
Do dialysis patients need dental prophylaxis? – Yes, for patients/clients receiving peritoneal dialysis. The dental hygienist should confirm with the nephrologist that the patient/client is medically stable to receive dental hygiene (and dental) treatment, as well as ascertain if antibiotic prophylaxis is indicated.
Do we give antibiotic prophylaxis to haemodialysis patients prior to dental surgery?
Forty-one per cent of respondents do not routinely give antibiotic prophylaxis to haemodialysis patients prior to dental surgery, but a majority (53%) would consider antibiotic prophylaxis if the patient had a synthetic arteriovenous fistula.
When is prophylaxis indicated for dental procedures?
For patients with these underlying cardiac conditions, prophylaxis is recommended for all dental procedures that involve manipulation of gingival tissue or the periapical region of teeth or perforation of the oral mucosa. those who have a prosthetic joint (s) and may be at risk for developing hematogenous infections at the site of the prosthetic.
Is antibiotic prophylaxis necessary for end-stage renal disease?
In the United States, there is a large and growing population of patients undergoing dialysis because of end-stage renal disease (ESRD). These patients present special management considerations for dentists, including antibiotic prophylaxis for the prevention of bacterial endocarditis (BE).
What are the AHA guidelines for prophylaxis of dialysis patients undergoing invasive dental treatment?
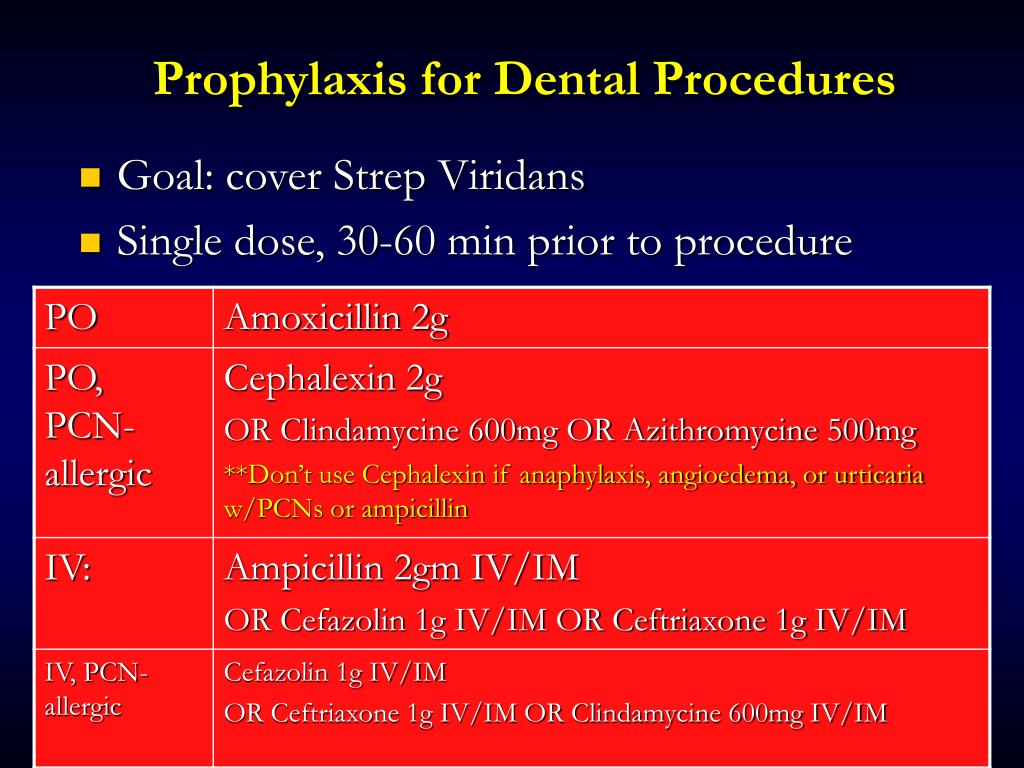
Antibiotic prophylaxis in dialysis patients undergoing invasive dental treatment The majority of clinicians follow the American Heart Association (AHA) guidelines with a single oral preoperative dose of 2 g amoxycillin or 600 mg clindamycin if patients are allergic to penicillin.
