
Can I use red ink on a CMS-1500 claim form?
Follow these guidelines on ink color: Submit the scannable, red-ink version of the CMS-1500 claim form. Do not use red ink to complete a CMS-1500 claim form. OCR scanners "drop out" any red that is on the paper. Use true black ink.
Can I use a copy of the CMS-1500 form?
The only acceptable claim forms are those printed in Flint OCR Red, J6983, (or exact match) ink. Although a copy of the CMS-1500 form can be downloaded, copies of the form cannot be used for submission of claims, since your copy may not accurately replicate the scale and OCR color of the form.
Who is responsible for the design and maintenance of the CMS-1500?
The National Uniform Claim Committee (NUCC) is responsible for the design and maintenance of the CMS-1500 form. CMS does not supply the form to providers for claim submission.
How do physician's get paid for CMS-1500 claims?
Physicians can submit the CMS-1500 form electronically, although paper claims are still in use. The payment will depend on different factors, including the patient's condition, the network status between the client and the patient and any previous settings.
What color is the CMS 1500 form?
Each of the vendors above sells the CMS-1500 claim form in its various configurations (single part, multi-part, continuous feed, laser, etc). The only acceptable claim forms are those printed in Flint OCR Red, J6983, (or exact match) ink.
Why is the CMS 1500 form red?
In 1990, the CMS-1500 changed the form to red ink print to promote the scanning of claims. Later, further changes were made in order to accommodate the National Provider Identifier (NPI).
What color ink must be used on CMS 1500 claims form in order for an OCR software to convert characters to text?
Follow these guidelines on ink color: Submit the scannable, red-ink version of the current HCFA CMS-1500 (02/12) or current UB-04 CMS-1450 claim forms. Do not use red ink to complete a claim form. OCR scanners "drop out" any red that is on the paper.
Can I hand write on CMS 1500 form?
Can CMS 1500 forms be hand written? Yes, in many instances, the CMS 1500 form can be handwritten.
Can Dirty claims be resubmitted?
Dirty claims cannot be resubmitted. Electronic claims are submitted via electronic media. Claims that are done by direct billing first go to a clearinghouse. Insurance information should be collected on the first visit.
What is the difference between HCFA 1500 and CMS 1500?
The HCFA 1500 claim form, also known as CMS-1500, enables medical physicians to submit health insurance claims for reimbursement from various government insurance plans including Medicare, Medicaid and Tricare.
How do I print on CMS 1500 form?
InformationNavigate to the. Claims module and select Claims Manager.Select the claims to be exported. Click the Actions. drop-down and select Export/Download.Select CMS 1500 (PDF) from the drop-down and click Export.
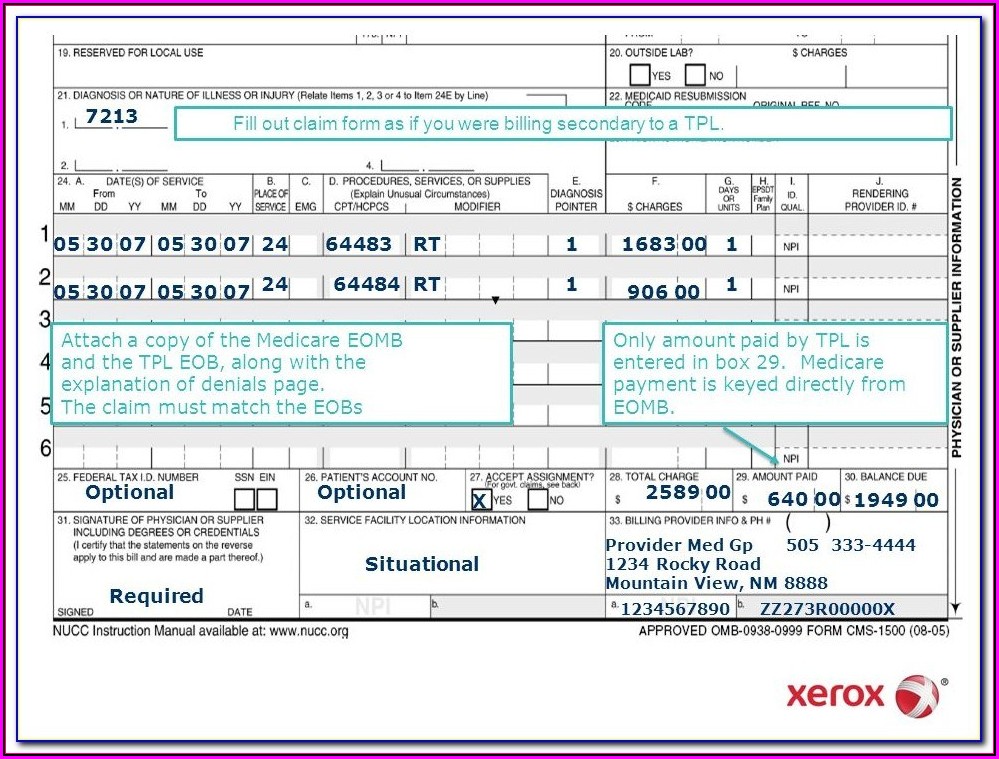
How do I fill out a CMS 1500 form?
