Patients with HIT may safely receive enoxaparin if their plasma does not aggregate platelets in the presence of enoxaparin. Thirty-four percent of plasma samples from patients with HIT (88% of those strongly positive) aggregated platelets in the presence of enoxaparin.
When is enoxaparin used in the treatment of heparin-induced thrombocytopenia syndrome (hit)?
Patients with HIT may safely receive enoxaparin if their plasma does not aggregate platelets in the presence of enoxaparin. Use of enoxaparin in patients with heparin-induced thrombocytopenia syndrome
Does enoxaparin interact with platelets in patients with hit?
Patients with HIT may safely receive enoxaparin if their plasma does not aggregate platelets in the presence of enoxaparin. Thirty-four percent of plasma samples from patients with HIT (88% of those strongly positive) aggregated platelets in the presence of enoxaparin.
What are the contraindications for enoxaparin?
If renal function is compromised, the clearance of enoxaparin will be delayed, and the risk of bleeding will increase. 3 • If platelet count is < 50×109/L, enoxaparin is contraindicated3 • If there is a decrease of 30-50% from baseline during treatment, enoxaparin should be discontinued immediately and HIT considered.
Should non-heparin anticoagulants be used for postoperative heparin treatment?
Non-heparin anticoagulants should be chosen for postoperative anticoagulation in surgical patients. Using full courses of heparin puts patients at risk for typical-onset HIT recurrence. Development of any new/ unexplained platelet drop 5-10 days after heparin exposure should trigger a concern for delayed-onset HIT, ...
What anticoagulant can be used with HIT?
A direct thrombin inhibitor, such as lepirudin, danaparoid or argatroban, is considered the agent of choice for treatment of HIT.
Can you use heparin after HIT?
Full courses of heparin should be avoided in patients with a history of HIT. Patients with a history of HIT are more likely to develop platelet-activating antibodies (SRA seroconversion) within their anti-PF4/heparin response and thus to develop HIT if they receive postoperative heparin.
Which heparin is more likely to cause a HIT?
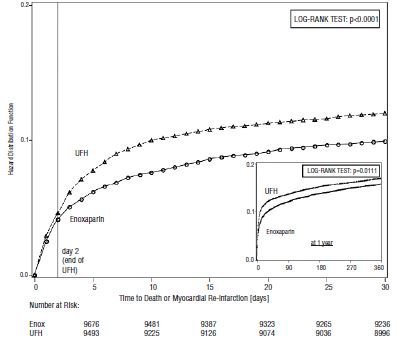
Heparin-induced thrombocytopenia (HIT) is caused by antibodies that bind to complexes of heparin and platelet factor 4 (PF4), activating the platelets and promoting a prothrombotic state. HIT is more frequently encountered with unfractionated heparin (UFH) than with low molecular weight heparin (LMWH).
Which is better enoxaparin or heparin?
New study shows LOVENOX® (enoxaparin sodium injection) is more effective than unfractionated heparin (UFH) for lowering the risk of venous thromboembolism (VTE) in patients with acute ischemic stroke.
Can you use Lovenox with history of HIT?
Conclusions: Thirty-four percent of plasma samples from patients with HIT (88% of those strongly positive) aggregated platelets in the presence of enoxaparin. Patients with HIT may safely receive enoxaparin if their plasma does not aggregate platelets in the presence of enoxaparin.
Does LMWH cause HIT?
Heparin-induced thrombocytopenia (HIT) is an uncommon but potentially devastating complication of anticoagulation with unfractionated heparin (UFH) or low-molecular-weight heparin (LMWH).
Can you get HIT from subcutaneous heparin?
Even low-dose subcutaneous UFH has been reported to cause HIT in about 1% of such patients. Low-molecular-weight heparin (LMWH) probably reduces risk of HIT in these patients (although this remains unproved).
Can enoxaparin cause low platelets?
Tell your doctor if you have any of these symptoms. Low platelets: In rare cases, this drug may lower your platelets. Platelets are needed for your blood to clot. This increases your risk of bleeding even more.
