are lower than in previous years because of improved prevention measures.
Where is C. difficile found?
C. difficile bacteria are found throughout the environment — in soil, air, water, human and animal feces, and food products, such as processed meats. A small number of healthy people naturally carry the bacteria in their large intestines and don't have ill effects from the infection.
What is the bacterium that causes diarrhea?
Clostridium difficile (klos-TRID-e-um dif-uh-SEEL), also known as Clostridioides difficile and often referred to as C. difficile or C. diff, is a bacterium that can cause symptoms ranging from diarrhea to life-threatening inflammation of the colon. Illness from C. difficile most commonly affects older adults in hospitals or in long-term care ...
What is the condition that causes enlargement of the colon?
C. difficile infection that is severe and sudden, an uncommon condition, may also cause intestinal inflammation leading to enlargement of the colon (also called toxic megacolon) and sepsis. Sepsis is a life-threatening condition that occurs when the body's response to an infection damages its own tissues. People who have these conditions are admitted to the intensive care unit.
How do you know if you have C. difficile?
difficile infection are: Watery diarrhea three or more times a day for two or more days. Mild abdominal cramping and tenderness.
How many people get C. difficile each year?
Each year in the United States, about a half million people get sick from C. difficile, and in recent years, C. difficile infections have become more frequent, severe and difficult to treat. Recurrent C. difficile infections also are on the rise. C. difficile infection care at Mayo Clinic.
How many bacteria are in the intestines?
Your intestines contain about 100 trillion bacterial cells and up to 2,000 different kinds of bacteria, many of which help protect your body from infection. When you take an antibiotic to treat an infection, these drugs tend to destroy some of the normal, helpful bacteria in addition to the bacteria causing the infection. Without enough healthy bacteria to keep it in check, C. difficile can quickly grow out of control. The antibiotics that most often lead to C. difficile infections include:
What is pseudomembrane colitis?
Pseudomembranous colitis is an inflammatory condition of the colon characterized by elevated yellow-white plaques that coalesce to form pseudomembranes on the mucosa. Patients with the condition commonly present with abdominal pain, diarrhea, fever, and leukocytosis.
When was Clostridium difficile first described?
Clostridium difficilewas first described in 1935 , but its association with antibiotics and PMC was not described until the 1970s, corresponding with an increased use of broad-spectrum antibiotics.7C. difficileis an obligate anaerobic organism and toxin-producing gram-positive rod with the ability to form spores.8This latter characteristic lends itself to acquisition from the environment, particularly in nosocomial settings. It has been identified as the causative agent in 15–30% of antibiotic-associated diarrhea and as the primary cause of antibiotic-associated colitis.9
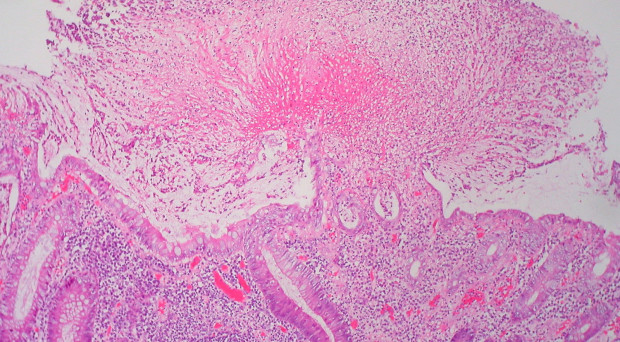
What is PMC on the colon?
On endoscopic examination, PMC is characterized by elevated yellow-white nodules or plaques that form pseudomembranes on the mucosal surfaces of the colon (Figure 1).2,3Endothelial damage from the initial event or disease process causes small areas of necrosis in the surface epithelium. The eruption of neutrophils, nuclear debris, and other inflammatory elements from the lamina propria onto the epithelium then leads to pseudomembrane formation.4,5Pseudomembranes can be up to two centimeters in diameter, scattered among areas of normal or erythematous mucosa; however, confluent pseudomembranes that cover the entirety of the mucosa can be seen in severe disease.4,6
What is PMC in medicine?
Pseudomembranous colitis ( PMC) is a manifestation of severe colonic disease that is usually associated with Clostridium difficileinfection, but can be caused by a number of different etiologies. Prior to the use of broad-spectrum antibiotics, PMC was more frequently related with ischemic disease, obstruction, sepsis, uremia, and heavy metal poisoning.1The list of associated etiologies is vast, although Clostridium difficileinfection (CDI) is still the most common cause.