What are the dental considerations in patients with renal dialysis?
The dentist should be made aware that their patient has kidney disease or is on dialysis. Ideally, dental procedures, such as tooth extraction, should occur on a non-dialysis day for those on hemodialysis. Heparin, administered during hemodialysis, may cause some people to have extra bleeding.
What conditions need premedication for dental treatment?
Hematogenous infections are infections of the blood. They are both very serious and can lead to death. Premedication for dental treatment is recommended for all dental procedures involving manipulation of gingival tissue or the periapical region of the teeth, or perforation of the oral mucosa.
When do you need dental treatment after dialysis?
In addition, the body may not be capable of using calcium in a helpful way, which means teeth may become loose and painful. If you are on dialysis, you should aim to schedule dental appointments within 24 hours of your treatment.
What dental procedures do not require antibiotic prophylaxis?
Prophylaxis is NOT recommended for the following procedures that occur above the gumline and are not expected to cause bleeding:Routine fillings.Periodontal procedures if bleeding not anticipated.Simple root canal treatment.Rubber dam placement.Suture removal.Removable appliance placement.Oral impressions.More items...
Who needs antibiotics before dental work?
Antibiotics are often prescribed for a day or two before dental visits to prevent infections in certain people, such as those who have had hip or knee replacements, but current American Dental Association and American Heart Association guidelines no longer recommend this in most cases.
When is antibiotic prophylaxis recommended?
Prophylaxis at the Time of Cardiac Surgery Because endocarditis is known to cause severe morbidity and even death in such patients, perioperative prophylactic antibiotics are recommended. Endocarditis associated with open-heart surgery is most often caused by staphylococci.
Why is dental treatment day after dialysis?
This fact is important because of proper timing of dental intervention. Accordingly, since heparin prolongs the bleeding time, the tooth extraction should be done a day after dialysis when the anti-coagulent agent's presence is reduced to the minimum while the dialysis effect is maximal.
Can dialysis affect your teeth?
Dialysis and dry mouth With less saliva to bathe them, your teeth are more prone to decay. Less saliva can also lead to bad breath, gum disease, and tooth loss (see Figure 2). In one study, the average number of teeth in people on dialysis was just 20—a loss of 12.
Why is it not advisable to perform invasive dental procedures on days when dialysis has occurred?
Risk of Bleeding. Dental treatment with risk of bleeding should be postponed to nondialysis day since the anticoagulant effect of heparin is absent, the bloodstream is free from toxic metabolites, and the patient is not debilitated by the treatment.
Do kidney transplant patients need antibiotics before dental work?
For liver, kidney and pancreas transplant recipients, it is not necessary to take antibiotics prior to routine dental appointments from a transplant perspective; however, patients are advised to consult with their primary care doctor and dentist to determine whether antibiotics may be needed for other medical ...
Do immunocompromised patients need antibiotics before dental work?
Recent investigations have demonstrated that in medically compromised patients in whom their systemic conditions are well controlled, routine dental extractions of non-infected teeth can be performed without antibiotics with low levels of post-operative infections and complications.
Who gets antibiotic prophylaxis?
Some types of surgery have a high risk of infection. Your doctor will probably give you prophylactic antibiotics if you're having one of these types of surgeries. Some of these surgeries include: Head or neck cancer surgery.
Does dentistry need pre med?
Students who wish to pursue the DMD program must complete a two-year pre-dentistry course and have any medical-related Bachelor's degree program. Those who aspire to become Dentists but graduated with a non-medical undergraduate program may enroll for the pre-dentistry course.
Do patients with knee replacement need antibiotics for dental work?
ALL patients who have undergone total joint replacement surgery should receive antibiotic prophylaxis* prior to any dental procedures and additional procedures as outlined below for 2 years after your surgery.
Is premed needed for rheumatic fever?
