How does mannitol reduce intracranial pressure?
Mannitol lowers intracranial pressure by osmotically drawing free water out of the brain and into circulation where it can be eliminated. If given as a continuous prolonged infusion, mannitol will eventually cross the blood-brain barrier and have no effect on intracranial pressure.
Does mannitol increase intracranial pressure?
Mannitol is currently used to reduce intracranial pressure (ICP), but the evidence supporting its usefulness has been questioned. We aim to meta-analyze the effectiveness of mannitol in reducing ICP in adult patients with cerebral injuries and its dependency on baseline ICP values, comparing findings from individual patient data (IPD) and aggregated data (AD) meta-analysis performed on the ...
How does mannitol cause transient volume expansion?
Mannitol being an osmotically active agent draws fluid from the extravascular compartment into the vascular compartment. This causes transient volume expansion and may cause pulmonary edema if the cardiac or renal status is compromised. But if the renal status is good, this extra fluid is soon excreted as mannitol is an osmotic diuretic as well.
Is mannitol bad for your teeth?
This includes diet soda, sugar free candy, and more. But few people realize that there is a relationship between sugar substitutes and dental health. Most current sugar-free products contain one or more of these three substitutes: Sorbitol, Mannitol, Saccharine . These sugar substitutes can turn into teeth-attacking acids in the mouth.

How does mannitol cause rebound ICP?
Aim: Widespread use of mannitol to reduce brain edema and lower elevated ICP in brain tumor patients continues to be afflicted by the so-called rebound phenomenon. Leakage of mannitol into the brain parenchyma through an altered BBB and secondary reversal of osmotic gradient is considered the major cause of rebound .
Does mannitol increase CPP?
Mannitol consistently reduced ICP and increased CPP and CBF by 10 to 20 minutes after infusion. The lowest flows (31.8 ml/100 gm/min) were recorded from the most damaged hemispheres of patients with focal injuries and elevated ICP.
Why is mannitol contraindicated in intracranial hemorrhage?
Therefore, the overall conclusion is that although mannitol decreases edema in ICH at first,[16,17] according to the three following mechanisms, it finally widens ICH, thus, its use is not recommended.
What fluids increase ICP?
Mannitol, a hypertonic crystalloid solution, is commonly used to decrease brain water content and reduce intracranial pressure (ICP). Hypertonic saline solutions also decrease brain water and ICP while temporarily increasing systolic blood pressure and cardiac output.
Does mannitol decrease ICP?
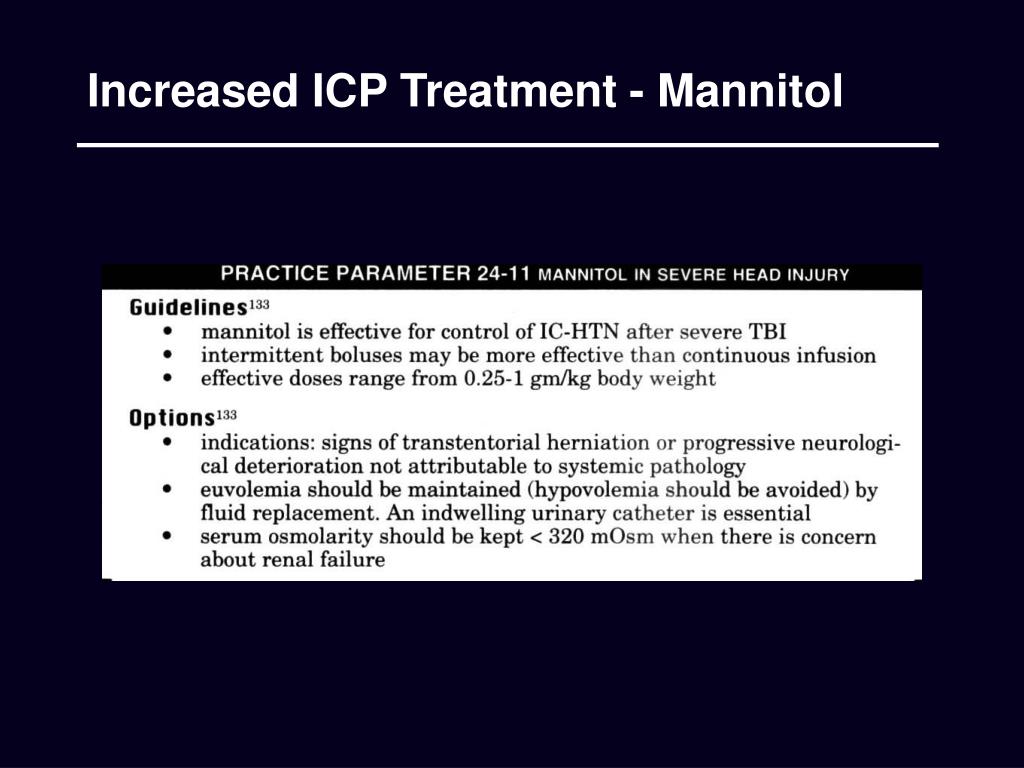
Mannitol has been used to reduce elevated ICP for decades. Current evidence suggests that mannitol is more effective in reducing ICP in patients with TBI compared with barbiturates and is recommended by guidelines.
