What are the stages of inflammation?
- Initial tissue damage and activation of local inflammatory factors
- Immune activation in the CNS and remodeling of the blood–brain barrier (BBB)
- Recruitment of circulating leukocytes and subsequent secondary immunopathology
- Engagement of anti-inflammatory responses that promote tissue repair and restoration of neurologic function
What are the steps of tissue repair?
What are the three basic steps in tissue repair?
- Inflammation, Organization, Regeneration. What are the three steps of tissue repair?
- Inflammation. Macrophages, mast cells, and injured tissue cells release inflammatory chemicals.
- Organization. Blood clot is replaced by granulation tissue.
- Regeneration.
- Fibrosis.
What is tissue response to inflammation?
This response includes the release of antibodies and proteins, as well as increased blood flow to the damaged area. The whole process usually lasts for a few hours or days in the case of acute inflammation. Chronic inflammation happens when this response lingers, leaving your body in a constant state of alert.
What are the four hallmarks of inflammation in tissue?
The four hallmarks of inflammation in tissue are: a. heat, swelling,redness, and itching. pain, sweeling, heat, and - Answered by a verified Veterinarian
Does inflammation heal tissue?
When your body activates your immune system, it sends out inflammatory cells. These cells attack bacteria or heal damaged tissue. If your body sends out inflammatory cells when you are not sick or injured, you may have chronic inflammation.
Does inflammation initiate healing?
The inflammatory response following tissue injury plays important roles both in normal and pathological healing. Immediately after injury, the innate immune system is activated, setting in motion a local inflammatory response that includes the recruitment of inflammatory cells from the circulation.
How does inflammation help tissue Repair?
Repair of injured tissues is dependent on activation of an inflammatory reaction. Release of danger signals by dying cells activates innate immune pathways, ultimately leading to induction of chemokines and proinflammatory cytokines at the site of the injury.
What triggers tissue repair?
Tissue repair is modulated by a variety of factors, including age, disease, nutrition, species, and strain, which cause marked changes in susceptibility and toxic outcome.
Is inflammation good for healing muscles?
Although inflammation was originally believed to interfere with skeletal muscle regeneration, several recent studies have highlighted the beneficial effects of inflammatory cells on muscle healing.
Does swelling promote healing?
While most people become alarmed when the body shows signs of swelling, it's important to remember that this is a natural part of the healing process. When swelling occurs, it's just the body requesting reinforcements to speed up the healing process.
Does inflammation delay healing?
Indeed, in experimental models of repair, inflammation has been shown to delay healing and to result in increased scarring. Furthermore, chronic inflammation, a hallmark of the non-healing wound, predisposes tissue to cancer development.
Why is inflammation important in healing?
Inflammation occurs in response to physical trauma, intense heat and irritating chemicals, as well as to infection by viruses and bacteria. The inflammatory response: (1) prevents the spread of damaging agents to nearby tissues (2) disposes of cell debris and pathogens and (3) sets the stage for the repair process.
How do you repair damaged tissue?
The Repair Phase As debris from damaged tissues is removed, the inflammatory phase gradually subsides and the tissue begins to repair and rebuild itself. New blood vessels grow into the area to deliver repair “supplies” and remove waste. Scar tissue begins to form.
What promotes tissue healing and repair?
The cell cycle. One of the main actions in the tissue repair script is cell proliferation. In order to heal after injury—whether by regeneration or scarring—cells must enter and progress through the cell cycle, a tightly-regulated process that consists of two main activities: DNA replication and mitosis.
When does tissue Repair begin?
Fibroblastic Repair/Subacute Phase: Can begin at Day 4, up to 6 weeks. This phase begins as the inflammation settles down and your body begins to repair the damaged tissue by laying down collagen.
What are the stimuli that promote tissue healing and repair?
The factors discussed include oxygenation, infection, age and sex hormones, stress, diabetes, obesity, medications, alcoholism, smoking, and nutrition. A better understanding of the influence of these factors on repair may lead to therapeutics that improve wound healing and resolve impaired wounds.