In other words, the only indications now are the high risk patients described above. Mitral valve regurgitation and a history of rheumatic fever alone are no longer indications for antibiotic premedication. 4. The following dental procedures do not require antibiotic prophylaxis under any conditions: a.
Is it necessary to take antibiotics before teeth cleaning?
It's usually a necessary part of such procedures as tooth extraction, root canal therapy or deep cleaning of the gums. In other cases, antibiotics may be prescribed to prevent an infection. This type of application is referred to as premedication.
How many teeth do you lose on dialysis?
In one study, the average number of teeth in people on dialysis was just 20—a loss of 12. Most transplant programs will require you to have healthy teeth and gums. A dry mouth and gum disease can make it harder to eat, too.
Why is saliva important for teeth?
Saliva moistens food so it's easier to swallow and less likely to scratch your throat. And, it lubricates and protects your tongue and the delicate tissues in your mouth. For all of these reasons, saliva is vital for healthy teeth and gums.
What do you need to know about kidney disease?
Dialysis and Dental Health: What You Need to Know. Keeping a healthy smile when you have kidney failure can take some extra effort. The type of treatment you choose can affect the health of your teeth and gums. In turn, your oral health can have an impact on the rest of your body. If you were a shark, you could grow a new set ...
How to get rid of tooth decay?
A drug change may help. Use sugar-free hard candy or gum to improve saliva flow. Avoid sugar: bathing your teeth in it raises your risk of tooth decay. Sticky foods like candy, dried fruit, or potato or corn chips (which stick to teeth once they are chewed) are more likely to cause problems.
Does dialysis help your mouth?
3 In the second study, much more gum disease was found in people on standard HD than in a group on peritoneal dialysis (PD) or a group who did not yet need dialysis. 4 In the third study, people on standard HD had more gum bleeding than those on PD—but both those on PD and HD had more tooth plaque than healthy people. 5 The results suggest that the closer a treatment can bring you to normal kidney function, the healthier your mouth may be, too.
Can dialysis cause low albumin levels?
A study found that people on dialysis who had severe gum disease also had low blood albumin (protein) levels. 1 Not getting enough protein can lead to malnutrition—which is a strong risk factor for death in people on dialysis. 2.
Can antibiotics be given at the dentist?
Antibiotics at the dentist. When you have your teeth cleaned, bacteria in pockets under the gum line may get into your bloodstream. These germs may stick to a dialysis fistula or graft and cause an infection. Some nephrologists prescribe antibiotics before a dental visit to help prevent a problem.
How does kidney disease affect dental care?
Kidney disease and its treatment can affect the oral cavity and dental treatment. As it progresses, there is a concomitant decrease in kidney function and it is associated with complications in nearly all organ systems. Kidney disease and kidney failure can be classified broadly as acute kidney injury (AKI) or chronic kidney disease (CKD). This chapter first gives a detailed background on CKD and AKI before focusing on medical and dental management. Under medical management, a set of key questions that have to be asked to the physician and another set that have to be asked to the patient, are also listed. Under dental management, risks of dental care, susceptibility to infection, drug actions/interactions, and the patient's ability to tolerate dental care, are described. A note on special considerations that are needed for a renal transplant recipient is also given at the end of the chapter.
What is CKD in dentistry?
Chronic kidney disease, (CKD) a gradual and inevitable deterioration in renal function, is the disease with the most associations in dentistry. Dosage adjustment is one among the vital elements to be familiar with, during their oral care. CKD patients take extended duration to filter out medications, therefore, dosage must always be tailored under the supervision of nephrologist. The relished benefits from antibiotic could transform as anti-microbial resistance on its abuse and nephrotoxic when contraindicated drugs are encouraged. It's a comeback for antibiotics as new patented drug belonging to oxazoliodine group has driven the researchers to handle the emerging AMR. The present communication provides pharmacological factors influencing in prescribing/restricting the antibiotics for CKD patient from the dentist's point of view. Conjointly, the formulas destined for calculating the optimal dosage of antibiotics have been documented in depth to aid oral physicians.
