How to cure atrial flutter?
- Get on your hands and knees on the floor.
- Hold your back straight in a "tabletop" position.
- Slowly move your hips back and extend your arms, keeping your hands planted.
- Tuck your tailbone to sit your butt on your heels. You may need to spread your knees farther apart to sink back enough.
- Keep breathing as you feel the stretch through your arms and back.
How to get rid of atrial fibrillation once and for all?
Medications, shocking the heart back into rhythm, or even a procedure to potentially cure atrial fibrillation, called a catheter ablation, may be necessary. Certainly, with A-fib, an ounce of prevention is definitely worth a pound of cure!
Is ablation of atrial flutter always safe?
Background: Radiofrequency ablation of typical atrial flutter is largely used and is considered as safe. The purpose of the study was to evaluate the prevalence and the causes of severe adverse...
What causes atrial flutter (AFL) following open heart surgery?
What Causes Atrial Flutter? In many cases, no underlying cause for atrial flutter is identified. In some patients, atrial flutter may occur in patients with prior open heart surgery, even occurring many years before. Some patients with atrial flutter have other heart conditions or a history of high blood pressure.
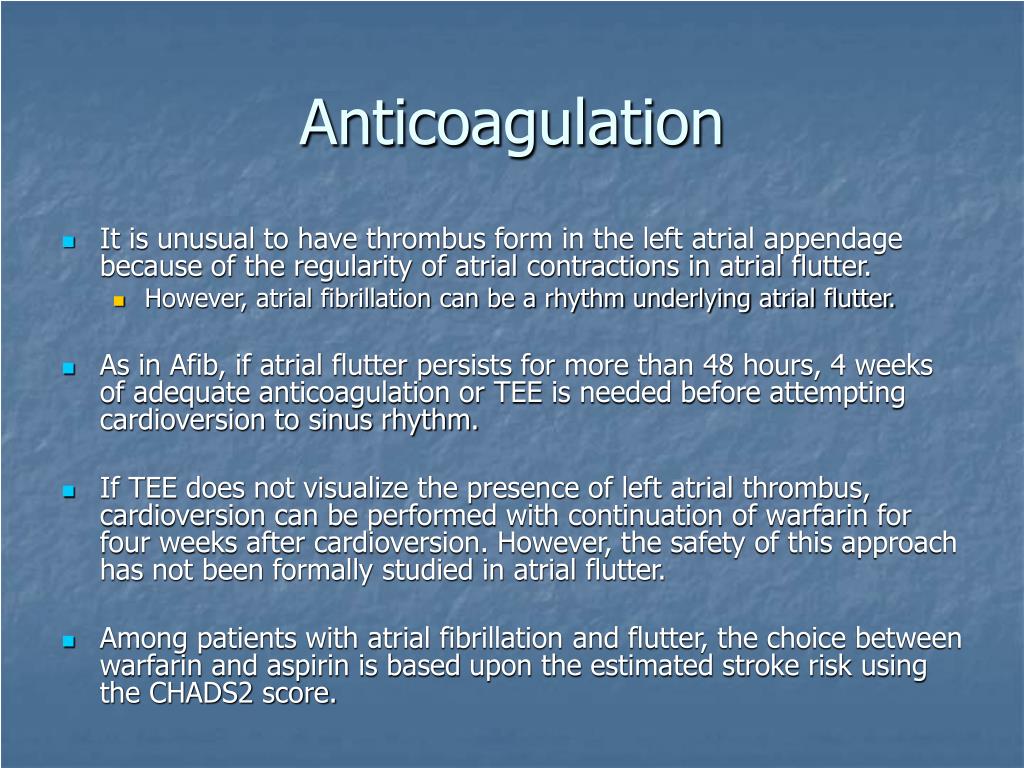
Do patients with atrial flutter need anticoagulation?
Most patients with atrial flutter should be considered for chronic anticoagulation in a manner similar to those with atrial fibrillation (AF). This recommendation is based not only on the fact atrial flutter carries a risk for systemic embolization but also that these patients usually have episodes of AF.
What is the most common treatment for atrial flutter?
Currently, atrial flutter is successfully "cured" by radiofrequency catheter ablation; but treatment to restore atrial fibrillation to sinus rhythm has been the traditional use of medications and external cardioversion.
What is the drug of choice for atrial flutter?
