Full Answer
How dangerous is pyelonephritis?
Pyelonephritis is an infection, however, and this infection can spread and become very severe. Complications of untreated or poorly controlled pyelonephritis can be serious, even life threatening in some cases.
How serious is pyelonephritis?
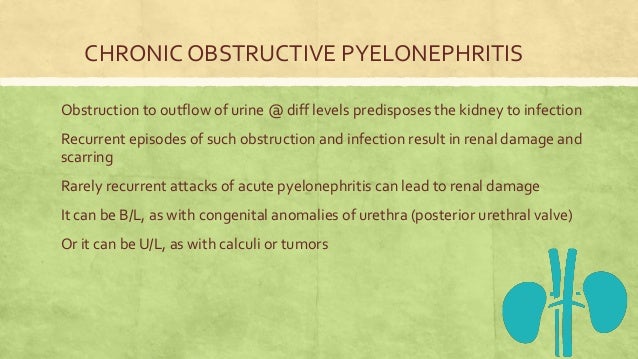
Rarely, pyelonephritis can develop into a serious infection that threatens the afflicted kidney, and possibly the patient’s life. Severe or untreated pyelonephritis may cause permanent kidney scars, which can lead to chronic kidney disease, high blood pressure, and kidney failure. What Causes Pyelonephritis?
What are possible complications of pyelonephritis?
What Are The Complications Of Pyelonephritis?
- recurrent kidney infections
- Spread of infection to surrounding tissues
- acute kidney failure
- kidney abscess
- Hypertension
How to treat hydronephrosis with home remedies?
Some home remedies that can help along with the hydronephrosis ayurvedic treatment are:
- Mix two spoons of olive oil and lemon juice and take it along with a glass of water. ...
- Taking radish leaves juice will also help remove a kidney stone from the body.
- Consume lots of water, and other fluids as this will pass stone from your kidney easily without any side effects.
- Tomato juice with a pinch of salt and pepper early in the morning.
What is pyelonephritis with hydronephrosis?
Pyonephrosis—pus in the renal pelvis—results from urinary tract obstruction in the presence of pyelonephritis. Purulent exudate (inflammatory cells, infectious organisms, and necrotic, sloughed urothelium) collects in the hydronephrotic collecting system ("pus under pressure") and forms an abscess.
What infection causes hydronephrosis?
Hydronephrosis is a condition of the urinary tract where one or both kidneys swell. This happens because urine does not fully empty from the body. Symptoms may include sudden or intense pain in the back or side, vomiting, painful urination, blood in the urine, weakness and fever due to a urinary tract infection.
What is the main cause of hydronephrosis?
Hydronephrosis is usually caused by a blockage in the urinary tract or something disrupting the normal workings of the urinary tract. The urinary tract is made up of the kidneys, the bladder, the ureters (the tubes that run from the kidney to the bladder) and the urethra (the tube that carries urine out of the body).
What can pyelonephritis lead to?
A kidney infection is also called pyelonephritis. A kidney infection needs prompt medical treatment. If not treated properly, an infection can cause lasting damage to the kidneys. Or the bacteria can spread to the bloodstream and cause a dangerous infection.
Can a kidney infection cause hydronephrosis?
The doctor can also check for blood in the urine, which can be caused by a kidney stone, infection or other factor. How is Hydronephrosis Treated? Hydronephrosis is usually treated by addressing the underlying disease or cause, such as a kidney stone or infection. Some cases can be resolved without surgery.
What will a urologist do for hydronephrosis?
In cases of severe blockage and hydronephrosis, your doctor might need to do one of the following: Insert a ureteral stent, a tube that allows the ureter to drain into the bladder. Insert a nephrostomy tube, which allows the blocked urine to drain from the kidney. Prescribe antibiotics to control infection.
What are the stages of hydronephrosis?
Hydronephrosis can vary in severity. Typically, your doctor will describe your child's hydronephrosis as mild, moderate or severe. Sometimes hydronephrosis is given a grade of 1, 2, 3 or 4, with 1 representing very minimal dilation and 4 representing severe dilation.
Can recurrent UTI cause hydronephrosis?
Sometimes the pee backs up to the kidneys. If it's infected with bacteria, it can lead to pyelonephritis. hydronephrosis, which is an enlargement of one or both kidneys due to backup or blockage of urine flow.