Is AP a common procedure?
Antibiotic prophylaxis (AP) still represents a common but often misused procedure in dental practice , thus aggravating the risk for antimicrobial resistance and adverse effects occurrence. Our primary objective is to review the available scientific evidence regarding AP in dentistry both among healthy subjects and medically compromised patients. Additionally, the latest available guidelines provided by some of the most authoritative associations are here discussed. AP is advisable only in a small percentage of patients where a risk of severe infective complications (i.e. infective endocarditis and prosthetic joint infection, septicaemia in severely immuno-compromised patients, bisphosphonate-related osteonecrosis of the jaw) exists. On the contrary, little or no scientific evidence exists for AP in subjects with other systemic diseases as well as in healthy individuals. This pioneering recommendation is strongly evidence-based, since a consistent association between any dental procedure and the development of local and distant infective complications is still lacking. In addition, the daily bacteraemia secondary to routine habits has been thought to be robustly associated with a greater risk of systemic disease bacterial-related than a single dental procedure exposure. Compliance of general dental or family practitioners to the current recommendations seems not to be optimal, thus, efforts to improve it should be planned and undertaken.
Why are people on dialysis?
In the United States, there is a large and growing population of patients undergoing dialysis because of end-stage renal disease ( ESRD). These patients present special management considerations for dentists, including antibiotic prophylaxis for the prevention of bacterial endocarditis (BE). ESRD pat …
Can antibiotics be used before dental treatment?
Prophylactic antibiotic therapy prior to dental treatment for patients with end-stage renal disease. In the United States, there is a large and growing population of patients undergoing dialysis because of end-stage renal disease (ESRD).
Why are antibiotics used in dentistry?
Antibiotics are used in addition to appropriate treatment to aid the host defences in the elimination of remaining bacteria.
How long does amoxicillin last after molar surgery?
Amoxicillin 2 000 mg for five days at a suitable dose and interval helps to cover the treatment requirements after third molar surgery[43]. Studies show a decrease in postoperative infection, following the use of antibiotics after orthognathic surgery[44],[45].
What is the best antibiotic for odontogenic infections?
Penicillin is the drug of choice in treating odontogenic infections as it is prone to gram positive aerobes and intraoral anaerobes, organisms found in alveolar abscess, periodontal abscess and necrotic pulps. Both aerobic and anaerobic microorganisms are susceptible to penicillin[9]. Penicillinase-resistant penicillin or an ampicillin-like derivative is prescribed for infections caused by penicillinase-producing staphylococci or those involving gram-negative bacteria[4]. A combinations of penicillin and clavulanic acid can be preferred for infections caused by staphylococcus, streptococci and pneumococci. Patients allergic to penicillin are treated with clindamycin 300 mg (65%) which is the ideal drug of choice and followed by azithromycin(15%) and metronidazole-spiramycin(13%)[10]. The first generation cephalosporins like cephadroxil, cephadrine provide a broad spectrum antibiotic when gram positive organisms are suspected to be the causative factor of the infection. Cephalosporin is advisable for delayed-type allergic reactions to penicillin and when erythromycin cannot be used. Cephalosporin is indicated in endodontic practice as they exhibit good bone penetration[11]. Tetracyclines are bacteriostatic antibiotics that specifically inhibit the binding of aminoacyl-t-RNA synthetases to the ribosomal acceptor site[12]. For cases of acute necrotizing ulcerative gingivitis requiring systemic antibiotic therapy in which penicillin is precluded, tetracyclines are most beneficial. The side effects encountered most often by the usage of penicillin are hypersensitivity, which is found roughly in 3%-5% of the population[13]. As with most antibiotics the occurrence of allergic reactions of all degrees of severity is common. The penicillins, followed by the cephalosporins and tetracyclines, are most frequently implicated in these reactions. Azithromycin has shown enhanced pharmacokinetics in encountering the anaerobes involved in endodontic infection. The oral dosage of azithromycin is 500 mg loading dose followed by 250 mg once a day for five to seven days[14]. Ciprofloxacin is one of the common drugs used for endodontic infections. The effective action against oral anaerobes, gram positive aerobic organisms (Staphylococcus aureus, Enterobacterspecies and Pseudomonas) demands the need of ciprofloxacin for endodontic infections[15]. Metronidazole is a synthetic antimicrobial agent, which is bactericidal and most effective against anaerobes. Baumgartner has shown effective number of bacteria resistant to metronidazole[16]. The recommended dosage is 1 000 mg loading dose followed by 500 mg every six hours for five to seven days[14]. Clindamycin remains the second drug of choice next to penicillin in treating odontogenic infections. It was observed that 10% of the Streptococcus viridans bacteria were resistant to clindamycin[17]. Gilad et aldeveloped a new clindamycin-impregnated fiberas an intracanal medicament, which is effective against other common endodontic pathogens[18]. Due to its adverse side effects the routine use of clindamycin is not advised. However, b lactum antibiotics still remain the drug of choice in odontogenic infections among the health professionals[19].