Why is inflammation important in healing?
Inflammation occurs in response to physical trauma, intense heat and irritating chemicals, as well as to infection by viruses and bacteria. The inflammatory response: (1) prevents the spread of damaging agents to nearby tissues (2) disposes of cell debris and pathogens and (3) sets the stage for the repair process.
Does reducing inflammation slow healing?
No, in most cases anti-inflammatory drugs (like ibuprofen or naproxen) don't help healing. In fact, in some cases it may even delay healing.
What is the purpose of inflammation?
Inflammation is the immune system's response to harmful stimuli, such as pathogens, damaged cells, toxic compounds, or irradiation [1], and acts by removing injurious stimuli and initiating the healing process [2]. Inflammation is therefore a defense mechanism that is vital to health [3].
Do anti inflammatories delay healing?
Among these factors, non-steroidal anti-inflammatory drugs (NSAIDs) can inhibit or impair bone healing process because their influence is critical on the stages of healing including inflammation, coagulation and angiogenesis and finally on the clinical outcome.
Does inflammation repair damaged tissue?
Inflammation underlies many chronic and degenerative diseases, but it also mitigates infections, clears damaged cells and initiates tissue repair.
Why is inflammation important in tissue repair?
Inflammation plays an important role in tissue repair and regeneration. Recent work reveals that inflammatory signaling increases DNA accessibility so as to promote phenotypic fluidity in response to injury.
Does inflammation speed up tissue repair?
Recently, scientists have discovered a new component of the inflammatory reaction, called the “pro-resolving” program, which stimulates wound healing and repair of the damaged tissue or organ.
What does inflammation do to tissue?
When inflammation happens, chemicals from your body’s white blood cells enter your blood or tissues to protect your body from invaders. This raises the blood flow to the area of injury or infection. It can cause redness and warmth. Some of the chemicals cause fluid to leak into your tissues, resulting in swelling.
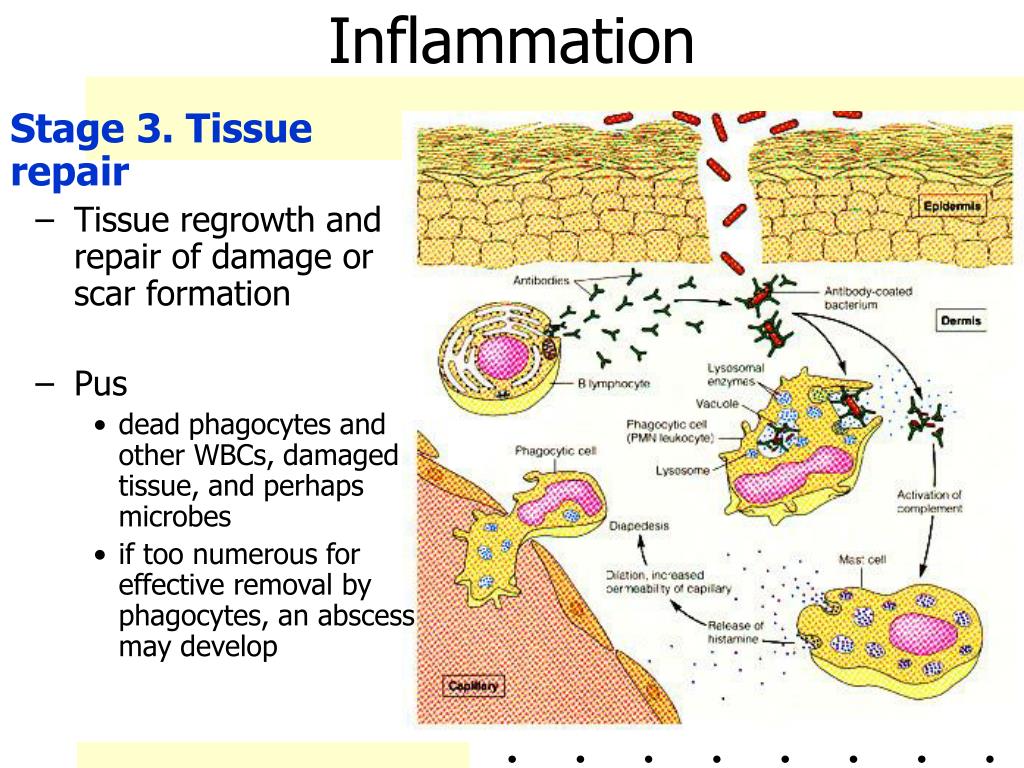
What are the 3 stages of inflammation?
