Does cricoid pressure prevent aspiration of gastric content during rapid sequence intubation?
Background: Cricoid pressure is considered to be the gold standard means of preventing aspiration of gastric content during Rapid Sequence Intubation (RSI). Its effectiveness has only been demonstrated in cadaveric studies and case reports.
Is cricoid pressure necessary?
Since cricoid pressure was introduced into clinical practice, controversial issues have arisen, including necessity, effectiveness in preventing aspiration, quantifying the cricoid force, and its reliability in certain clinical entities and in the presence of gastric tubes.
What is a cricoid pressure on the stomach?
cricoid pressure refers to digital pressure against the cricoid cartilage of the larynx, pushing it backwards with the intention of oesophageal compression against the vertebrae and prevention of passive regurgitation of gastric and oesophageal contents.
What is cricoid pressure in a chest xray?
cricoid pressure refers to digital pressure against the cricoid cartilage of the larynx, pushing it backwards with the intention of oesophageal compression against the vertebrae and prevention of passive regurgitation of gastric and oesophageal contents

Why is cricoid pressure no longer recommended?
As the cricoid cartilage is 2-3 cm caudad to the larynx, for purely anatomical reasons CP must be expected to hinder application of optimal external laryngeal pressure, 15 thereby increasing the chance of poor laryngoscopic view.
What is the role of cricoid pressure?
Cricoid pressure, also known as the Sellick manoeuvre or Sellick maneuver, is a technique used in endotracheal intubation to try to reduce the risk of regurgitation. The technique involves the application of pressure to the cricoid cartilage at the neck, thus occluding the esophagus which passes directly behind it.
What maneuver is done at the beginning of intubation to prevent aspiration?
Cricoid pressure is a technique that has become part of rapid sequence intubation to prevent aspiration of gastric contents.
How do you prevent aspiration during intubation?
Laboratory studies have suggested that the lateral Trendelenburg position is effective in preventing ventilator-associated pneumonia. [18,19] Pulmonary aspiration may be prevented during intubation attempt by the use of a combination of the head-down tilt and the semi-lateral position.
When should cricoid pressure be used?
Cricoid pressure to occlude the upper end of the oesophagus, also called the Sellick manoeuvre, may be used to decrease the risk of pulmonary aspiration of gastric contents during intubation for rapid induction of anaesthesia. Effective and safe use of the technique requires training and experience.
When do you apply cricoid pressure?
Cricoid pressure should be performed during induction of anaesthesia for both emergency surgery (full stomach) and for elective surgery when lower oesophageal sphincter is likely to be incompetent, (e.g. last half of pregnancy or gastro oesophageal reflux disease possible), and in patients with delayed gastric emptying ...
Which complication is prevented when cricoid pressure is applied during intubation?
Because cricoid pressure is used during intubation to reduce the risk of pulmonary aspiration, it is important to understand the prevalence and risk factors for this complication.
When should cricoid pressure be used in ACLS?
The routine use of cricoid pressure during intubation is no longer recommended. To maximize the chance of good resuscitation outcomes, epinephrine should be administered as early as possible, ideally within 5 minutes of the start of cardiac arrest from a nonshockable rhythm (asystole and pulseless electrical activity).
How do you prevent anesthesia aspiration?
Obstetrical patients and patients requiring emergency surgery most often have a "full stomach." Prevention of aspiration in such patients can be approached positively, by inserting an endotracheal tube before induction of general anesthesia, or negatively, avoiding general anethesia and substituting "conduction" ...
How do I stop aspiration?
Preventing AspirationAvoid distractions when you're eating and drinking, such as talking on the phone or watching TV.Cut your food into small, bite-sized pieces. ... Eat and drink slowly.Sit up straight when eating or drinking, if you can.If you're eating or drinking in bed, use a wedge pillow to lift yourself up.More items...•
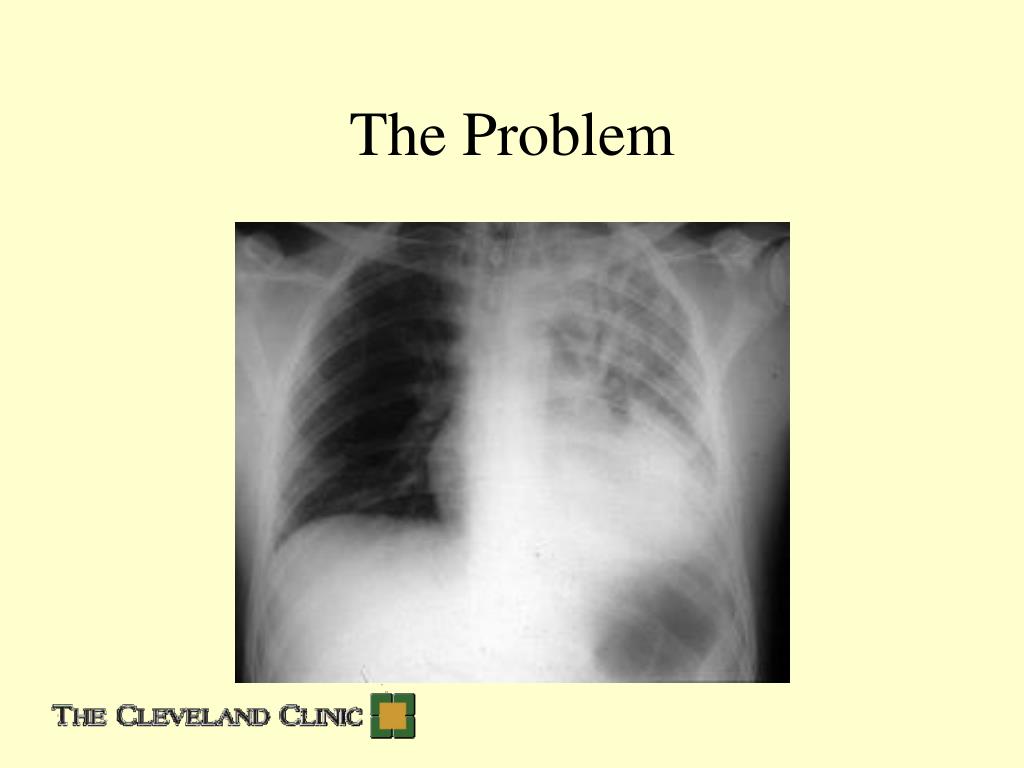
What happens if you aspirate during intubation?