Why is vancomycin used in prosthetic heart valves?
Vancomycin and streptomycin are used prophylactically for prevention of infective endocarditis in patients with prosthetic heart valves. Prophylactic failure is possible to occur in patients with congenital heart disease if the proper antibiotic is not selected[36].
What antibiotics are used for syphilis?
Tuberculosis management requires a long duration of antibiotic service which includes ethambutol, isoniazid, rifampicin, pyrazinamide and streptomycin. Penicillin G benzatine is administered in the management of syphilis. Clofazimine, dapsone and rifampicin are used for treating leprosy. 2.3.
Is penicillin good for ulcerative gingivitis?
For cases of acute necrotizing ulcerative gingivitis requiring systemic antibiotic therapy in which penicillin is precluded, tetracyclines are most beneficial. The side effects encountered most often by the usage of penicillin are hypersensitivity, which is found roughly in 3%-5% of the population[13].
Is antibiotics necessary for dental procedures?
Antibiotic therapy is mandatory and essential in medicine and dentistry. Penicillin is the drug of choice in treating dental infections. Patients at high risk include those with infective endocarditis, immunocompromised conditions and dental procedures which may produce bacteremias. Invasive dental procedures if performed in such patients should be preceded with an antibiotic prophylaxis. Consultation with the physicians and specialists is required before any dental treatment is carried out in organ transplant and pregnant patients. Special caution needs to be addressed to the above patients to determine the best outcome of dental procedure and to provide the required dose adjustments and thereby preventing the complications in the dental clinic. And hence it is clear that apart from invasive dental procedures in high risk patients not all dental procedures require the need for antibiotic prophylaxis. Recommendations on antibiotic prescribing are essential to prevent overprescribing of antibiotic. The prescription of antibiotics should be considered adjunctive to the dental treatment.
Is antibiotic prophylaxis indicated prior to dental procedures?
Compared with previous recommendations, there are currently relatively few patient subpopulations for whom antibiotic prophylaxis may be indicated prior to certain dental procedures.
Can you take antibiotics for joint replacement?
According to the ADA Chairside Guide, for patients with a history of complications associated with their joint replacement surgery who are undergoing dental procedures that include gingival manipulation or mucosal incision, prophylactic antibiotics should only be considered after consultation with the patient and orthopedic surgeon; in cases where antibiotics are deemed necessary , it is most appropriate that the orthopedic surgeon recommend the appropriate antibiotic regimen and, when reasonable, write the prescription.
Can you give antibiotics prior to dental surgery?
With the exception of the AHA/ACC guidelines regarding prevention of infective endocarditis, 7, 8, 10 there is no general guidance or recommendation to provide antibiotics as a prophylactic measure prior to dental procedures except for specific individuals with extenuating circumstances, where the determination and prescription is made by the patient’s surgeon or other treating physician. However, there are a myriad of other conditions that either patients, physicians, or dentists may think that antibiotic prophylaxis prior to dental treatment might be warranted to prevent development of infections at remote locations by bacteria normally associated with the oral flora.