Can a kidney recovery from hydronephrosis?
This study suggests that the period required for maximum recovery from hydronephrosis is usually constant, unless the obstruction is too mild to cause any damage or too long to permit any recovery.
What is the most serious complication of pyelonephritis?
Acute pyelonephritis can have several complications, such as renal or perinephric abscess formation, sepsis, renal vein thrombosis, papillary necrosis, or acute renal failure, with one of the more serious complications being emphysematous pyelonephritis.
What are the classic signs of pyelonephritis?
The classic presentation in acute pyelonephritis is the triad of fever, costovertebral angle pain, and nausea and/or vomiting. These may not all be present, however, or they may not occur together temporally. Symptoms may be minimal to severe and usually develop over hours or over the course of a day.
What part of the kidney is affected by pyelonephritis?
In acute pyelonephritis the lining of the renal structures into which urine drains, the renal pelvis and the calyces, may be inflamed. Abscesses may form in the kidney tissue, and some of the nephron tubules (urine-producing structures) may be destroyed.
Who is most likely to get hydronephrosis?
These groups include:pregnant women, due to an enlarging womb that may compress the ureters.men over the age of 50, due to enlargement of the prostate or prostate cancer.sexually active women, due to their risk for recurrent urinary tract infections.people who are predisposed to recurrent kidney stones.
Can hydronephrosis lead to sepsis?
Obstructive uropathy is one of the leading causes of urosepsis. In patients with severe hydronephrosis, underlying sepsis and renal dysfunction should be treated with caution. The immediate drainage of hydronephrosis is crucial for infectious source removal and is hence related to the patient's prognosis.
Does hydronephrosis mean kidney disease?
Hydronephrosis (kidney swelling) occurs as the result of a disease. It is not a disease itself. Conditions that may lead to hydronephrosis include: Blockage of a ureter due to scarring caused by prior infections, surgeries, or radiation treatments.
What can mimic hydronephrosis?
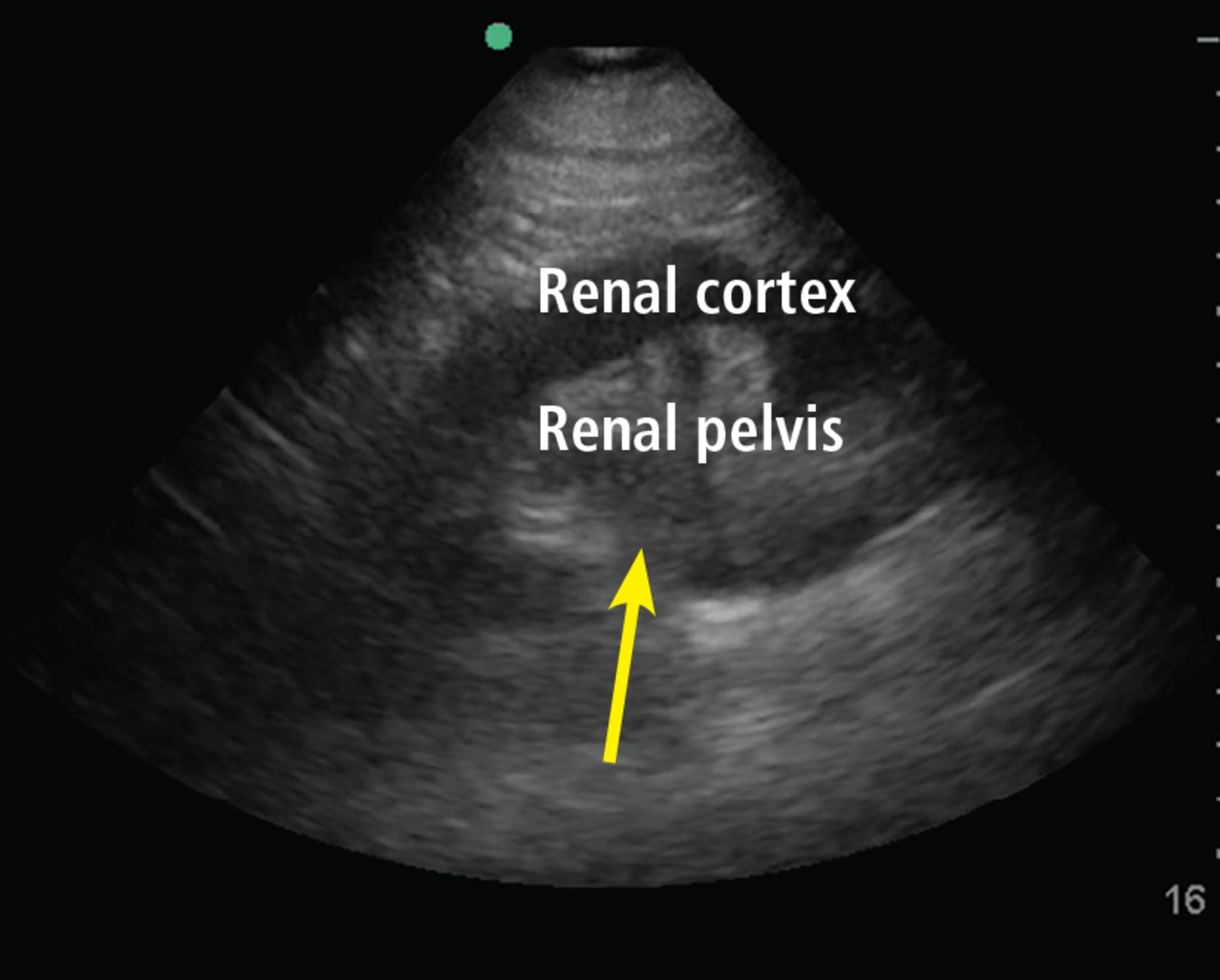
Parapelvic cysts also can mimic hydronephrosis because of their anechoic nature (like urine, clear fluid in the cysts is black on ultrasound) and close proximity to the collecting system.
Can hydronephrosis cause pylonephritis?
Related: If a kidney is obstructed, it can dilate ( hydronephrosis ). The blockage causes the urine flow to decrease, making infection possible ( pyelonephritis ). This is a common risk with obstructing kidney stones.
Causes of hydronephrosis?