What are the most common causes of PMC?
This article will review the many diverse etiologies of PMC (Table 1). Although CDI is the most common cause, other less common etiologies of PMC will be described. These include ischemic colitis, collagenous colitis, inflammatory bowel disease, viral infection with cytomegalovirus (CMV), numerous bacterial and parasitic organisms, and multiple drugs and toxins. The purpose of this comprehensive review is to aid the general practitioner in the diagnosis of both typical (C. difficle) and atypical (non-C. difficile) causes of PMC.
What are the symptoms of CDI?
The clinical presentation of CDI is highly variable, ranging from the asymptomatic carrier to the patient with PMC, fulminant colitis, and toxic megacolon.5,10,11Accompanying signs and symptoms include fever, leukocytosis, abdominal cramping, and non-specific radiographic findings of colitis or megacolon. Severe cases can present with profound leukocytosis (with reports of white blood cell counts up to 100,000/mm3), hypovolemia, hypotension, hypoalbuminemia/protein-losing enteropathy, renal dysfunction, and reactive arthritis.3,9–12It is estimated that 3–8% of patients with CDI develop fulminant infection, which includes severe ileus, toxic megacolon, colonic perforation with subsequent peritonitis, and septic shock; many of these patients require colectomy and have an overall high mortality.13
How long does it take to treat a mild to moderate CDI?
Mild-to-moderate disease is typically defined as CDI with diarrhea and other symptoms not consistent with severe illness; recommended treatment is oral metronidazole for 10–14 days or oral vancomycin for 10–14 days if the patient cannot tolerate or does not improve significantly while on metronidazole.9,11,28,32Important adverse reactions of metronidazole therapy include nausea, vomiting, taste disturbances, and dose-dependent neurotoxicity.9Of note, fidaxomicin, a macrolide antibiotic, was approved for the treatment of mild-moderate CDI in 2011. Two separately conducted phase III, randomized, double-blinded trials demonstrated non-inferiority when compared to oral vancomycin; further analysis proposed that fidaxomicin might be superior in preventing recurrences in non-NAP1/BI/027 strains, although the small number of trials and short duration of follow-up limits additional conclusions. Moreover, fidaxomicin is much more expensive than vancomycin, and it is unclear if its proposed benefits outweigh the cost.28,33–35
What is the most common organism that is associated with pseudomembranous colitis?
C difficile is the organism most commonly linked to pseudomembranous colitis, but other bacterial, viral, and parasitic pathogens have also been implicated. Staphylococcus aureus was believed to be responsible for enterocolitis in a series of 155 surgical patients between 1958 and 1962 receiving antibiotic therapy.
What is the test for C difficile?
Testing for C difficile is with polymerase chain reaction, enzyme immunoassay for toxins A and B, and glutamate dehydrogenase measurement.
What is a pseudomembrane?
A pseudomembrane is a layer of fibropurulent exudate composed of acute inflammatory cells and mucus originating from inflamed and erupting crypts. 2 Although most often seen in C difficile infection, pseudomembranous colitis is a nonspecific pattern of injury resulting from decreased oxygenation, endothelial damage, and impaired blood flow to the mucosa that can be triggered by a number of disease states. 2
What are the factors that predispose to pseudomembrane formation?
Chemicals, medications, ischemia, microscopic colitis, other infectious organisms, and inflammatory conditions can all predispose to pseudomembrane formation and should be included in the differential diagnosis. As most patients with pseudomembranous colitis have C difficile infection, it should be excluded first.
What is pseudomembrane on endoscopy?
On endoscopy, pseudomembranes appear as raised whitish or yellowish plaques that may be scattered or confluent in distribution ( Figure 1 ). 2 They are usually found in the rectosigmoid colon but may be isolated to more proximal segments. 3 Lower endoscopy is often performed in the diagnostic evaluation of patients with unexplained diarrhea, hematochezia, and abnormal abdominal computed tomographic findings (eg, colonic thickening).
Where are pseudomembrane rods found?
14, 15 This invasive gram-negative rod normally resides in the gastrointestinal tract of cattle, sheep, and other animals and can be pathogenic to people who eat undercooked beef.
Which disease retains the characteristics of inflammatory bowel disease?