When is mannitol contraindicated?
There are multiple contraindications to giving mannitol, including: Established anuria due to renal disease. Pulmonary edema or severe pulmonary congestion. Active intracranial bleeding except for during a current craniotomy.
What medication reduces ICP?
Medication Summary Carbonic anhydrase inhibitors (eg, acetazolamide) and loop diuretics (eg, furosemide) are thought to exert their effect on ICP by reducing cerebrospinal fluid (CSF) production at the choroid plexus. Cardiac glycosides have a similar effect.
Do you give mannitol for hemorrhagic stroke?
Mannitol infusion in patients with acute intracerebral hemorrhage can improve cerebral blood flow in bilateral hemispheres and decrease intracranial pressure in the hemorrhagic hemisphere (250ml) and in the nonhemorrhagic hemisphere (125ml and 250ml).
What drugs decrease intracranial pressure?
Mannitol is the most commonly used hyperosmolar agent for the treatment of intracranial hypertension.
Do IV fluids increase ICP?
Large amounts of hypo-osmolar or hypotonic fluids reduce plasma osmolality, drive water across the blood brain barrier (BBB), and increase cerebral water content and ICP.
Why mannitol is given in head injury?
Mannitol is a sugar alcohol solution which is sometimes effective in reducing brain swelling after head injury.
Is mannitol contraindicated in head injury?
However, its effectiveness in the ongoing treatment of severe head injury remains unclear. There is evidence that excessive administration of mannitol may be harmful, by mannitol passing from the bloodstream into the brain, where it increases pressure within the skull and worsens brain swelling.
How does mannitol increased osmolality?
Mannitol also acts as an osmotic diuretic, leading to free water clearance and an increase in serum osmolality. As a result, water moves from the intracellular to the extracellular space, inducing a prolonged dehydrating effect.
What are the side effects of mannitol?
Common side effects may include:increased urination;nausea, vomiting;fever, chills, headache, runny nose;chest pain;rash; or.dizziness, blurred vision.
How does mannitol cause plasma expansion?
At large doses mannitol increases excretion of sodium and potassium. Initially, mannitol acutely raises plasma and extracellular osmolality, which leads to an increase in circulating blood volume. This leads to increase in stroke volume, cardiac output, and blood pressure.
What is the mechanism of action of mannitol?
Mannitol elevates blood plasma osmolality, resulting in enhanced flow of water from tissues, including the brain and cerebrospinal fluid, into interstitial fluid and plasma. As a result, cerebral edema, elevated intracranial pressure, and cerebrospinal fluid volume and pressure may be reduced.
How does mannitol help with intraocular pressure?