Several: Blockage in the ureter, bladder neck or urethra. This can be internal, external or within the walls of these organs.There are several causes.
What are the complications of acute pyelonephritis?
Acute pyelonephritis can have several complications such as renal or perinephric abscess formation, sepsis, renal vein thrombosis, papillary necrosis, or acute renal failure, with one of the more serious complications being emphysematous pyelonephritis (EPN).[4] Emphysematous pyelonephritis is a necrotizing infection of the kidney usually caused by E. colior Klebsiella pneumoniae and is a severe complication of acute pyelonephritis. EPN is usually seen in the setting of diabetes and occurs more frequently in women. The diagnosis can be made with ultrasound, but CT is typically necessary. Overall the mortality rate is estimated to be approximately 38% with better outcomes associated with patients who receive both medical and surgical management versus medical management alone. [5]
How to diagnose acute pyelonephritis?
A good history and physical is the mainstay of evaluating acute pyelonephritis, but laboratory and imaging studies can be helpful. A urinary specimen should be obtained for a urinalysis. On urinalysis, one should look for pyuria as it the most common finding in patients with acute pyelonephritis. Nitrite production will indicate that the causative bacteria is E.coli. Proteinuria and microscopic hematuria may be present as well on urinalysis. If hematuria is present, then other causes may be considered such as kidney stones. All patients with suspected acute pyelonephritis should also have urine cultures sent for proper antibiotic management. Blood work such as a complete blood cell count (CBC) is sent to look for an elevation in white blood cells. The complete metabolic panel can be used to search for aberrations in creatinine and BUN to assess kidney function. The imagining study of choice for acute pyelonephritis is abdominal/pelvic CT with contrast. Imaging studies will usually not be required for the diagnosis of acute pyelonephritis but are indicated for patients with a renal transplant, patients in septic shock, those patients with poorly controlled diabetes, complicated UTIs, immunocompromised patients, or those with toxicity persisting for longer than 72 hours. Ultrasonography can be used to detect pyelonephritis, but a negative study does not exclude acute pyelonephritis. Regardless, ultrasound can still be a useful study when evaluating for acute pyelonephritis because it can be done bedside, has no radiation exposure and may reveal renal abnormalities, which can prompt further testing or definitive treatment.
What is the most common disease of the kidneys?