1:4719:58How-to Accurately Fill Out the CMS 1500 Form for Faster PaymentYouTubeStart of suggested clipEnd of suggested clipCompany in the top right hand corner of the form. Although. You may be submitting the formMoreCompany in the top right hand corner of the form. Although. You may be submitting the form electronically. The name and address of the insurance carrier must be included in this space on the form.
What is Field 11 in CMS 1500 claim form?
The street address, area, state, ZIP code, and telephone number are included. Box 11: This field requires the insured's policy or group number to be filled.
Does Medicare accept handwritten claims?
Medicare to Reject Handwritten Claims. Providers who wish to continue to submit paper claims may do so as long as they are printed and as long as the only handwriting included in the claim is in a signature field. Software programs are available that will allow providers to print information into a CMS 1500 form.
Can you submit Medicare claims on paper?
The Administrative Simplification Compliance Act (ASCA) requires that Medicare claims be sent electronically unless certain exceptions are met. Providers meeting an ASCA exception may send their claims to Medicare on a paper claim form.
What goes in box 19 on a CMS 1500?
Services rendered to an infant may be billed with the mother's ID for the month of birth and the month after only. Enter “Newborn using Mother's ID”/ “(twin a) or (twin b)” in the Reserved for Local Use field (Box 19). 3 Required Patient's Birth date - Enter member's date of birth and check the box for male or female.
What are three common errors that delay CMS-1500 claims processing?
Most Common Mistakes in CMS-1500 FormMistake 1: Using an Outdated Form. ... Mistake 2: Not Using Diagnosis Code to Highest Level of Specificity. ... Mistake 3: Using Inaccurate CPT Code. ... Mistake 4: Misusing CPT Codes. ... Mistake 5: Claim Wasn't Filed on Time. ... Mistake 6: Patient Information is Missing.More items...
What was the CMS-1500 form previously called?
The HCFA-1500 became known as the CMS-1500, when the HCFA was re-titled as re-titled the Centers for Medicare and Medicaid Services (CMS). CSM-1500 (12-90) form changed so that it could accommodate reporting of the National Provider Identifier ( NPI) for providers; this form was referred to as the CMS-1500 (08-05).
What is a CMS-1500 form quizlet?
CMS-1500. Claim form used to submit paper claims fo services and procedures rendered by physicians and other health care professional on an outpatient basis. Continuity of care. Coordinating treatment and health services between patients' health care providers.
What is Block 12 on the CMS-1500 form?
What is it? Box 12 indicates the client authorizes the release of any medical information needed to process and/or adjudicate the claim. This can be done by entering "Signature on File", "SOF", or by using an actual signature.
How should the 1500 form be centered?
Information should be centered horizontally and vertically within the confines of each item box on the 1500 form. All information should be aligned on the same horizontal plane. The OCR equipment may not read information that is not centered properly causing unnecessary denials or incorrect payment. Only six line items should be entered per claim; do not squeeze two lines of information on one line.
What type of ink is used for Medicare claims?
Medicare Part B Basic Billing Manual states: “Claims should not be handwritten, upper case letters only must be used, print must be Pica 10 or 12 point type face, and printer ink should be black only.”
What happens if NAS envelopes are overstuffed?
NAS receives many overstuffed envelopes. This causes the material to become damaged, partially received, or lost altogether before it arrives in our office.
Can you use a dot matrix printer for CMS?
Providers who use dot matrix printers run the risk of their claims being processed slower and possibly incorrectly. OCR equipment is unable to read claims submitted with dot matrix printers as there are breaks in the letters or numbers. It is recommended that you use an ink jet or laser printer to complete the CMS–1500 claim form.
Can you use red ink on a CMS claim form?
Due to the use of Optical Character Recognition equipment, no red ink should be used to complete a CMS-1500 claim form. This equipment will “drop out” any red that is on the paper. The only ink that is picked up correctly is true black ink. Any variation of blue, purple, or red ink should not be used.
Do envelopes contain correspondence?
Envelopes should also contain similar contents. For example, one envelope should contain claims, another should contain correspondence. The time it takes to process all items received will improve if different items are mailed separately.
Can you print a CMS 1500 claim without red ink?
The CMS–1500 claim form must be submitted using the scannable, red ink version. These red ink versions can be purchased from a printer company, such as the U.S. Government Printing Office by calling (202) 512-1800. You can also contact the U.S. Government Printing office at the following address:
How to purchase a CMS-1500?
In order to purchase claim forms, contact the U.S. Government Printing Office at 1-866-512-1800, local printing companies, and/or office supply stores. Each of these vendors sells the CMS-1500 claim form in its various configurations (single part, multi-part, continuous feed, laser, etc).
How many line items are on a CMS 1500?
Do not include more than six line items on a CMS-1500 claim form.
What is OCR in Noridian?
Noridian uses optical character recognition (OCR) to process paper CMS-1500 claim forms. OCR is a means of inputting text into a computer. It involves scanning a paper document to create a digital image of the text and then using software to store knowledge about that digital image. With OCR, it is very important suppliers follow proper paper claim ...