While anesthesia is generally safe, respiratory complications such as anesthesia-related aspiration can be fatal. Occurring as often as 1 in every 2–3,000 operations requiring anesthesia,3 almost half of all patients who aspirate during surgery develop a related lung-injury, such as pneumonitis or aspiration pneumonia.
What is the best position to prevent aspiration?
Body positions that minimize aspiration include the reclining position, chin down, head rotation, side inclination, the recumbent position, and combinations of these. Patients with severe dysphagia often use a 30° reclining position.
What is the sniffing position?
Background: The sniffing position, a combination of flexion of the neck and extension of the head, is considered to be suitable for the performance of endotracheal intubation. To place a patient in this position, anesthesiologists usually put a pillow under a patient's occiput.
What are the steps for intubation?
PreparationAirway Evaluation. Time permitting, the first step in preparation is to perform an airway evaluation, which includes a history of intubation and difficult intubations. ... Positioning. ... Endotracheal Tube. ... Medications. ... Pre-Oxygenation. ... Apneic Oxygenation.
How do I stop aspiration?
Preventing AspirationAvoid distractions when you're eating and drinking, such as talking on the phone or watching TV.Cut your food into small, bite-sized pieces. ... Eat and drink slowly.Sit up straight when eating or drinking, if you can.If you're eating or drinking in bed, use a wedge pillow to lift yourself up.More items...•
Participation eligibility
Participant eligibility includes age, gender, type and stage of disease, and previous treatments or health concerns. Guidelines differ from study to study, and identify who can or cannot participate. There is no guarantee that every individual who qualifies and wants to participate in a trial will be enrolled.
Participating Mayo Clinic locations
Study statuses change often. Please contact the study team for the most up-to-date information regarding possible participation.
What is cricoid pressure?
cricoid pressure refers to digital pressure against the cricoid cartilage of the larynx, pushing it backwards with the intention of oesophageal compression against the vertebrae and prevention of passive regurgitation of gastric and oesophageal contents. the cricoid cartilage is the only complete ring-shaped cartilage in respiratory tract, ...
When must cricoid pressure be released?
If used, cricoid pressure must be released if there is vomiting, if there is difficulty visualising the cords, if BVM ventilations are required or if an LMA is to be placed
What is the objective of oesophageal compression?
objective is to achieve oesophageal compression against the vertebrae thus preventing passive regurgitation of gastric and oesophageal contents
How to identify cricoid cartilage?
identify cricoid cartilage (C6 level, find thyroid cartilage and move inferiorly to find cricothyroid membrane and then feel cricoid caudal to membrane) place index finger over cartilage. then place thumb and middle finger on either side. apply moderate pressure whilst patient awake with 10N of force.
Is cricoid pressure a standard part of airway management during intubation?
Cricoid pressure should not be a standard part of airway management during intubation (for instance it is not routinely recommended in the NSW HEMS prehospital RSI manual) This is an example of an intervention introduced with little evidence, handed down from teacher to student over the years as a pseudoaxiom.
Is cricoid pressure a risk for aspiration?
some argue that this is irrelevant as cricoid pressure is designed to occlude the upper not lower esophagus, however if cricoid pressure is released due to a difficult laryngos copic view there may be a higher risk of aspiration. aspiration despite cricoid pressure is well documented in anesthestic and EM literature.
Is cricoid pressure used in English?
Cricoid pressure is widely used in English-speaking countries despite a lack of evidence, whereas it is rarely or never used by practitioners in some European countries.
What are the complications of cricoid pressure?