Is there a correlation between antibiotic prophylaxis and endocarditis?
In 2015, The Lancet published a study out of the United Kingdom that reported a correlation between institution of more limited antibiotic prophylaxis guidelines by the National Institute for Health and Clinical Evidence (NICE) in 2008 and an increase in cases of infective endocarditis. 13 Because of the retrospective and observational nature of the study, the authors acknowledged that their “data do not establish a causal association.” At this time, the ADA recommends that dentists continue to use the AHA/ACC guidelines discussed above. Dental professionals should periodically visit the ADA website for updates on this issue.
Do you have to premedicate for antibiotic prophylaxis?
Sometimes, patients forget to premedicate before their appointments. The recommendation is that for patients with an indication for antibiotic prophylaxis, the antibiotic be given before the procedure. This is important because it allows the antibiotic to reach adequate blood levels. However, the guidelines to prevent infective endocarditis 7, 8 state, “If the dosage of antibiotic is inadvertently not administered before the procedure, the dosage may be administered up to 2 hours after the procedure.” If a patient with an indication for prophylaxis who appropriately received antibiotic premedication prior to a dental procedure one day and who is then scheduled the following day for a dental procedure also warranting premedication (e.g., dental prophylaxis), the antibiotic prophylaxis regimen should be repeated prior to the second appointment. Because of the nature of the pharmacokinetics of an antibiotic prophylaxis regimen, a single loading dose is given in order to cover the period of potential bacteremia produced by a single procedure. 11-13
Is antibiotic prophylaxis recommended for congenital heart disease?
b Except for the conditions listed above, antibiotic prophylaxis is no longer recommended for any other form of congenital heart disease.
Is endocarditis prophylaxis premedication?
For infective endocarditis prophylaxis, American Heart Association guidelines (updated with a scientific statement in 2021) support premedication for a relatively small subset of patients. This is based on a review of scientific evidence, which showed that the risk of adverse reactions to antibiotics generally outweigh the benefits of prophylaxis for many patients who would have been considered eligible for prophylaxis in previous versions of the guidelines. Concern about the development of drug-resistant bacteria also was a factor.
What happens during a kidney transplant?
During workup for a kidney transplant a person will undergo a thorough oral exam. Infections from gum disease or advanced tooth decay can prevent someone from being eligible or delay the transplant until dental work is completed.
Why is oral hygiene important?
Good oral health,or dental hygiene,is important for people with chronic kidney disease who may or may not be at end stage renal disease and are on dialysis,especially if their renal disease is caused by diabetes.
What causes kidney disease?
Diabetes is one of the major causes of chronic kidney disease. If your renal disease is caused by diabetes, you should know that those with diabetes are more prone to having the following dental problems: 1 Cavities (tooth decay) 2 Gum disease (periodontal disease) 3 Problems with the salivary glands 4 Fungal infections 5 Infections and delayed healing
What causes tooth decay?
Tooth decay. Tooth decay and gum disease are caused by plaque. Plaque is a sticky film of bacteria that coats the teeth. The sugars and starches of the food you eat react with the plaque, causing it to release acids. These acids wear away the hard tooth enamel, eventually leading to cavities and tooth decay.
How to determine kidney disease stage?
Determine which stage of kidney disease you’re in by calculating a glomerular filtration rate (GFR) and start managing your health.
Why are people with kidney disease more susceptible to infections?
A study in the Journal of Clinical Periodontology reported that people with kidney disease and those on dialysisare more likely to have periodontal disease and other oral health problems than the general population. Buildup of bacteria in the mouth can cause infection. Because people with kidney disease have weakened immune systems, they are more susceptible to infections.
Why do kidneys lose teeth?
Because people with kidney disease have weakened immune systems, they are more susceptible to infections. Bone loss in the jaw can occur in those with kidney disease. Calcium imbalance contributes to loss of calcium from the bones resulting in weak bones. Weak bones can cause teeth to become loose and potentially fall out.
