Since labetalol can be administered orally, is economical, has low toxicity potential, does not require specialized training to administer or monitor, and decreases CPP, it may be an ideal agent for controlling blood pressure (BP
BP
BP plc is a British multinational oil and gas company headquartered in London, United Kingdom. It is one of the world's seven oil and gas "supermajors", whose performance in 2012 made it the world's sixth-largest oil and gas company, the sixth-largest energy company by market capitaliz…
Does labetalol lower heart rate?
Monitoring esophageal Doppler hemodynamics confirms and underscores the fact that labetalol’s stronger beta-1 blocking decreases heart rate and contractility preferentially. We have seen profound effects on contractility with this drug, including frequent decreases in aortic peak velocities by 50% and greater.
Is it safe to take labetalol during pregnancy?
Use of labetalol in pregnancy is common and there is no concern that it causes harm. Labetalol belongs to a family of medicines called beta blockers. Studies have not shown that beta blockers cause birth defects, stillbirth, or preterm birth. Women taking beta blockers may be more likely to have a small baby.
How much labetalol to give IV?
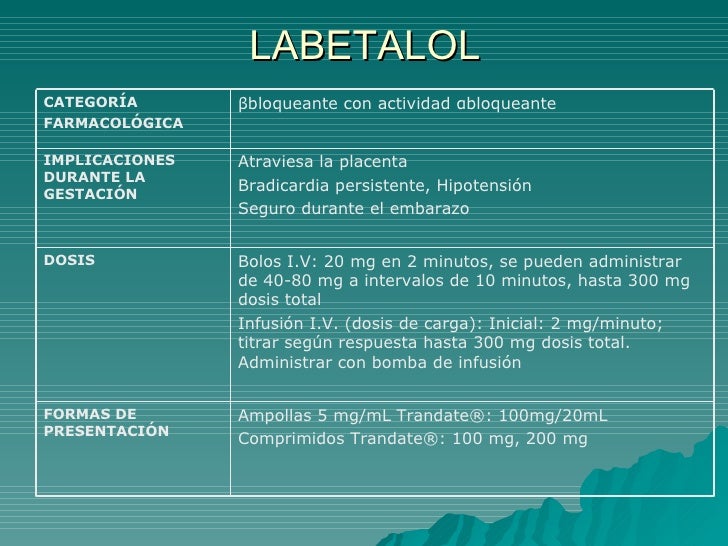
The dosage for labetalol is 20 mg IV with repeat doses (40, 80, 80, and 80 mg) every 10 minutes up to a maximum dose of 300 mg. Decreases in BP are observed after 5 minutes (in contrast to the slower onset of action of hydralazine), and the drug results in less overshoot hypertension than does hydralazine. Why is mgso4 given in eclampsia?
What is labetalol used to treat?
Used to lower high blood pressure (hypertension). The injectable form of labetalol is only used to treat severe hypertension. Only mildly slows heart rate. Blunts the increase in blood pressure and heart rate that occurs during exercise without affecting how well the lungs are perfused with blood.