Acute pyelonephritis is a bacterial infection causing inflammation of the kidneys and is one of the most common diseases of the kidney. Pyelonephritis occurs as a complication of an ascending urinary tract infection (UTI) which spreads from the bladder to the kidneys and their collecting systems. Symptoms usually include fever, flank pain, nausea, vomiting, burning on urination, increased frequency, and urgency. The 2 most common symptoms are usually fever and flank pain. Acute pyelonephritis can be divided into uncomplicated and complicated. Complicated pyelonephritis includes pregnant patients, patients with uncontrolled diabetes, kidney transplants, urinary anatomical abnormalities, acute or chronic kidney failure, as well as immunocompromised patients and those with hospital-acquired bacterial infections. It is important to make a distinction between complicated and uncomplicated pyelonephritis, as patient management and disposition depend on it.
What is the bacterial infection that causes a burning sensation in the kidneys?
Acute pyelonephritis is a bacterial infection causing inflammation of the kidneys. Pyelonephritis occurs as a complication of an ascending urinary tract infection which spreads from the bladder to the kidneys. Symptoms usually include fever, flank pain, nausea, vomiting, burning with urination, increased frequency, and urgency. This activity outlines the clinical presentation, diagnosis, and management of acute pyelonephritis , and highlights the role of the interprofessional team in caring for patient with the condition.
How is pyelonephritis treated?
Overall the majority of cases of pyelonephritis are managed in an outpatient setting with most patients improving with oral antibiotics. Usually, young women are among those most likely to be treated as outpatients.[1] Despite pyelonephritis improving in most cases, there is still significant morbidity and mortality that can be associated with severe cases of this disease. Overall mortality has been reported around 10% to 20% in some studies with a recent study from Hong Kong finding a mortality rate closer to 7.4%. More importantly, this study found that old age (older than 65 years), male gender, impaired renal function, or presence of disseminated intravascular coagulation were associated with increased mortality. With the proper recognition of the underlying etiology and prompt intervention with adequate treatment, even patients with severe pyelonephritis generally have a good outcome. [3]
What is the most common bacterial infection that causes pyelonephritis?
E. coliis the most common bacteria causing acute pyelonephritis due to its unique ability to adhere to and colonize the urinary tract and kidneys. E.colihas adhesive molecules called P-fimbriae which interact with receptors on the surface of uroepithelial cells. Kidneys infected with E. colican lead to an acute inflammatory response which can cause scarring of the renal parenchyma. Though the mechanism in which renal scarring occurs is still poorly understood, it has been hypothesized that the adhesion of bacteria to the renal cells disrupts the protective barriers, which lead to localized infection, hypoxia, ischemia, and clotting in an attempt to contain the infection. Inflammatory cytokines, bacterial toxins, and other reactive processes further lead to complete pyelonephritis and in many cases systemic symptoms of sepsis and shock.
When diagnosing acute pyelonephritis, keeping the differential broad is a wise idea?
When diagnosing acute pyelonephritis, keeping the differential broad is a wise idea. Physicians should consider other disorders as well when patients present with fever, flank pain, and costovertebral angle tenderness. Because symptoms can be variable (unilateral, bilateral, radiating, sharp, dull) and because pyelonephritis can progress to sepsis and shock the differential diagnoses associated with pyelonephritis can be extensive. Common mimics of acute pyelonephritis can include but is not limited to:
What is the tube that drains urine from the kidney?
If the hydronephrosis is acute or sudden, a stent or soft tube (nephrostomy tube) may be inserted through the skin into the kidney to drain off excess urine. A soft plastic tube called a ureteral stent may be placed between the kidney and bladder by a urologist during a cystoscopy to drain excess fluids.
What causes hydronephrosis in adults?
In adults, the conditions that most often cause hydronephrosis include: Kidney stones: Stones that may become lodged in the kidneys or urinary tract. Cancer: Tumors in the bladder, prostate gland, uterus or other organs that are part of or near the urinary tract may cause blockages that disrupt the flow of urine.
Why do my kidneys swell?
Hydronephrosis is a condition in which one or both kidneys become swollen due to incomplete emptying of the urinary tract. It can be sudden or chronic, partial or complete, one-sided or bilateral. It can occur anywhere along the urinary tract from the opening of the kidneys to the ureters (draining the kidneys to the bladder), the bladder, and the urethra (draining the bladder). Problems with any of these structures may cause impaired emptying of the urinary system and back up of fluid and pressure.