Mannitol may be used to reduce intraocular pressure when given intravenously. The mannitol is a new solute in the intravascular space, which increases the tonicity of the blood plasma. The increased tonicity of the blood plasma draws water out of the vitreous humor of the eye and into the intravascular space. Once in the intravascular space, the mannitol and associate water are excreted by the kidney. The decreased water of the vitreous humor lowers the intraocular pressure.
Why is mannitol given?
Much like mannitol given for oliguria of acute renal failure, mannitol can be given to increase the excretion of toxic materials, substances, and drugs. The kidneys excrete mannitol. The mannitol is poorly reabsorbed once excreted and thus draws extra water with it into the renal collecting ducts. The extra water in the renal collecting ducts can help increase the excretion of water-soluble toxic materials, substances, and drugs.
How does mannitol affect the brain?
The mannitol causes the cells in the brain to dehydrate mildly. The water inside the brain cells (intracellular water) leaves the cells and enters the bloodstream as the mannitol draws it out of the cells and into the bloodstream. Once in the bloodstream, the extra water is whisked out of the skull. When the mannitol gets to the kidneys, the kidneys filter the mannitol into the urine. The mannitol again draws the water with it, and diuresis (increased urination) ensues.
What is mannitol used for?
Mannitol can be used for the reduction of intracranial pressure and brain mass, to reduce intraocular pressure if this is not achievable by other means, to promote diuresis for acute renal failure to prevent or treat the oliguric phase before irreversible damage, and to promote diuresis to promote excretion of toxic substances, materials, and metabolites. There are also multiple uses of mannitol that are not FDA-approved. This activity will highlight the mechanism of action, adverse event profile, pharmacology, monitoring, and relevant interactions of mannitol, pertinent for members of the interprofessional team in treating patients with conditions where it is of clinical value.
How much mannitol is in 100 ml of fluid?
Mannitol can be found in varying concentrations from 5% mannitol (5 gm mannitol dissolved in 100 mL of fluid) up to 25% mannitol (25 gm of mannitol dissolved in 100 mL of fluid). A commonly encountered solution is 20% mannitol (20 grams of mannitol dissolved in 100 mL of fluid). [2]
How does mannitol work?
Mannitol works to protect sharp objects as they get introduced into a vascular space. A mannitol cap on a pacemaker wire will protect the tip from becoming dulled while a clinician introduces it into the vascular system then the mannitol will readily dissolve away with minimal effect.
How many carbons are in mannitol?
Mannitol is a six-carbon, linear, simple sugar which is only mildly metabolized by the body and primarily excreted rapidly by the kidneys when given intravenously and poorly absorbed when taken orally.
How does mannitol work?
Mannitol works by both improved osmotic gradient and rheology – studies have shown that mannitol increases CBF by as much as 20% and decreases CBF after brain injury, although it was recently shown not to affect brain tissue oxygenation. Note that there is some evidence that Osm > 320 will impair renal function, and most people will hold mannitol of [Na+] > 155-160, however the data supporting either of these is not strong.
What is the most powerful predictor of neurological worsening?
A retrospective look at 427 in the NMDA antagonist Selfotel trial found that the most powerful predictor of neurological worsening was ICP 20 mm Hg either initially or during neurological deterioration. There was no correlation with the CPP as long as the CPP was > 60 mm Hg.
Is cerebral perfusion pressure dependent on ICP?
The recognition of this led to the concept of Cerebral Perfusion Pressure, defined as MAP – ICP (or CVP if it is higher than ICP). Management of patients with head injuries focuses on optimizing perfusion, ie miminimizing ICP and maximizing CPP. Complicating this is the fact that excessive cerebral edema can cause herniation, which is fatal independent of the effects of CPP. There is thus considerable debate as to whether ICP or CPP is a more important target (see #ICP vs. CPP for more).
Do barbiturates lower ICP?