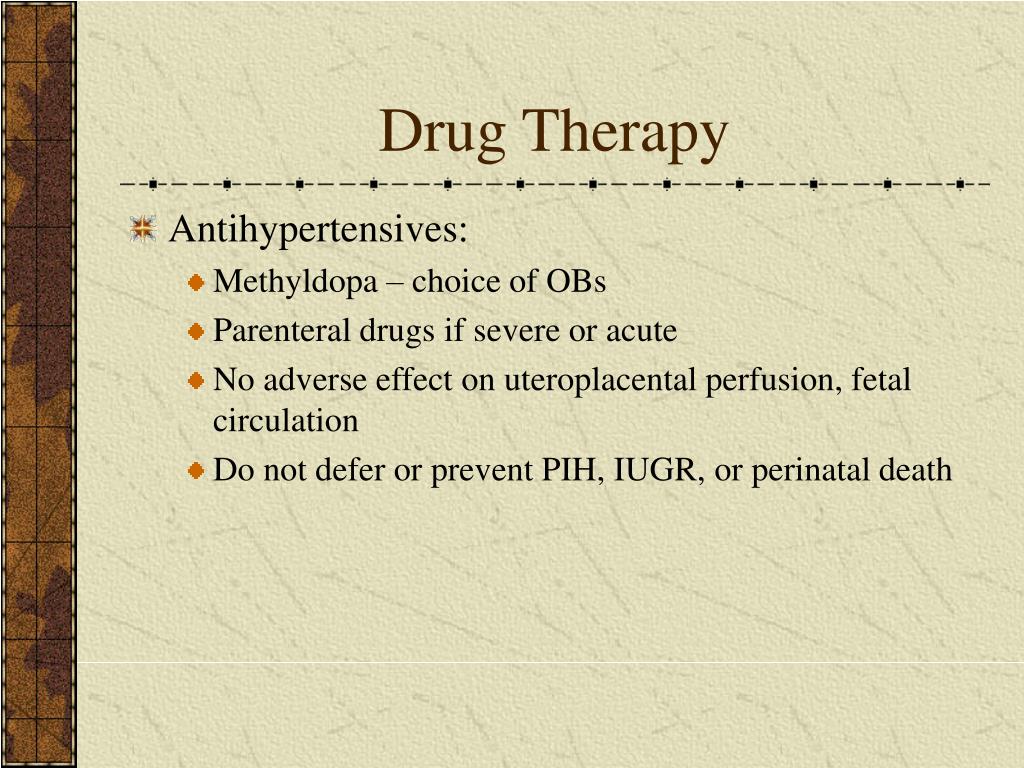
Can blood pressure medication prevent preeclampsia?
Medications are available to reduce blood pressure and manage the symptoms of the disease, but ultimately, the delivery of your baby is recommended to stop progression of preeclampsia and lead to resolution.
What is the drug of choice for preeclampsia?
The drug of choice for the prevention and control of maternal seizures in patients with severe preeclampsia or eclampsia during the peripartum period is i.v. magnesium sulfate. Its mechanism of action for the treatment of eclampsia is not well understood.
Can you prevent preeclampsia while pregnant?
Currently, there is no sure way to prevent preeclampsia. Some contributing factors to high blood pressure can be controlled and some can't. Follow your doctor's instruction about diet and exercise.
Can blood pressure meds mask preeclampsia?
As in women with chronic hypertension, antihypertensive medications should be prescribed with the goal of preventing maternal consequences of severe hypertension, because there is no evidence that targeted BP control prevents preeclampsia.
What BP is considered preeclampsia?
Symptoms. Signs of preeclampsia in a pregnant woman include: Blood pressure of 140/90. Systolic blood pressure that rises by 30 mm Hg or more even it if is less than 140.
What is the most effective cure for preeclampsia?
Pre-eclampsia can only be cured by delivering the baby. If you have pre-eclampsia, you'll be closely monitored until it's possible to deliver the baby. Once diagnosed, you'll be referred to a hospital specialist for further assessment and any necessary treatment.
What were your first signs of preeclampsia?
The first signs of preeclampsia are often detected during routine prenatal visits with a health care provider. Along with high blood pressure, preeclampsia signs and symptoms may include: Excess protein in urine (proteinuria) or other signs of kidney problems. Decreased levels of platelets in blood (thrombocytopenia)
What triggers preeclampsia?
There are a number of things that can increase your chances of developing pre-eclampsia, such as: having diabetes, high blood pressure or kidney disease before you were pregnant. having an autoimmune condition, such as lupus or antiphospholipid syndrome. having high blood pressure or pre-eclampsia in a previous ...
What are the early warning signs of preeclampsia?
Preeclampsia SymptomsHigh blood pressure during pregnancy.Blurred vision.Headache.Swelling of the face, hands and feet.Upper abdominal pain.Vomiting.Shortness of breath.HELLP syndrome (severe form of preeclampsia)
How much labetalol should I take for preeclampsia?
Initial therapy should consist of labetalol 20 mg or hydralazine 5- 10 mg IV over 2 minutes. Hydralazine begins to have an effect within 5-20 minutes with its maximum effect occurring at 15-30 minutes. Labetalol onset is within 2-5 minutes and has its maximum effect after 5 minutes.
Is blood pressure always high with preeclampsia?
Preeclampsia is a serious blood pressure condition that develops during pregnancy. People with preeclampsia often have high blood pressure (hypertension) and high levels of protein in their urine (proteinuria). Preeclampsia typically develops after the 20th week of pregnancy.