Why is urine held inside the body?
Urinary retention: Urine may be held inside the body due to an inability to empty the bladder. Vesicoureteral reflux: This is a condition when urine flows backward from the bladder to the kidneys. Uterocele: This is a condition where the lower part of the ureter may protrude into the bladder.
Why does hydronephrosis occur?
In women, hydronephrosis may occur as a result of: Pregnancy: As the uterus expands, it can press on the ureters and block the flow of urine. Uterine prolapse: A condition in which a woman's uterus (womb) sags or slips out of its normal position.
Why is my urinary tract narrowing?
Narrowing or stricture of the urinary tract: This narrowing can be due to injury, infection, birth defects or surgery. Nerve or muscle problems: These problems can affect the kidneys or ureters, such as from diabetes mellitus. Urinary retention: Urine may be held inside the body due to an inability to empty the bladder.
What is it called when both kidneys are affected?
If only one of the kidneys is affected, the condition is called unilateral hydronephrosis. If both kidneys are affected, it is called bilateral hydronephrosis.
What causes a newborn to have a ureteropelvic junction obstruction?
Yearly, of the estimated 6% total new births worldwide (8 million) born with serious birth defects, as many as 1% of the newborns have congenital defects of kidney and urinary tract.[1] Hydronephrosis is present in a growing number of neonates and infants, most commonly due to ureteropelvic junction obstruction. This is found in up to 1 in 100 live births in the United States and is treated conservatively. In the majority of cases, spontaneous resolution is found by 2 years of age. Less commonly found is vesicoureteral reflux, which accounts for 10%-20% of neonatal and infantile hydronephrosis. Obstruction of ureterovesical junction, posterior urethral valves, and stricture are the other common anatomical abnormalities.
What is the function of the urinary system?
The urinary system is a complex, multi-component organ system that has the primary function of maintaining body homeostasis by regulating the volume of body fluid, electrolyte balance, and excretion of metabolic end products through a final product called urine. Anatomically it includes the kidneys, ureters, urinary bladder, and urethra. Each kidney has an outer cortex and an inner medulla, which is formed into renal pyramids that extend into the renal pelvis, which is continued as the ureter. Hydronephrosis and hydroureter can present independently or together. They occur in all age groups. The presentation can be acute or chronic, physiologic (very common in pregnant females) or pathologic, unilateral, or bilateral.
Why is a catheter placed in the bladder?
Placement of a urinary catheter is important when lower urinary tract obstruction at the bladder level is highly suspected. Cystoscopy guided ureteral stent placement is a common procedure for various intrinsic and extrinsic causes of hydronephrosis at the ureter level. Fluoroscopy guided percutaneous nephrostomy tube placement is a less invasive procedure performed by interventional radiologists when ureteral stent placement is contraindicated or cannot be done.
What is the cause of hydroureteronephrosis?
Hydronephrosis and hydroureter result from obstruction of urine flow in the urinary system at the renal pelvis and ureter level , respectively. This is common in all age groups, from newborns to elderly patients. Both conditions should be promptly diagnosed and treated to prevent severe renal dysfunction. This activity reviews the etiology, epidemiology, and diagnosis of hydroureteronephrosis and highlights the role of prompt management for timely prevention of renal dysfunction.
How long does hydronephrosis last?
It is mostly identified in the second trimester and may persist up to 6 to 12 weeks postpartum. Ureteral stenting is a treatment of choice if patients develop pain and renal failure. [3]
What is the term for dilation of the ureter due to obstruction of urine outflow?
Dilation of the ureter due to obstruction of urine outflow is called hydroureter.
Why do infants with hydroureteronephrosis need a voiding cystourethrogram?
Infants with congenital hydroureteronephrosis should undergo a voiding cystourethrogram to identify patients with vesicoureteral reflux.[7] When presenting with fever, abdominal pain, nausea, or decreased oral intake, a urinalysis should be obtained as these patients are predisposed to urinary tract infections (UTIs). A basic metabolic panel should be ordered to establish a baseline renal function which can be followed to indicate the resolution of hydronephrosis as well as indicate surgical management in patients with worsening renal function.