Barbiturates have been studied by in several prospective, randomized clinical trials with none of them showing a clear benefit, however one suggested a benefit in patients in whom barbiturates lowered ICP – a 2000 Cochrane Database Review, however, concluded that “there is no evidence that barbiturate therapy in patients with acute severe head injury improves outcome. Barbiturate therapy results in a fall in blood pressure in 1 in 4 treated patients. The hypotensive effect of barbiturate therapy will offset any ICP lowering effect on cerebral perfusion pressure.” If patients are tried on barbiturates, wean them as soon as possible to avoid myocardial complications as well as pneumonia, for which these patients are at a high risk
Does sedation increase ICP?
Sedation decreases anxiety, fear, and response to pain, all of which increase ICP. Steroids can reduce edema, especially in traumatic brain injury – steroids are harmful in the setting of TBI but may be exceedingly helpful in patients with intracranial tumors.
Does mannitol cause renal failure?
Much of this is refuted by a recent retrospective study of 98 patients on mannitol at WUSTL, the multivariate analysis of which showed that APACHE II and history of CHF were the only predictive factors leading to mannitol-induced renal failure. Osmolality gap and mannitol dose had no correlation. Furthermore, all cases of MI-RF reversed. Loop diuretics are helpful as well but are also recommended only when Osm < 320 and [Na+] < 155.
How to measure ICP?
The use of ultrasound to measure the diameter of the optic nerve sheath has been recently identified as a method to indicate raised ICP. This is usually measured 3 mm behind the globe with 2–3 measurements taken in each eye. The threshold for denoting elevated ICP usually ranges from 0.48 cm to 0.63 cm.
What should be included in an ICP evaluation?
The evaluation of increased ICP should include detailed history taking, physical examination, and ancillary studies.
What is intracranial hypertension?
Intracranial hypertension (IH) is a clinical condition that is associated with an elevation of the pressures within the cranium. The pressure in the cranial vault is measured in millimeters of mercury (mm Hg) and is normally less than 20 mm Hg.
What causes increased intracranial pressure?
The causes of increased intracranial pressure (ICP) can be divided based on the intracerebral components causing elevated pressures: Increase in brain volume. Generalized swelling of the brain or cerebral edema from a variety of causes such as trauma, ischemia, hyperam monemia, uremic encephalopathy, and hyponatremia.
What is the pressure in the cranial vault?
The pressure in the cranial vault is measured in millimeters of mercury (mm Hg) and is normally less than 20 mm Hg. The cranium is a rigid structure that contains three main components: brain, cerebrospinal fluid, and blood. Any increase in the volume of its contents will increase the pressure within the cranial vault.
Is hypertonic saline safe?
Three percent hypertonic saline is also commonly used to decrease cerebral edema and can be administered as a 5 ml/kg bolus or a continuous infusion, monitoring serum sodium levels closely. It is considered relatively safe while serum sodium is < than 160mEq/dl or serum osmolality is less than 340 mOsm. [12]
Does intracranial hypertension increase the risk of death?
Prognosis depends on the underlying etiology and severity of the presentation. Benign intracranial hypertension does not increase the risk of death rate by itself; rather, the death rate is increased by morbid obesity which is a common association with benign intracranial hypertension.
Is mannitol good for traumatic brain injury?
Mannitol for acute traumatic brain injury. High-dose mannitol may be preferable to conventional-dose mannitol in the acute management of comatose patients with severe head injury. Mannitol therapy for raised ICP may have a beneficial effect on mortality when compared to pentobarbital treatment, but may have a detrimental effect on mortality …. ...
Is mannitol good for comatose patients?
High-dose mannitol may be preferable to conventional-dose mannitol in the acute management of comatose patients with severe head injury. Mannitol therapy for raised ICP may have a beneficial effect on mortality when compared to pentobarbital treatment, but may have a detrimental effect on mortality …. Mannitol for acute traumatic brain injury ...
Does mannitol help with ICP?