When should a pregnant woman take labetalol?
1 The National Institute for Health and Care Excellence (NICE) recommends labetalol as first-line antihypertensive treatment for non-severe (<160/110 mm Hg) gestational hypertension and pre-eclampsia once blood pressure exceeds 150/100 mm Hg.
What is the standard treatment for eclampsia?
Eclampsia Treatment Immediate treatment, usually in a hospital, is needed to stop the mother's seizures, treat blood pressure levels that are too high, and deliver the fetus. Magnesium sulfate (a type of mineral) may be given to treat active seizures and prevent future seizures.
What drugs are given to eclampsia?
The drug of choice to treat and prevent eclampsia is magnesium sulfate. Familiarity with second-line medications phenytoin and diazepam/lorazepam is required for cases in which magnesium sulfate may be contraindicated (eg, myasthenia gravis) or ineffective.
Why is mgso4 given in eclampsia?
Magnesium sulfate therapy is used to prevent seizures in women with preeclampsia. It can also help prolong a pregnancy for up to two days. This allows drugs that speed up your baby's lung development to be administered.
Why methyldopa is safe in pregnancy?
Methyldopa can prevent the complications caused by hypertension (high blood pressure) in pregnancy, and a related condition called pre-eclampsia. These complications include preterm birth, low birth weight in the baby, and illness in both the mother and baby which is sometimes serious.
How many tablets of labetalol are given?
Patients randomized to labetalol will receive two 100 mg tablets orally. The labetalol tablets (200 mg) will be repeated every 6 hours, unless the patient is hypotensive (BP < 90 mmHg systolic and/or 60 mmHg diastolic). The tablets will be swallowed with a maximum of 10cc of water. In those patients where the clinical team desires a more rapid intravenous dosing, a single 20mg of labetalol will be given before the oral dose is taken. Labetalol therapy will be continued for 24 hours post delivery.
Why do we need an IND number for labetalol?
This IND number is only necessary for grant funding. The FDA has assessed this study and does not feel that it required an IND number for clinical reasons since labetalol is already an approved antihypertensive medication. The only reason that an IND number was requested was to allow us to satisfy the requirements for various Federal Funding agencies. The foreign institutions will not require an IND number but will all require an active approval from their Institutional Review Board.
What is the cause of perinatal morbidity and mortality?
Eclampsia is a major cause of perinatal morbidity and mortality. The pathophysiology is not known but magnetic resonance imaging (MRI) and Doppler data suggest that overperfusion of the cerebral tissues is a major etiologic factor. Hypertensive encephalopathy from overperfusion, and vascular damage from excessive arterial pressure (cerebral barotrauma) are believed to lead to vasogenic and cytotoxic cerebral edema, with resultant neuronal anomalies, seizure activity and cerebral bleeding if left unchecked. Doppler data have shown that cerebral perfusion pressure (CPP) is abnormally increased in severe preeclampsia and that autoregulation of the middle cerebral artery is affected by this condition leading to increased CPP. Magnesium sulfate (MgSO4) is the most widely accepted eclampsia treatment and prophylactic agent, and it has been used in the USA since the 1950's. Despite widespread use, its mechanism of action is unknown. MgSO4 is given intravenously or intramuscularly and requires specialized nursing training and monitoring to minimize toxicity from respiratory and cardiac depression. Labetalol, a combined alpha and beta blocker, has been used for many years to safely treat hypertension in preeclamptic women, and is now known to reduce CPP in women with preeclampsia. In the United Kingdom labetalol was for many years used as the sole agent in treating preeclampsia, and the rate of seizure was no different to that reported in the USA with MgSO4. Since labetalol can be administered orally, is economical, has low toxicity potential, does not require specialized training to administer or monitor, and decreases CPP, it may be an ideal agent for controlling blood pressure (BP) and decreasing the incidence of eclampsia in women with preeclampsia. The current study is a multicenter, randomized, controlled trial to compare the anti-seizure effect of parenteral MgSO4 versus oral labetalol in hypertensive pregnant women who are eligible for MgSO4 therapy. The primary outcome measure is eclampsia, and the secondary outcome measures include blood pressure control, and relevant antenatal, intrapartum, and postnatal maternal and fetal/neonatal parameters including adverse effects and complications. Inclusion criteria are deliberately broad in order to make the study clinically relevant. Hypertensive pregnant women, in whom the decision for delivery has been made, will be enrolled after written, informed consent. Patients will be randomized to receive MgSO4 therapy as given in their institution, versus oral labetalol (200mg/q6 hours), from enrollment in the study until 24 hours post delivery. There will be 4000 patients in each arm of the study and analysis will be by intention-to-treat. The study is powered to show both therapeutic superiority as well as clinical equivalence. This study has the potential to change the way preeclampsia is managed, and will represent a major advance in terms of the availability and safety of prophylactic therapy, especially in developing nations where MgSO4 is underutilized due to cost constraints.