The Three Stages of Inflammation Written by Christina Eng – Physiotherapist, Clinical Pilates Instructor. Phase 1: Inflammatory Response. Healing of acute injuries begins with the acute vascular inflammatory response. Phase 2: Repair and Regeneration. Phase 3: Remodelling and Maturation.
Can you reverse inflammation?
You can control — and even reverse — inflammation through a healthy, anti-inflammatory diet and lifestyle. People with a family history of health problems, such as heart disease or colon cancer, should talk to their physicians about lifestyle changes that support preventing disease by reducing inflammation.
What initiates tissue repair?
After containment of an injury, the tissue repair phase starts with removal of toxins and waste products. Clotting (coagulation) reduces blood loss from damaged blood vessels and forms a network of fibrin proteins that trap blood cells and bind the edges of the wound together.
Why is inflammation important?
In other words, inflammation is a protective response to rid the body of the cause of cell injury and the resultant necrotic cells that cell injury produces . Although the processes of acute and chronic inflammation are an important protective mechanism used by the body to deal with potentially damaging agents, they are potentially damaging to ...
How long does inflammation last?
Acute inflammation has a rapid onset, lasts for minutes to days, and is characterized by exudation of fluid and protein from vessels and emigration of neutrophils. Acute inflammation is a protective process that is designed to rid the body of the inciting agent and set up the process of repair.
What are the general concepts of acute and chronic inflammation?
Overview: The body must undergo changes locally through vasodilation and increased vascular permeability in the area of the agent inciting the inflammatory reaction to allow white blood cells to accumulate. The white blood cells must then leave the blood vessel, cross the basement membrane, ...
What happens when tissue damage is substantial?
Repair, which occurs when tissue damage is substantial or the normal tissue architecture cannot be regenerated successfully, results in the formation of a fibrous scar. Through the repair process, endothelial cells give rise to new blood vessels, and cells called fibroblasts grow to form a loose framework of connective tissue.
What happens to damaged cells during the healing process?
Healing and repair. During the healing process, damaged cells capable of proliferation regenerate. Different types of cells vary in their ability to regenerate. Some cells, such as epithelial cells, regenerate easily, whereas others, such as liver cells, do not normally proliferate but can be stimulated to do so after damage has occurred.
What causes suppuration in the body?
The most common cause of suppuration is infection with the pyogenic (pus-producing) bacteria, such as Staphylococcus and Streptococcus. Once pus begins to collect in a tissue, it becomes surrounded by a membrane, giving rise to a structure called an abscess.
What happens if you don't replicate the original framework of an organ?
In some cases, the failure to replicate the original framework of an organ can lead to disease. This is the case in cirrhosis of the liver, in which regeneration of damaged tissue results in the construction of abnormal structures that can lead to hemorrhaging and death.
What is the process of pus formation?
The process of pus formation, called suppuration, occurs when the agent that provoked the inflammation is difficult to eliminate. Pus is a viscous liquid that consists mostly of dead and dying neutrophils and bacteria, cellular debris, and fluid leaked from blood vessels.
Can an abscess burst?
Sometimes a surgical incision is necessary to drain and eliminate it. Some abscesses, such as boils, can burst of their own accord. The abscess cavity then collapses, and the tissue is replaced through the process of repair. Load Next Page.
How long does it take for inflammation to heal?
Inflammation does not always require treatment. For acute inflammation, rest, ice and good wound care often relieve the discomfort in a few days.
How does inflammation affect the body?