Mannitol therapy for raised ICP may have a beneficial effect on mortality when compared to pentobarbital treatment, but may have a detrimental effect on mortality when compared to hypertonic saline.
How many tiers of ICP elevation?
Treatment for ICP elevation can be loosely divided into three rough tiers, depending on how aggressive the treatments are (table below). Please note, however, that this is intended only as a rough cognitive rubric. It will often be appropriate to mix treatments from different tiers.
How does fever affect ICP?
A fever increases ICP by increasing the brain’s metabolic demands and need for arterial blood supply.
Why is noncommunicating hydrocephalus easier to diagnose?
Noncommunicating hydrocephalus is therefore easier to diagnose based on CT scans, because pressure differentials will cause shifts in brain tissue visible on CT.
What causes cytotoxic edema in MRI?
MRI features: cytotoxic edema causes diffusion restriction, which leads to hyperintensity on DWI sequences and hypointensity on ADC sequences. Causes: Cytotoxic edema is caused most notably by ischemic stroke.
Is papilledema accurate for ICP elevation?
Papilledema may be less accurate for immediate-onset intracranial hypertension, because it takes some time to develop. Papilledema may be useful for identifying ICP elevation in cases where the nerve sheath is borderline (e.g., between 5-6 mm wide). More on this here.
What concentration of hypertonic saline should be infused through a central line?
Hypertonic saline greater than 3% concentration should be infused through a central line.
What causes intracranial pressure to increase?
Acute brain injuries of all sorts increase the pressure inside the skull (intracranial pressure). Traumatic brain injury, bleeding in or around the brain, severe ischemic stroke, and acute hepatic failure all raise intracranial pressure, and increased intracranial pressure often becomes the most severe and immediate threat to life ...
How does intracranial pressure affect the brain?
As volume increases inside the skull, intracranial pressure exponentially rises after it passes an inflection point of ~20-25 mm Hg. As ICP passes 50-60 mm Hg and approaches arterial pressure, global brain ischemia and eventual brain death result. The brain is 80% water, so using hyperosmolar agents to create an osmolar gradient between the inside of the brain and the systemic circulation has strong theoretical appeal. Hypertonic saline and mannitol are effective because they do not cross the blood-brain barrier (much), and thereby draw cerebrospinal fluid out of the cranium and fluid out of the injured brain, reducing pressure and further injury.
What is the safest osmolarity?
Serum osmolarity of 320 mOsm/L has been traditionally considered the upper limit for safety, but some expert clinicians exceed this in practice and have not reported any safety problems, according to the author.
How to calculate sodium needed in mmol?
sodium needed in mmol = (lean body weight in kg × 0.5 for a woman or 0.6 for a man) × (target sodium − current sodium in mmol/L).
Is mannitol effective for brain injury?
Hypertonic saline and mannitol are effective because they do not cross the blood-brain barrier (much), and thereby draw cerebrospinal fluid out of the cranium and fluid out of the injured brain, reducing pressure and further injury. In brain injuries that include disruption of the blood-brain barrier, hyperosmolar therapy may be less effective.
Can an intensivist treat intracranial pressure?
In ideal circumstances, every patient with raised intracranial pressure would be treated at a center providing advanced neurologic critical care; however, this is not the case in most of the world. Therefore, every intensivist should be at least familiar with the principles of hypertonic / hyperosmolar therapy for the treatment ...
Does mannitol increase blood pressure?
At large doses mannitol increases excretion of sodium and potassium. Initially, mannitol acutely raises plasma and extracellular osmolality, which leads to an increase in circulating blood volume. This leads to increase in stroke volume, cardiac output, and blood pressure.
Is mannitol an osmotic diuretic?
Definition. Mannitol is an osmotic diuretic that is a six-carbon carbohydrate that undergoes filtration at the glomerulus with limited or no reabsorption in the proximal tubules. It works as osmotic diuretic and is often used to reduce intracranial pressure and treat oliguric renal failure. At large doses mannitol increases excretion ...