In inflammatory bowel disease, even with secondary pseudomembranes, ulcerative colitis and Crohn disease retain the characteristics of inflammatory bowel disease with crypt architectural distortion and focal or diffuse basal lymphoplasmacytosis on microscopy. 48
What is C diff colitis?
What Is Pseudomembranous Colitis (C. diff Colitis)? Pseudomembranous colitis is a type of inflammation in the large intestine (also called the gut or colon). Unlike a similar condition called microscopic colitis, it’s caused by an overgrowth of C. diff ( Clostridium difficile) bacteria . One of the main causes of pseudomembranous colitis is ...
How to prevent pseudomembrane colitis?
To prevent pseudomembranous colitis from recurring, choose foods that benefit your gut bacteria. These include products with probiotics like yogurt (with live active cultures), kefir and sauerkraut.
How Does C. diff Bacteria Get Into the Gut?
While C. diff can occur in the gut naturally, it’s most often spread through contaminated materials in healthcare facilities.
What is the first course of action for pseudomembranous colitis?
When pseudomembranous colitis is diagnosed, generally the first course of action is to stop taking the antibiotics that are suspected of causing the infection. Ironically, pseudomembranous colitis is also treated with antibiotics. Typically, metronidazole is used for mild to moderate symptoms, and vancomycin is used for severe cases.
What is the term for inflammation of the gut that is associated with an overgrowth of C diff bacteria?
Pseudomembranous colitis refers to inflammation in the gut that is associated with an overgrowth of C. diff bacteria.
What antibiotics are used for pseudomembrane colitis?
Summary: Discontinuing the antibiotic that is suspected of leading to the infection is usually the first line of treatment. Metronidazole or vancomycin may then be prescribed. While these antibiotics help most people, some will develop recurring pseudomembranous colitis.
What foods can help with C diff?
Summary: Eat foods that may benefit gut health, including those with probiotics. Early evidence shows kefir in particular may lower the chance of recurring C. diff colitis. Following a Mediterranean diet may also have beneficial effects on gut bacteria.
Who is at greatest risk for pseudomembrane colitis?
People who have the greatest risk for developing pseudomembranous colitis include: Residents of nursing homes. People who have been in the hospital for a long time. People living with another, severe medical condition.
How do you know if you have pseudomembrane colitis?
Symptoms of pseudomembranous colitis include: Frequent watery diarrhea that is sometimes bloody. Pain and tenderness in the stomach. Cramping. Nausea. Fever. Loss of appetite. In more severe cases, sepsis (the body’s potentially dangerous overreaction to an infection) can occur.
What is the medical emergency for pseudomembranous colitis?
In rare cases, pseudomembranous colitis causes toxic megacolon (severe intestinal distention, or swelling), intestinal perforation (puncture) or sepsis. These conditions are medical emergencies that must be treated immediately. Call 911 or go to an emergency room if you have signs of these complications, including:
What is the name of the infection that causes swelling and irritation in the large intestine?
Pseudomembranous colitis is inflammation (swelling, irritation) of the large intestine. In many cases, it occurs after taking antibiotics. Using antibiotics can cause the bacterium Clostridium difficile ( C. diff) to grow and infect the lining of the intestine, which produces the inflammation. Certain antibiotics, like penicillin, clindamycin ...
How long does it take for pseudomembrane colitis to show symptoms?
Most people who have pseudomembranous colitis notice symptoms 5 to 10 days after starting treatment with antibiotics.
How long does it take to cure pseudomembrane colitis?
In most cases, doctors prescribe metronidazole (Flagyl®), vancomycin (Vancocin®) or fidaxomicin (Dificid®) for up to 14 days.
Can C diff cause pseudomembranous colitis?
Some people suffer reinfections with C. diff, which can cause pseudomembranous colitis to recur many times.

Overview
Increase in the number of times a person discharges stool.
Symptoms
Causes
Risk Factors
Complications
- Some people carry C. difficile bacteria in their intestines but never become sick. These individuals are carriers of the bacteria and may spread infections. Signs and symptoms usually develop within 5 to 10 days after starting a course of antibiotics. However, they may occur as soon as the first day or up to three months later.
Prevention
- C. difficile bacteria enter the body through the mouth. They can begin reproducing in the small intestine. When they reach the large intestine (colon), they can release tissue-damaging toxins. These toxins destroy cells, produce patches of inflammatory cells and cellular debris, and cause watery diarrhea. When the bacteria are outside the colon — virtually anywhere in the environmen…