Dofetilide is effective in 70-80% of patients with atrial flutter. This drug should be initiated in an inpatient setting. Ibutilide [17, 18, 19, 20] is also effective, converting recent-onset atrial flutter to sinus rhythm in 63% of patients with a single infusion.
Can atrial flutter cause blood clots?
Although atrial flutter is usually not life-threatening at first, it does limit how well your heart pumps blood. This can cause a clot to form in your heart. If the clot breaks loose, it could lead to a stroke. Over time, atrial flutter can weaken your heart muscle.
Which is worse AFib or a flutter?
Both heart diseases have the potential of becoming serious. However, many doctors and other health care professionals consider atrial flutter to be less serious than atrial fibrillation because flutter symptoms tend to be less severe and flutter waves have less risk of embolization (clot formation).
How do you get rid of atrial flutter?
At a minimum, these strategies may help you relax and cope with the episode until it stops.Engage in deep, mindful breathing. ... Get some exercise. ... Valsalva maneuver. ... Practice yoga. ... Put some cold water on your face. ... Contact a health professional.
What is the first line treatment for atrial flutter?
Rate control. Rate control is the first line of management for symptomatic AFIB/AFLUT with Rapid Ventricular Rate (RVR). For the majority of patients that are hemodynamically stable and do not require immediate cardioversion, anti-arrhythmic drug therapies can potentially be utilized.
What is initial treatment of atrial flutter?
To slow the ventricular response, administration of calcium channel blockers (CCBs) such as diltiazem, or beta blockers such as esmolol, are commonly used as initial treatment. Beta-adrenergic blockers are especially effective in the presence of thyrotoxicosis and increased sympathetic tone.
What is the difference between AF and atrial flutter?
Normally, the top chambers (atria) contract and push blood into the bottom chambers (ventricles). In atrial fibrillation, the atria beat irregularly. In atrial flutter, the atria beat regularly, but faster than usual and more often than the ventricles, so you may have four atrial beats to every one ventricular beat.
How serious is an atrial flutter?
Atrial flutter is a type of abnormal heart rhythm, or arrhythmia. It occurs when a short circuit in the heart causes the upper chambers (atria) to pump very rapidly. Atrial flutter is important not only because of its symptoms but because it can cause a stroke that may result in permanent disability or death.
Can you live a normal life with atrial flutter?
Most patients with atrial flutter lead an entirely normal life with modern drugs and treatments.
Can I exercise with atrial flutter?
If you are in AF all the time (persistent AF), you can exercise as much as you want, as long as your heart rate is under control, you are stable on your treatment and are feeling well. If you're not feeling well because of your AF, ask your GP or specialist for exercise advice.
What is the first line treatment for atrial flutter?
Rate control. Rate control is the first line of management for symptomatic AFIB/AFLUT with Rapid Ventricular Rate (RVR). For the majority of patients that are hemodynamically stable and do not require immediate cardioversion, anti-arrhythmic drug therapies can potentially be utilized.
Can you live a long life with atrial flutter?
The good news is that although AF is a long-term condition, if managed correctly, you can continue to lead a long and active life. There are a number of steps you can take that will help you manage your condition, lower your risk of stroke and relieve any worries you may have.
How serious is an atrial flutter?
Atrial flutter is a type of abnormal heart rhythm, or arrhythmia. It occurs when a short circuit in the heart causes the upper chambers (atria) to pump very rapidly. Atrial flutter is important not only because of its symptoms but because it can cause a stroke that may result in permanent disability or death.
What can trigger atrial flutter?
Causes of atrial flutter include:Heart valve disorders.Birth defect in your heart.Coronary artery disease.High blood pressure.Overactive thyroid.
Which echocardiography shows a more organized atrial mechanical function?
However, transmitral and left atrial appendage Doppler echocardiography demonstrate more organized atrial mechanical function with sustained atrial flutter, as opposed to AF, in which organized atrial contraction is absent.
Is atrial flutter a chronic disease?
Most patients with atrial flutter should be considered for chronic anticoagulation in a manner similar to those with atrial fibrillation (AF). This recommendation is based not only on the fact atrial flutter carries a risk for systemic embolization but also that these patients usually have episodes of AF.
What is atrial flutter?from ncbi.nlm.nih.gov
Atrial flutter, a supraventricular arrhythmia, is one of the most common rhythm disturbances of the heart. It is characterized by a fast atrial rate with a fixed or variable ventricular rate. There are several atrial contractions to one ventricular contraction and symptoms include fatigue, palpitations, and syncope. This activity outlines the evaluation and treatment of atrial flutter and highlights the role of the interprofessional team in managing patients with this condition.