Inflammation is an essential part of your body’s healing process. It occurs when inflammatory cells travel to the place of an injury or foreign body like bacteria. If inflammatory cells stay too long, it may lead to chronic inflammation. Chronic inflammation is a symptom of other health conditions, such as rheumatoid arthritis. Your healthcare provider may recommend medication or at-home management. You can reduce inflammation by eating anti-inflammatory foods and managing stress.
What happens when your body activates your immune system?
When your body activates your immune system, it sends out inflammatory cells. These cells attack bacteria or heal damaged tissue. If your body sends out inflammatory cells when you are not sick or injured, you may have chronic inflammation. Inflammation is a symptom of many chronic diseases, such as arthritis or Alzheimer’s disease.
What is the first response of the immune system?
Your immune system sends out its first responders: inflammatory cells and cytokines (substances that stimulate more inflammatory cells).
What diet should I follow for inflammation?
You may choose to follow an anti-inflammatory diet. Some research shows that people who follow a Mediterranean diet have lower levels of inflammation in their bodies.
What supplements can help with inflammation?
Supplements: Certain vitamins (vitamin A, vitamin C, vitamin D) and supplements (zinc) may reduce inflammation and enhance repair. For example, your healthcare provider may prescribe a fish oil supplement or vitamin (s). Or you may use spices with anti-inflammatory properties, such as turmeric, ginger or garlic.
What is the response to sudden body damage such as cutting your finger?
Acute inflammation: The response to sudden body damage, such as cutting your finger. To heal the cut, your body sends inflammatory cells to the injury. These cells start the healing process.
Abstract
Tissue repair after injury is a complex, metabolically demanding process. Depending on the tissue’s regenerative capacity and the quality of the inflammatory response, the outcome is generally imperfect, with some degree of fibrosis, which is defined by aberrant accumulation of collagenous connective tissue.
New insights emerging from live imaging of the wound response
The immune response to tissue damage and infection was first observed by Metchnikoff in his studies of translucent waterborne creatures in the early 20th century ( 4 ).
Model organism studies reveal some of the damage attractants and how inflammatory cells respond
At a fundamental cell biology level, we know that immune cells respond to attractant cues through Rho family small guanosine triphosphatase (GTPase) regulation of their actin cytoskeletons. If Rac is knocked down in Drosophila macrophages, they fail to make proper lamellae and efficiently migrate to the wound.
Resolving the inflammatory response
After healing is complete, the resolution of inflammation is not simply a passive process. Although there is clear evidence in mammalian wounds that many neutrophils undergo apoptosis at the site of inflammation, there is also evidence for the reverse migration of zebrafish neutrophils from sites of inflammation.
Reliance of tissue repair and regeneration on the wound inflammatory response
The role of the inflammatory response, and specifically the function of macrophages, is not clear-cut. Knockdown of macrophages in rabbits with anti-macrophage serum led to severely impaired healing ( 17 ), whereas no major impact was observed when neutrophils were depleted.
Regenerative inflammation: An evolutionarily conserved mechanism
In lower vertebrates that regenerate whole appendages, such as fins and limbs, and even regions of damaged central nervous system, most studies suggest that inflammation is necessary.
Dysregulated tissue repair and inflammation promote pathological fibrosis
Although the wound inflammatory response drives many aspects of tissue repair and regeneration, it can become dysregulated or chronic, and this may lead to the development of pathological fibrosis or scarring that can disrupt normal tissue architecture and function ( 29 ).
Why is inflammation important?
Inflammation represents an essential survival mechanism that helps the body fight off hostile microbes and repair damaged tissue. Yet there is another side of inflammation that can be harmful rather than helpful to human health.
What is the role of chronic inflammation?
Chronic inflammation plays a central role in some of the most challenging diseases of our time, including rheumatoid arthritis, cancer, heart disease, diabetes, asthma, and even Alzheimer’s . This report will examine the role that chronic inflammation plays in these conditions, and will also provide information on the breadth of drugs currently available to alleviate symptoms. Drug choices range from simple aspirin, a nonsteroidal anti-inflammatory drug that’s been available for more than a century, to disease-modifying drugs and so-called biologics that promise more targeted treatments.