What is the ASCA in Medicare?
The Administrative Simplification Compliance Act (ASCA) mandates the submission of electronic claims to Medicare unless a supplier meets certain "exceptions" described within the law.
What is EDI in healthcare?
Electronic Data Interchange (EDI) provides the ability to quickly and efficiently exchange healthcare information in a safe , secure, and cost-effective way . Electronic claims are transmitted to the Common Electronic Data Interchange (CEDI) contractor. After the electronic claim has been accepted by the CEDI, the claim is then transferred to the appropriate DME MAC for processing based on the beneficiary's address listed on the electronic claim.
Is OCR sensitive to ink?
The OCR equipment is sensitive to ink color. Follow these guidelines on ink color:
Can OCR scanners print red?
OCR scanners "drop out" any red that is on the paper. Use true black ink. Do not use any other color ink such as blue, purple, or red. Avoid using old or worn ink cartridges, toner cartridges, or printer ribbons. To process a claim correctly, proper alignment of the CMS-1500 form information is necessary.
What size paper do you need to attach a claim to a Medicaid claim?
Attachments must be on 8 ½" x 11" white paper and one-sided. Do not submit twosided material. Multiple claims cannot be submitted with one attachment. Each claim form that requires an attachment must have a separate attachment. Do not staple or paperclip the documentation to the claim form.
What is UB-04 form?
Use the UB-04 form to complete a Medicare claim for institutional services. To complete this form, refer to the instructions in UB-04 Claim Form Specifications in this chapter. Field information is required unless otherwise noted. This form may be prepared according to Medicare guidelines as long as all required fields are completed.
What ink is used for UB-04?
The Plan accepts UB-04 forms printed in Flint OCR Red, J6983, (or exact match) ink. Although a copy of the form can be downloaded from the CMS website, copies of the form cannot be used for submission of claims and will be rejected since your copy may not accurately replicate the scale or color of the form when scanned using Optical Character Recognition (OCR).
How long does it take to get a paper claim on a remittance?
Paper claims should appear on a remittance advice (RA) within 60 days of submission. Do not resubmit a claim prior to the 60-day period.
Can you mail a claim form with no attachments?
material" (for extraneous material) on the outside. Do not put claims that have no attachments in this envelope. Mail claims without attachments separately. Do not send attachments unless the attachment is required as unnecessary attachments delay claim processing.
Can you scan a UB-04?
Photocopies cannot be scanned and therefore are not accepted. There are key fields to properly identify and adjudicate claim information on a paper UB-04 form when submitted to our Plan. Below are guidelines identifying these fields to ensure timely and accurate processing of your claim submission.
Can you scan a form?
This scanning technology allows for the data contained on the form to be read while the actual form fields, headings and lines remain invisible to the scanner. Photocopies cannot be scanned and therefore are not accepted.
Why is it important to complete medical billing forms?
As well as being aware of the differences, it is important that a medical billing company complete these forms carefully. Keeping track of the specific requirements for each insurance company will avoid needless denials and ultimately speed up reimbursement.
What is a UB-04 Form?
Since then, the UB-04 has been the standardized form used by hospitals, ambulatory surgery centers, nursing facilities, and other medical and mental health institutions. These claims forms can be submitted both electronically and on paper.
How many fields are on UB-04 form?
The UB-04 form includes 81 fields, or form locators, while the 1500 includes 33. The extent to which these will need to be completed is determined by each carrier. Nevertheless, all insurance companies will require that the information be legible and correctly aligned within each box
Do CMS 1500 and UB-04 stand alone?
The two form types do not always stand alone. For example, if a surgeon performs a procedure in a facility such as a hospital or ASC, a CMS-1500 will be submitted for the surgeon’s services only, while a separate UB-04 form will be submitted for the use of the facility. Both forms will be needed to fully bill out for a procedure.
Do Medicare claims have to be submitted on a CMS 1500?
One exception to this rule is when a facility is billing to Medicare. All Medicare claims must be submitted on a CMS-1500.
What information is needed for a CMS-1500?
Both the CMS-1500 and UB-04 forms contain many of the same boxes that need to be filled out including patient demographics, provider identification information, procedures and charges and insurance plan identification information. The more information you can provide to the patient’s insurance company, the better. It is important to include information like when the first occurrence began, is it recurring or onset, if it was related to an accident, etc. Also, always be sure to recheck all claims for coding accuracy.
What is HCFA 1500?
CMS-1500 Form (sometimes called HCFA 1500): This is the standard health insurance claim form used for submitting physician and professional claims to bill Medicare providers. In other words, the CMS-1500 is used for individual provider claims and is used to submit charges under Medicare Part-B.
What is UB-04 form?
The UB-04 is the claim form for institutional facilities and includes the following: The form would be used for surgery, radiology, laboratory, or other facility services.
Can CMS 1500 and UB-04 be used interchangeably?
While the CMS-1500 and UB-04 forms may look similar, they are very different and have distinct purposes. Thus, the two forms cannot be used interchangeably. First, let’s look at the individual forms and see why they are different in their functions.