What is the INR for a stroke?from academic.oup.com
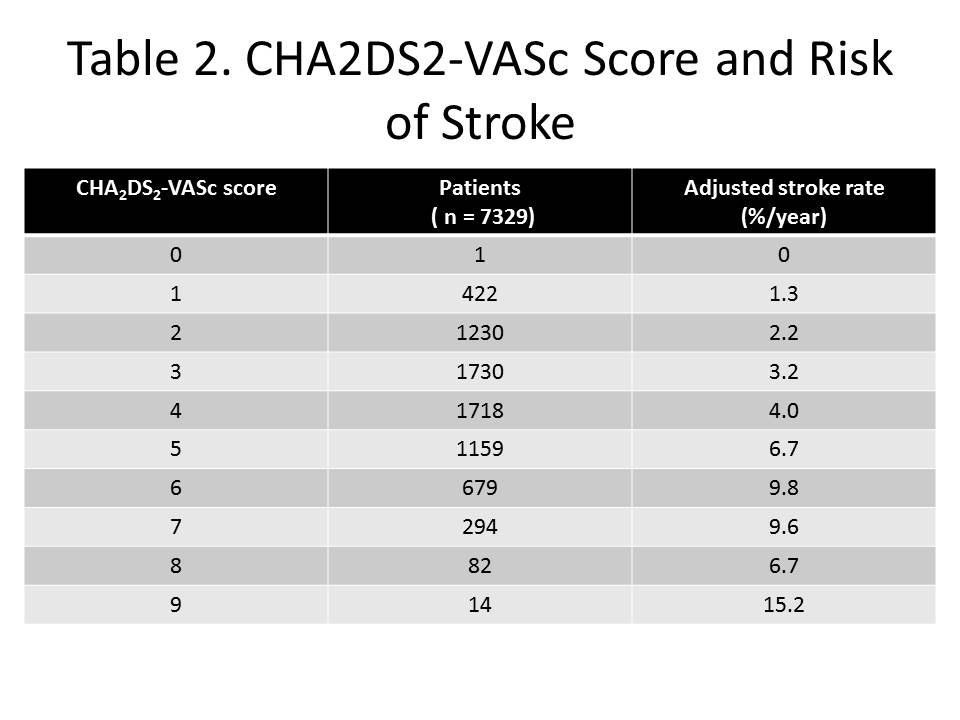
The evidence strongly supports the use of oral anticoagulation, aiming at an international normalised ratio (INR) between 2 and 3, in patients with AF who have an average or higher risk of stroke. This also includes the elderly. Only in younger patients without additional risk factors is the use of oral anticoagulation not indicated. Aspirin is advised by the guidelines ( Table 2 ) for lower risk patients [11] but a true evaluation in this patient group is lacking [84] . Paroxysmal AF and atrial flutter should be treated in the same way as persistent and permanent forms of AF. For high-risk patients with a contraindication to anticoagulants, a left atrial occluder may be valuable, and is currently under investigation. Guidelines for the use of anticoagulation surrounding pulmonary vein isolation are not yet available, but a high level of anticoagulation is necessary during the procedure. It is appropriate to prescribe oral anticoagulation before and to re-initiate it after the procedure. A covering period with heparin until the INR reaches the level of 2 is advisable. It is possible that medical practice will change with the introduction of new antithrombin drugs and with further documentation of the efficacy of low molecular heparin in this area. The initial optimism over the introduction of ximelagatran has been tempered by criticism on the basis of its side effects [33] .
What does a physical exam show for atrial flutter?from ncbi.nlm.nih.gov
The physical exam in patients with atrial flutter will show regular or irregularly regular peripheral pulse ( due to variable conduction from the atrioventricular node), jugular venous distension, respiratory sounds with crackles in lung fields, tachycardia, abdominal distention, and lower extremities edema when congestion occurs.