Cricoid pressure–associated complications have also been alleged, such as airway obstruction leading to interference with manual ventilation, laryngeal visualization, tracheal intubation, placement of supraglottic devices, and relaxation of the lower esophageal sphincter. This review synthesizes available information to identify, address, and attempt to resolve the controversies related to cricoid pressure. The effective use of cricoid pressure requires that the applied force is sufficient to occlude the esophageal entrance while avoiding airway-related complications. Most of these complications are caused by excessive or inadequate force or by misapplication of cricoid pressure. Because a simple-to-use and reliable cricoid pressure device is not commercially available, regular training of personnel, using technology-enhanced cricoid pressure simulation, is required. The current status of cricoid pressure and objectives for future cricoid pressure–related research are also discussed.
How rare is CP aspiration?
Early reports supporting the effectiveness of CP have been criticized because they were based primarily on cadaver studies 16–18 and single-case reports. 50 Critics of the maneuver also argue against the need for CP since perioperative aspiration is rare—an incidence between 0.014% and 0.1% for adults and a slightly higher incidence in pediatric patients are generally accepted. 51–63 However, the incidence of aspiration has been shown to be higher in patients undergoing emergency surgery, 58, 60 with American Society of Anesthesiologist physical status 3 and 4, 58, 60 emergency intubations, 42, 64–68 and repeated intubation attempts. 68 A review of 2,833 emergency tracheal intubations revealed a 1.9% incidence of aspiration when laryngoscopy was performed once or twice as compared with an incidence of 22% with three or more attempts. 68 Because of the complexity of airway management in critically ill and trauma patients and the possibility of aspiration before intubation or after extubation, the true incidence is difficult to assess in these patients. 62–74 Although most reports indicate that mortality from perioperative aspiration is rare, values as high as 4.6% have been reported. 62, 74, 75
What part of the alimentary tract is compressed by CP?
24 evaluated the maneuver in the sniffing, neutral, and extended head positions using magnetic resonance imaging (MRI). They found that the part of the alimentary tract compressed by CP is actually the postcricoid hypopharynx. They also observed that, unlike the cervical esophagus, the postcricoid hypopharynx moved with the cricoid cartilage as an anatomical unit during CP. 24 These findings confirmed Sellick’s original observation that CP compresses the conduit between the stomach and the pharynx. Furthermore, they demonstrated that compression of the postcricoid hypopharynx during CP occurs in spite of the variable position of the cricoid cartilage in relation to the vertebral body (midline or lateral position). 24 The postcricoid hypopharynx is also referred to as the cricopharyngeus, which is a major component of the upper esophageal sphincter. Recently, the postcricoid hypopharynx has been referred to as the esophageal entrance. 25
How effective is CP in achalasia?
In achalasia, the dilated esophagus is wider than the area under the cricoid cartilage. 77–79 Nonetheless, it is probable that the maneuver would be effective since the compression area is much larger than the surface area of the cricoid cartilage. 77 In Zenker diverticulum, the effectiveness of CP may depend on the location of the pouch and its neck ( Fig. 1 ). 80 If the neck of the pouch is posterior to the cricoid cartilage, CP will occlude the neck, and the contents of the pouch will not be extruded into the pharynx. 80 Conversely, if the pouch is at the level of the cricoid cartilage (because it has no neck), CP may compress the pouch, spilling its contents into the pharynx. 80
How effective is CP in preventing regurgitation?
Several lines of evidence raise questions about the effectiveness of CP in preventing regurgitation and aspiration. First, case reports provide examples of fatal aspiration in spite of CP. 37, 38 Second, surveys revealed that 11 to 14% of anesthesia providers and assistants witnessed regurgitation, usually once in their career, even though CP was applied. 39, 40 Third, a 30-yr review of closed malpractice claims reported aspiration in 67 cases despite the use of CP in 17 of these cases. 41 Fourth, in a prospective study of emergency airway management in 297 critically ill patients, 12 showed newer or unexpected radiographic infiltrates even though CP was applied in nine patients. 42 Fifth, in a report of almost 5,000 general anesthetics for obstetrical patients in Malawi, 11 deaths attributable to regurgitation occurred despite application of CP in nine patients. 43 Critics of the CP maneuver have cited the findings listed above as proof of its unreliability. 7–12 Conversely, proponents of the maneuver suggest that these failures could be due to improper application, early release, application by untrained personnel, and the possibility of aspiration before anesthetic induction or after extubation. 28, 44–48 They also claim that the incidence of aspiration would be higher if CP was not used. 49
Why is CP used in resuscitation?
As early as 1774, CP was used to prevent gastric distension during resuscitation of drowning victims. 19 In his seminal publication, Sellick 1, 2 suggested that the maneuver can be useful to avoid gastric insufflation during positive-pressure ventilation.
Is a CP effective in closing the esophageal entrance?
Zeidan et al. 25 provided real-time visual and dynamic evidence for the effectiveness of CP in closing the esophageal entrance in anesthetized and paralyzed patients. In this study, the Glidescope (R) Video Laryngoscope (GVL; Verathon Medical Canada ULC, Canada) allowed the panoramic view of the esophageal entrance and the laryngeal structures. Closure of the esophageal entrance was observed, and it was not possible to insert a gastric tube when 30-N cricoid force was exerted. These findings were independent of the location of the esophageal entrance in relation to the glottis.