Can heparin flush cause HIT?
Sometimes, heparin causes severe complications such as heparin-induced thrombocytopenia (HIT), which result in not only thrombocytopenia but also arterial/venous thrombosis.
Why is enoxaparin preferred over heparin?
In comparison with unfractionated heparin, enoxaparin has been shown to be more stable and have more predictable pharmacokinetics,1 providing an optimal level of anticoagulation at the time of the procedure in more than 90% of patients, by whatever route the drug is administered.
Can you give heparin and enoxaparin together?
heparin enoxaparin Using heparin together with enoxaparin may increase the risk of bleeding, including severe and sometimes fatal hemorrhage.
Why would you use heparin instead of enoxaparin?
Results found that, compared to heparin, enoxaparin significantly reduced blood clots without increasing the risk of major bleeding. One caveat to using Lovenox is that its dosage needs to be adjusted in patients with renal failure. Otherwise, there is an increased risk of bleeding.
When do you not give heparin?
A patient should not receive heparin if[5]: The platelet count is 100,000/mm or lower. The patient cannot have routine monitoring tests performed to monitor therapeutic heparin. The patient has an active, uncontrollable bleed except for disseminated intravascular coagulation (DIC).
Does HIT cause bleeding or clotting?
But with heparin-induced thrombocytopenia (HIT), your body reacts to heparin in a way that may cause clots instead of preventing them. Thrombocytopenia means you have a low level of platelets, which are blood cells that help your blood clot. Usually, low platelets would cause you to bleed.
How do you treat heparin bruises?
Accordingly, clinical nurses are suggested to use cold packs to reduce the occurrence and size of bruising associated with subcutaneous heparin injection.
How does heparin cause HIT?
Heparin-induced thrombocytopenia (HIT) occurs when a patient receives heparin, a blood-thinning medication, and subsequently forms antibodies against heparin and the platelet factor-4 (PF4) complex.
What happens if you stop heparin after a HIT?
Because HIT causes a hypercoagulable state, venous and/or arterial thrombosis can occur. The most common complications are deep venous thrombosis (DVT), pulmonary embolism (PE), or skin necrosis. The latter is particularly a risk if warfarin is administered in the acute phase. The risk of these complications is highest within the first 10 days, but the pro-thrombotic state persists up to 30 days after stopping heparin. [7]
What is a heparin induced thrombocytopenia?
Heparin-induced thrombocytopenia (HIT) is a severe complication that can occur in patients exposed to any form or amount of heparin products.[1] A fall in platelet counts and a hypercoagulable state characterize HIT. Patients who experience HIT may also develop thromboembolic complications that are associated with morbidity and mortality. This is a significant burden since heparin is widely used for treatment and prophylaxis of thromboembolism, line flushes, and heparin-coated catheters. This review will discuss the pathophysiology, diagnosis, and management of patients with HIT.
What happens when PF4 is attached to heparin?
HIT can only occur if IgG, while attached to the heparin-PF4 complex, binds to the FC receptor on the platelet surface and leads to platelet activation. Activated platelets then release pro-thrombotic substances (such as thrombin) and PF4. As IgG activates more platelets, more PF4 is released forming more complexes with heparin, thus activating more platelets. This creates a severely hypercoagulable state and a continuous cycle that can only be broken when heparin is discontinued, and appropriate treatment is initiated.
How long does it take for a type 2 heparin reaction to occur?
Type II HIT is an immune, antibody-mediated reaction. Because it takes time for the antibodies to form, this reaction usually occurs after 5 to 14 days of receiving heparin. However, if a patient has been exposed to heparin within the last 100 days, antibodies may remain in the system, causing this reaction to manifest as soon as day one of re-exposure to heparin. This is a very serious reaction that causes a hypercoagulable state and can lead to life-threatening complications. The rest of this review will focus on type II HIT and its management.
When should a patient be suspected of a HIT?