What is the role of the immune system in the body?
Unchecked, the immune system prompts white blood cells to attack nearby healthy tissues and organs, setting up a chronic inflammatory process that plays a central role in some of the most challenging diseases of our time , including rheumatoid arthritis, cancer, heart disease, diabetes, asthma, and even Alzheimer’s.
How long does it take for inflammation to go away?
Acute inflammation comes on rapidly, usually within minutes, but is generally short-lived. Many of the mechanisms that spring into action to destroy invading microbes switch gears to cart away dead cells and repair damaged ones. This cycle returns the affected area to a state of balance, and inflammation dissipates within a few hours or days.
What is the final stage of the inflammatory process?
The final stage of the inflammatory process is termination and repair. Once the offending pathogen or substance has been eliminated, tissue repair begins. The surviving cells regenerate to replace damaged ones. Cells that are part of less complex structures, such as the surface of the skin, regrow easily.
How long does inflammation last?
Chronic inflammation often begins with the same cellular response, but morphs into a lingering state that persists for months or years when the immune system response fails to eliminate the problem. Alternatively, the inflammation may stay active even after the initial threat has been eliminated.
What happens if you cut your finger and twisted your knee?
If you’ve ever twisted your knee, cut your finger, or been stung by an insect, you have firsthand experience with inflammation. The familiar sensations of pain, redness, swelling, and heat that result from an injury or infection are hallmarks of the inflammatory process.
What causes inflammation to occur?
Acute inflammation starts after a specific injury that will cause soluble mediators like cytokines, acute phase proteins, and chemokines to promote the migration of neutrophils and macrophages to the area of inflammation.[3] These cells are part of natural innate immunity that can take an active role in acute inflammation. If this inflammation does not resolve after six weeks, this will cause the acute inflammation to develop from subacute to the chronic form of inflammation with the migration of T lymphocytes and plasma cells to the site of inflammation. If this persists with no recovery, then tissue damage and fibrosis will ensue. Other varieties of cells, such as macrophages and monocytes, play a role in both acute and chronic inflammation. In this article, we will discuss "acute inflammation."
How to tell if you have inflammation?
There are five cardinal signs of inflammation, namely redness (rubor), heat (calor), swelling (tumor), pain (dolor), and loss of function (functio laesa). The sensation of heat is caused by the increased blood movement in dilated vessels into environmentally cooled extremities. This reaction will also lead to redness due to an increase in the number of erythrocytes passing through the injured area. The swelling of the area occurs due to an increase in the permeability and dilatation of the blood vessels. Pain is due to an increase in the pain mediators, either due to direct damage or resulting from an inflammatory response itself. Loss of function occurs due to either simple loss of mobility due to either edema or pain or replacement of the cells with scar tissue. [20]
What are the causes of inflammatory bowel disease?
Polygenic inflammatory bowel disease (IBDs) is characterized by an excessive inflammatory response to gut microbial flora. IBDs include Crohn disease (CD) and ulcerative colitis (UC). These two diseases are cytokine driven. Apart from that, other causes include non-infectious inflammation of the bowel. The system can recognize the microbial agent through the TLRs. These PAMPs that bind to the TLRs (mainly TLR4) activate the signaling pathways (NF-kB, MAPK) that cause the production of cytokines and chemokines to start the resistance to the infection. [19]
What are mediators in the inflammatory process?
The first group of mediators is the toll-like receptors (TLRs), which are membrane-spanning proteins found on the surfaces of the innate immune system cells like macrophages and dendritic cells. These single-pass membrane-spanning receptors recognize the pathogen-associated molecular patterns (PAMPs) or can recognize endogenous signals activated during tissue or cell damage known as danger-associated molecular patterns (DAMPS). To date, research has identified more than ten TLRs. An important example is the CD14 (cluster of differentiation 14), a co-receptor for TLR4, which is present on the surface of innate immune system cells preferentially expressed in macrophages, monocytes, and neutrophils. TLR4 can recognize the Lipopolysaccharide, which is the major component of the outer membrane of the gram-negative bacteria (PAMPs). Then the transmission of PAMPs and DAMPs are mediated by MyD88 (myeloid differentiation 88) along with the TLRs. Subsequently, the signaling will transmit through a specific cascade that leads to nuclear translocation of transcription factors, such as NF-kB, activator protein-1 (AP-1), or interferon regulatory factor 3(IRF3). [7][8][9]
What are the two groups of inflammatory inducers?
As an alternative, we could also divide the inflammatory inducers into two large groups, which are the infectious factors and the non-infectious factors.
What are the signs of inflammation?
This mechanism is non-specific and immediate.[1] There are five fundamental signs of inflammation that include: heat (calor), redness (rubor), swelling (tumor), pain (dolor), and loss of function (functio laesa). Inflammation can divide into three types based on the time of the process that responds to the injurious cause; acute which occurs immediately after injury and lasts for few days, chronic inflammation that may last for months or even years when acute inflammation fails to settle, and subacute which is a transformational period from acute to chronic which lasts from 2 to 6 weeks.[2]
Is inflammation an adaptive response?
Acute inflammation is an immediate, adaptive response with limited specificity caused by several noxious stimuli, such as infection and tissue damage (tissue necrosis). The controlled inflammatory response is generally beneficial, and this can be seen clearly in providing protection against infectious organisms, including mycobacterium tuberculosis, protozoa, fungi, and other parasites. However, it can become detrimental if not regulated, such as seen in septic shock.[4] The inflammatory pathway consists of a sequence of events involving inducers, sensors, mediators, and effectors. [5]
Which cells are involved in inflammation?
Following tissue injury, fibroblasts induce chemokine synthesis, which in turn activate chemotaxis of immune cells. Monocytes and macrophages undergo substantial phenotypic and functional changes to in order to mediate the initiation, maintenance, and resolution phases of tissue repair. Activated macrophages release proinflammatory factors (cytokines such as IL-1 or TNFα) causing vasodilatation and increased permeability of the blood vessels that facilitates Neutrophils migration.
Which cell is primarily the first inflammatory cell to respond and migrate towards the site of inflammation?
Neutrophils are primarily the first inflammatory cells to one respond and migrate towards the site of inflammation. CB2 activation suppresses both adhesion to the endothelium and transmigration through blood vessels towards the site of the injury.
What are the roles of macrophages in tissue repair?
Macrophages exert pivotal regulatory activity at all stages of tissue repair and fibrosis. Following tissue injury, local gradient of chemokine and adhesion molecules cause a recruitment of inflammatory monocytes, macrophage precursors from the bone marrow. Growth factors and cytokines released in the local tissue microenvironment stimulate proliferation and differentiation of the recruited and resident macrophage populations. Activated macrophages further release chemokines, matrix metalloproteinases, and other inflammatory factors that initiate the cellular response upon tissue injury. They also stimulate fibroblast differentiation into myofibroblasts that are responsible for wound contraction and closure. CB2 stimulation suppress macrophage activation and proliferation. Moreover CB2 activation stimulates macrophage apoptosis and decrease production of pro-inflammatory cytokines, chemokines and reactive oxygen species.
Does THC inhibit smooth muscle proliferation?
Vascular smooth muscle proliferation and migration are critical events in the pathogenesis of atherosclerosis and are directly implicated in the failure of clinical interventions used to treat patients with coronary heart disease. Delta9-tetrahydrocannabinol (THC), a cannabis constituent, has recently been demonstrated to inhibit atherosclerosis progression in a mouse model of the disease, presumably via CB 2 receptor stimulation. Interestingly, the expression of CB 2 receptors could be enhanced by the pro-inflammatory cytokine TNF-α in vascular smooth muscle cell. CB 2 receptor stimulation attenuates TNF-α-induced (but not basal) cell proliferation as well as cell migration of vascular smooth muscle cells.