What is the most commonly used treatment for eclampsia?
Magnesium sulfate ( MgSO4) is the most widely accepted eclampsia treatment and prophylactic agent, and it has been used in the USA since the 1950's. Despite widespread use, its mechanism of action is unknown.
What type of anesthesia is used for delivery?
Type of anesthesia administered (none, local infiltration for delivery only, epidural for labor, epidural for delivery, spinal for delivery, combined/spinal epidural for labor and delivery, general anesthesia for delivery).
Does preeclampsia cause increased CPP?
Doppler data have shown that cerebral perfusion pressure (CPP) is abnormally increased in severe preeclampsia and that autoregulation of the middle cerebral artery is affected by this condition leading to increased CPP.
Can labetalol be administered orally?
Since labetalol can be administered orally, is economical, has low toxicity potential, does not require specialized training to administer or monitor, and decreases CPP, it may be an ideal agent for controlling blood pressure (BP) and decreasing the incidence of eclampsia in women with preeclampsia.
What is labetalol used for?
As labetalol is typically used to treat acute hypertension, whether it presents in the emergency department or an outpatient clinic, an interprofessional team approach and effective communication are essential for quality patient care. This interprofessional team can include specialists, other clinicians (MDs, DOs, PAs, NPs), nursing staff, and pharmacists. In the emergency department, swift intake and triage by the nurse or medical technician to identify a patient with dangerously elevated blood pressure and quickly but effectively convey the critical information to a physician or provider are necessary. If hospital admission is warranted, communicating the crucial details of the patient's presentation, medical history, and the treatment and current medical workup that have been completed are important, so time and resources are not wasted on repeating tests and exams. Utilizing an interprofessional team methodology that employs open communication between all team members and coordinated activity will improve patient outcomes and fewer adverse effects, particularly in hypertensive emergencies. [Level 5]
What is intravenous labetalol used for?
Intravenous labetalol in the treatment of severe hypertension and hypertensive emergencies.
What is the best antihypertensive for pregnancy?
Labetalol is one of the most commonly used anti-hypertensives medications used for the treatment of hypertension during pregnancy. Hypertension during pregnancy is an increasingly common and a leading cause of maternal mortality and morbidity worldwide. Severe hypertension requires prompt treatment with rapid-acting antihypertensive agents such as labetalol to avoid stroke and placental abruption. Previously, intravenous hydralazine was utilized as a first-line drug for this purpose, although there is a growing experience with other agents, including intravenous labetalol and oral nifedipine. There appears to be a growing concern about the neonatal effects of hydralazine. Treatment aims to lower blood pressure during pregnancy into the mild range (less than 160/100 mm Hg), reduce the risk of stroke and other maternal cardiovascular complications. [3][4]
How long does it take for a lbetalol to work?
Labetalol is metabolized by the liver resulting in an inactive glucuronide conjugate. It has an onset of action within 2 to 5 minutes, reaches its peak effects at 5 to 15 minutes, has an elimination half-life of 5.5 hours, and a duration of action up to four hours.
Is labetalol safe for hypotension?
Overall, labetalol is usually well tolerated. Most adverse effects are typically mild and transient. As previously described above, symptomatic postural hypotension is a potential occurrence if patients are tilted or allowed to change positions from the supine or seated position to standing too quickly. This is especially important in the post-operative period (PACU or the ward) when managing a hypertensive patient with labetalol who can otherwise ambulate to the bathroom. Increased sweating, as well as flushing, have been reported with the use of labetalol. It seems the incidence of adverse reactions after administering labetalol seems to be dose-dependent. [6]
What is the best treatment for a beta blocker overdose?