HIT should be suspected when there is an unexplained drop in platelet counts in a patient currently on heparin or recently exposed to heparin products. HIT typically presents as a steady drop in platelet counts (no fluctuations), while hemoglobin and hematocrit counts remain relatively stable. [10][11][12]
Does Fondaparinux cause HIT?
Fondaparinux is a heparin-like drug that does not cause HIT, nor does it react with heparin-induced antibodies. UFH is a heterogeneous product that consists of long saccharide chains of varying lengths and molecular weights; the average UFH molecule is 45 saccharide units long. LMWH is also a heterogeneous product; however, LMWH is, on average, 15 saccharide units long. Fondaparinux is a synthetic pentasaccharide consisting of only the 5 sugars. The shorter the saccharide chain and the smaller the molecular weight, the less likely the drug is to bind to plasma proteins and cells. Therefore, there is a reduced risk of a HIT with LMWH compared to UFH, whereas fondaparin ux does not cause HIT and can be safely utilized in patients with a history of HIT and potentially in the treatment of acute HIT.
Is heparin a mediated reaction?
Type I HIT, also known as heparin-associated thrombocytopenia (HAT), is a non-immune mediated reaction. Type I HIT is much more common than type II and can occur as early as day 1 of therapy. This is a mild reaction, it is not associated with any complications, and platelet counts will spontaneously normalize even if heparin is continued.
What is unfractionated heparin?
Unfractionated heparin (UFH) is the clear anticoagulant of choice in 3 conditions — cardiac surgery, vascular surgery, and hemodialysis.
What is a heparin induced thrombocytopenia?
Heparin-induced thrombocytopenia (HIT) is an immune-mediated reaction occurring in 0.2-5% of adults treated with heparin causing a ≥50% drop in platelets from baseline. Patients with HIT have a high risk of thrombosis, which can lead to serious complications including limb loss and death. HIT occurs when heparin binds to platelet factor-4 (PF4), ...
How long does it take for a heparin to react with a PF4?
This serious reaction typically develops 5-10 days after heparin exposure, ...
How long does it take for platelets to drop after heparin?
Development of any new/ unexplained platelet drop 5-10 days after heparin exposure should trigger a concern for delayed-onset HIT, a subtype of HIT that develops 5+ days after heparin therapy has been discontinued.5 Delayed-onset HIT occurs when IgG antibodies activate platelets even in the absence of heparin.
Does heparin cause a rapid immune response?
In fact, any immunizing exposure to heparin, whether first or subsequent re-exposure, leads to a relatively rapid immune response (~5 days). This means that heparin re-challenge despite prior HIT often induces anti-PF4/heparin antibodies, but no faster than seen with typical HIT. It is believed that all cases of HIT likely represent a type of “secondary” immune response. Although the reason for this is unknown, one hypothesis is that “primary” immunization occurs from exposure to PF4-coated bacteria. 2,3,4
Can you take heparin with a positive SRA?
Key Recommendations. Heparin use should be avoided in patients with a positive SRA.5 Using heparin in patients with a positive SRA puts them at risk for rapid-onset HIT, a subtype of HIT occurring within 24 hours in patients exposed to heparin within the past 30 days.
What is heparin induced thrombocytopenia?
Heparin-induced thrombocytopenia (HIT) is a life-threatening complication of exposure to heparin (ie, unfractionated heparin, low molecular weight [LMW] heparin) that occurs in up to 5 percent of patients exposed, regardless of the dose, schedule, or route of administration. HIT results from an autoantibody directed against platelet factor 4 (PF4) in complex with heparin (referred to as a HIT antibody). HIT antibodies activate platelets and can cause catastrophic arterial and venous thrombosis, with a mortality rate as high as 20 percent, although with improved recognition and early intervention, mortality rates below 2 percent have been reported.
What is HIT algorithm 1?
Overview of initial management — HIT requires immediate treatment to reduce the risk of potentially life-threatening thrombosis ( algorithm 1 ). In most cases, treatment must be initiated based on a strong clinical suspicion of HIT, even before confirmatory laboratory test results are available.