What is the low voltage area of the right atrium?from ncbi.nlm.nih.gov
In patients without prior cardiac intervention, the atrial flutter circuit can be low voltage areas like the lateral right atrium,[10]this might be secondary to fibrosis due to chronic atrial high pressures, or cardiomyopathy that can produce fibrosis of the myocardium and creating low voltage areas that allow atrial flutter to occur. [10]
What is atypical atrial tachycardia?from ncbi.nlm.nih.gov
Atypical atrial flutter or other macroreentrant atrial tachycardia has a circuit configuration different from the typical right atrial flutter circuit. Electrophysiologic studies and intracardiac mapping are the only means to determine the exact mechanism or area generating the atrial flutter. Different from typical atrial flutter, the presence of atypical atrial flutter is related to structural heart diseases as prior cardiac surgery or ablation procedures. [8]
How long after cardioversion should I take anticoagulation?from academic.oup.com
Anticoagulation is recommended for 3 to 4 weeks before and after cardioversion for patients with AF of unknown duration and for AF of more than 48 hours duration [11] . A reasonable alternative strategy is early cardioversion with a short period of anticoagulation therapy after exclusion of LA/LAA thrombi with TOE [79] .
What causes atrial flutter in CTI?from ncbi.nlm.nih.gov
The initiation of atrial flutter is due to an ectopic beat that depolarizes one segment of the pathway of the circuits that become refractory and starts the tachycardia from a no-refractory segment. [3]
What is the CHA score for anticoagulation?
Lin et al comment that current European guidelines recommend that anticoagulation is prescribed at CHA 2 DS 2 -VASc score two or higher (and considered in those with a score of one) in both patients with atrial flutter and those with atrial fibrillation.
Is atrial flutter the same as atrial fibrillation?
Authors Yu-Sheng Lin (Division of Cardiology, Depart of Internal Medicine, Chang Gung Memorial Hospital, Chiay, Taiwan) and others report that atrial flutter is similar to atrial fibrillation “in that its incidence increases with age and it contributes to heart failure, stroke, and all-cause mortality”.
What is atrial flutter?
Atrial flutter, a supraventricular arrhythmia, is one of the most common rhythm disturbances of the heart. It is characterized by a fast atrial rate with a fixed or variable ventricular rate. There are several atrial contractions to one ventricular contraction and symptoms include fatigue, palpitations, and syncope. This activity outlines the evaluation and treatment of atrial flutter and highlights the role of the interprofessional team in managing patients with this condition.
What tests are used to evaluate atrial flutter?
Summarize the use of electrocardiogram, echocardiogram and laboratory tests in the evaluation of atrial flutter.
What is the most common arrhythmia?
Atrial flutter is one of the most common arrhythmias and is characterized by an abnormal cardiac rhythm that is fast with an atrial rate of 300beats/min and a ventricular rate that can be fixed or be variable that can cause palpitations, fatigue, syncope, and embolic phenomenon. [1]
What is supraventricular arrhythmia?
Supraventricular arrhythmias are a diverse group of atrial arrhythmias. Atrial fibrillation and atrial flutter are the most common of these atrial arrhythmias, and the other less common supraventricular arrhythmias are atrial tachycardias, atrioventricular reentrant tachycardia, atrioventricular nodal tachycardia, and others.
How many beats per minute in an atrial wave?
Electrocardiogram generally shows flutter waves with the absence of an isoelectric line between QRS complexes, with an atrial wave around 300 beat s per minute with ventricular conduction that can be 2 to 1, 3 to 1 or 4 to 1 or with variable conduction due to Wenckebach phenomenon.
Why is there no isoelectric line between P waves and QRS complexes?
The absence of an isoelectric line between P waves or QRS complexes is due to the constant cycling of the circuit or atrial activation.
Why do flutter waves resemble picket fences?
In inferior leads, typical flutter waves resemble a picket fence or sawtooth because the P waves are negative due to the direction of the vector.
What is the rate of atrial flutter?
Atrial flutter is an abnormal cardiac rhythm characterized by rapid, regular atrial depolarizations at a characteristic rate of approximately 300 beats/min and a regular ventricular rate of about 150 beats/min in patients not taking atrioventricular (AV) nodal blockers. It can lead to symptoms of palpitations, shortness of breath, fatigue, or lightheadedness, as well as an increased risk of atrial thrombus formation that may cause cerebral and/or systemic embolization.
Is atrial flutter the same as atrial fibrillation?
Atrial flutter occurs in many of the same situations as atrial fibrillation, which is much more common. Atrial flutter may be a stable rhythm or a bridge arrhythmia between sinus rhythm and atrial fibrillation, or an organized rhythm in atrial fibrillation patients treated with antiarrhythmic drugs.
What increases the risk of atrial flutter?
What increases my risk for atrial flutter? High blood pressure. Heart failure, heart surgery, or other heart conditions. Age 65 years or older. A blood clot in your lungs. Thyroid disease, obesity, or diabetes. Heavy alcohol use. Certain medicines, such as some antidepressants, bronchodilators, and cancer medicines.
How can I manage atrial flutter?
Know your target heart rate. Learn how to take your pulse and monitor your heart rate.
What is atrial flutter?
Atrial flutter is an irregular heartbeat. It reduces your heart's ability to pump blood, which means you do not get enough oxygen. An irregular heartbeat could lead to a life-threatening blood clot or stroke.
How is atrial flutter diagnosed?
Your healthcare provider will ask about your symptoms and if they come and go. He or she will measure your heart rate. Tell him or her what health conditions you have and what medicines you take. He or she will also ask if you smoke, drink alcohol, or use any illegal drugs. You may need any of the following tests:
What does it mean when your heart beats irregularly?
Atrial flutter is an irregular heartbeat. It reduces your heart's ability to pump blood, which means you do not get enough oxygen. An irregular heartbeat could lead to a life-threatening blood clot or stroke.
How to keep your gums from bleeding when taking blood thinners?
Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your te eth. This can keep your skin and gums from bleeding.
Is warfarin a blood thinner?
Warfarin is a blood thinner that you may need to take. The following are things you should be aware of if you take warfarin: Foods and medicines can affect the amount of warfarin in your blood. Do not make major changes to your diet while you take warfarin.
Who developed the ACC/AHA/ESC guidelines for the management of patients with atrial fibrillation?
Fuster V, Rydén LE , Asinger RW, et al. ACC/AHA/ESC Guidelines for the Management of Patients With Atrial Fibrillation: Executive Summary A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines and Policy Conferences (Committee to Develop Guidelines for the Management of Patients With Atrial Fibrillation) Developed in Collaboration With the North American Society of Pacing and Electrophysiology. Circulation 2001; 104:2118.
What is the glomerular filtration rate for AF?
For patients with AF and severe kidney disease (stage G4 or G5; estimated glomerular filtration rate <30 mL/min/1.73 m 2 ), on dialysis, or with acute renal injury, DOAC is generally avoided and VKA is generally the preferred long-term anticoagulant. Patients with stage 4 and 5 CKD are at higher risk of having unpredictable sudden deterioration in renal function than patients with normal renal function, and such deterioration could cause an abrupt reduction in clearance of a DOAC that depends on renal metabolism. In such a setting, use of an agent such as warfarin that allows for therapeutic drug monitoring may be preferred. A time in the therapeutic range of >70 percent is desirable. (See "Direct oral anticoagulants (DOACs) and parenteral direct-acting anticoagulants: Dosing and adverse effects", section on 'Chronic kidney disease' and "Warfarin and other VKAs: Dosing and adverse effects", section on 'Monitoring (PT/INR)' .)
What is the recommended INR for VKA?
Vitamin K antagonist — For patients with AF treated with VKA (eg, warfarin ), an INR between 2.0 and 3.0 is recommended with an average TTR >70 percent [ 18,19 ]. This is based upon the increased risk of stroke observed with INR values significantly below 2 (four- to sixfold at an INR of 1.3 compared with an INR of 2 or above) and the increased risk of bleeding associated with INR above 3.0 ( figure 1) [ 20-24 ]. Dosing of warfarin is discussed in detail separately. (See "Warfarin and other VKAs: Dosing and adverse effects", section on 'Warfarin administration' .)
What is the INR for a stroke?
However, we recommend an INR between 2.0 and 3.0 for these patients as well [ 24 ].
Is there a randomized controlled trial comparing DOACs?
Regarding the relative efficacy and safety of the DOAC agents, no randomized controlled trials (RCTs) directly comparing the DOACs have been published. Published observational studies have many limitations and are no substitute for head to head RCTs [ 10-14 ].
Can you continue VKA with AF?
However, it is reasonable to continue VKA in these patients.
Can anticoagulant failure cause thromboembolic events?
Anticoagulant failure — Thromboembolic events occur despite adequate anticoagulation in patients with AF . Predictors of these events include (see "Early antithrombotic treatment of acute ischemic stroke and transient ischemic attack", section on 'Atrial fibrillation' ):