Supportive care and close monitoring are the staples of treatment for an overdose of beta-blockers with the addition of glucagon for severe refractory hypotension and bradycardia.
Is labetalol FDA approved?
The FDA-approved indication for labetalol is the treatment of arterial hypertension, which ranges from acute hypertensive crises (urgent/emergency) to stable chronic hypertension. Labetalol in clinical practice has several common off-label uses that include acute hypertension in pregnancy and hypertension associated with acute ischemic stroke, and intracranial hemorrhage, including subarachnoid hemorrhage. Today, labetalol is usually reserved for the acute management of hypertensive crises.
Does labetalol cause hypotension?
Neonatal side effects of maternal labetalol treatment in severe preeclampsia. Hypotension is more common after maternal labetalol exposure, regardless of the dosage and route of administration. The need for intubation and the presence of a PDA also play a role.
Is hypoglycemia related to prematurity?
Hypoglycemia is a very common finding in this population and is merely related to prematurity and independent of lab …. Hypotension is more common after maternal labetalol exposure, regardless of the dosage and route of administration. The need for intubation and the presence of a PDA also play a role. Hypoglycemia is a very common finding in this ...
What is the injectable form of labetalol used for?
The injectable form of labetalol is only used to treat severe hypertension.
How long does it take to stop labetalol?
If you need to discontinue labetalol, your doctor will advise how to do this slowly over one to two weeks. If you have diabetes, labetalol may mask some of the symptoms of low blood sugar, such as a fast heartbeat. Tell all health professionals that you take labetalol as it may interfere with some procedures. 6.
How long does it take for labetalol to work?
Peak concentrations of labetalol tablets are reached after one to two hours of oral administration. Labetalol tablets need to be given twice a day. Peak concentrations are reached within 5 minutes of labetalol injection. Blood pressure-lowering effects increase with higher dosages.
What medications can interact with labetalol?
Common medications that may interact with labetalol include: antidepressants, such as fluoxetine, paroxetine, St John’s Wort, and monoamine oxidase inhibitors. Tricyclic antidepressants (such as amitriptyline, imipramine, and nortriptyline) may increase the risk of tremor . antifungals, such as terbinafine.
What class of drug is lbetalol?
Labetalol belongs to the class of drugs known as beta-blockers. It has selective alpha-1 adrenergic receptor blocking activity and nonselective beta-blocking activity.
Can labetalol cause heart attacks?
Sudden discontinuation of labetalol has been associated with an exacerbation of angina, and occasionally heart attacks and arrhythmias. The dosage needs to be tapered off slowly.
Can you take a Labetalol with a diuretic?
Use at recommended dosages does not appear to have a detrimental effect on kidney function in people with normal kidney function. Labetalol may be used alone or in addition to other antihypertensives (such as diuretics). Available in an injectable form and as a tablet. Brand names include Normodyne and Trandate.
METHODS
Exclusion criteria: Active labor |Received other antihypertensive medication within 2 hours of initial cerebral perfusion pressure measurement
CONCLUSION
Cerebral perfusion pressure was significantly decreased following a single dose of oral nifedipine vs IV labetalol in patients with severe hypertension in the setting of preeclampsia
How long after maternal labetalol is it detectable?
In a 6-day-old breastfed infant whose mother was taking labetalol 600 mg daily, labetalol in plasma was 18 and 21 mcg/L at 4 and 8 hours after the maternal dose; labetalol was undetectable in a 7-day-old infant whose mother was taking the same dosage.[4]
What is the name of the National Library of Medicine?
Bethesda (MD): National Library of Medicine (US); 2006-.
Does labetalol cause accumulation in breast milk?
With 50% protein binding, 5% renal excretion and a moderate half-life, labetalol presents moderat ely low risk for accumulation in infants.
Does labetalol increase prolactin?
Intravenous labetalol can increase serum prolactin in men and non-nursing women, although the increase is greater in women. Oral labetalol does not increase serum prolactin.[8,9] The maternal prolactin level in a mother with established lactation may not affect her ability to breastfeed.