Is Fondaparinux an anticoagulant?
Gerhardt A, Zotz RB, Stockschlaeder M, Scharf RE. Fondaparinux is an effective alternative anticoagulant in pregnant women with high risk of venous thromboembolism and intolerance to low-molecular-weight heparins and heparinoids. Thromb Haemost 2007; 97:496.
How long to take fondaparinux with warfarin?
Orally as tablet. Avoid unopposed use for first 3 to 5 days until INR is at target value. The DTI or fondaparinux is overlapped with warfarin for about 5 days, until a target value is achieved on a blood test (known as international normalized ratio, or INR) that measures the level of anticoagulation from warfarin.
What are the signs of heparin injections?
Severe indicators of HIT are skin changes that present as bruising or blackening around the heparin injection site as well as the fingers, toes, and nipples that may progress to gangrene. The extremities are especially susceptible to the small clots that form because of HIT.
What Is Heparin-Induced Thrombocytopenia?
Triggered by the immune system in response to heparin, HIT causes a low platelet count (thrombocytopenia).
How Is HIT Diagnosed?
HIT can often be diagnosed by measuring the platelet count and PF4 antibody level in the blood. Symptoms of new blood clot formation may suggest HIT.
What if I Need Anticoagulants in the Future?
Although HIT is caused by a reaction to heparin that is similar to other allergic reactions, it is not a true allergy. In contrast to many allergies to other medications or foods, the allergy to heparin is not long-lasting. The PF4 antibody that causes HIT will usually disappear after approximately 3 months. Thereafter, heparin may be considered for use if a new clot did not develop from HIT and if the PF4 antibody test is negative.
What is a direct thrombin inhibitor?
Direct thrombin inhibitors (DTI) are a class of anticoagulant medications that do not cause HIT. These drugs are administered by continuous intravenous infusion. Three DTIs have been approved by the Food and Drug Administration: lepirudin, argatroban, and bivalirudin. You may also be treated with another class of injectable anticoagulant medication called fondaparinux instead of a DTI ( Table ). After several days, your blood will be tested to make sure that the platelet count has returned to normal. At that point, the oral blood thinner warfarin (commonly called by its trade name, Coumadin) may be prescribed in addition to the fondaparinux or DTI.
What is the most commonly used intravenous anticoagulant?
The most commonly used intravenous anticoagulant is heparin . This Cardiology Patient Page focuses on heparin- induced thrombocytopenia (HIT), a complication of heparin therapy. This complication of heparin is often confusing because in HIT, heparin does the opposite of what it is supposed to do: It forms rather than prevents new blood clots.
Why is enoxaparin used?
Enoxaparin is used to thin your blood. It keeps your blood from forming clots. Blood clots are dangerous because they can lead to serious blockages in your blood vessels. This can cause a stroke or a heart attack.
How does enoxaparin work?
Enoxaparin works by blocking a protein in your body that causes clotting. This keeps blood clots from forming. If you have a blood clot, it will stop it from getting worse while your body breaks down the clot on its own.
How to store enoxaparin?
Store enoxaparin at room temperature. Keep it at 77°F (25°C). Keep it away from light. Don’t store this medication in moist or damp areas, such as bathrooms.
How often is a 30 mg injection given?
Typical dosage is a one-time intravenous (into the vein) injection of 30 mg given in the hospital, plus a 1-mg/kg injection under the skin. Then, 1 mg per kg of body weight will be injected every 12 hours. This will be given by a healthcare provider in the hospital.
Where is enoxaparin injected?
Enoxaparin is injected subcutaneously (under your skin ). Your healthcare provider will show you how to give this drug to yourself.
How to avoid interactions with medications?
To help avoid interactions, your doctor should manage all of your medications carefully. Be sure to tell your doctor about all medications, vitamins, or herbs you’re taking. To find out how this drug might interact with something else you’re taking, talk to your doctor or pharmacist.
What to do if you have serious side effects?
Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life-threatening or if you think you’re having a medical emergency. Serious side effects and their symptoms can include the following:
