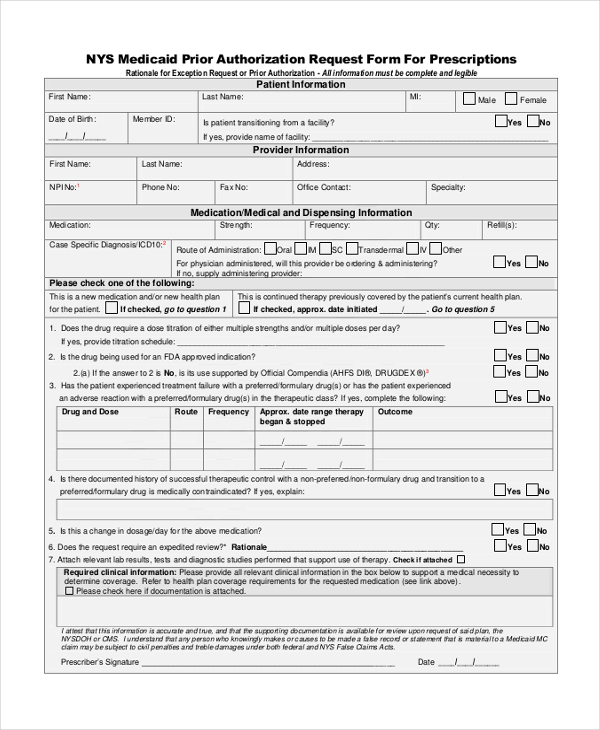
In some referral cases, you may first be required to obtain prior authorization from your Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
What medications need prior authorization?
What types of medical treatments and medications may need prior authorization?
- Medications that may be unsafe when combined with other medications
- Medical treatments that have lower-cost, but equally effective, alternatives available
- Medical treatments and medications that should only be used for certain health conditions
- Medical treatments and medications that are often misused or abused
- Drugs often used for cosmetic purposes
Does Medicare require pre approval?
Traditionally, both parts of Original Medicare (Medicare Parts A and B) rarely require pre-approval. Originally, Medicare Part A required no prior authorization whatsoever. Now however, the law has been changed to allow this process for certain limited Durable Medical Equipment items on very rare occasions.
Does your insurance plan require an authorization?
What you need to know... Some insurance plans require our office (the PP) to seek authorization for your visit with a specialist or imaging facility before they will treat you. This process is known as an Authorization. In order to complete an authorization we must submit information to your insurance carrier for approval.
Does Medicare TRICARE beneficiary require authorization?
Preauthorization review is only required for TRICARE For Life (TFL) beneficiaries when TFL is the primary payer for the specific services listed below. If Medicare or another primary insurance covers the care, then no authorization review is necessary.
What happens if you don't get prior authorization?
If you're facing a prior-authorization requirement, also known as a pre-authorization requirement, you must get your health plan's permission before you receive the healthcare service or drug that requires it. If you don't get permission from your health plan, your health insurance won't pay for the service.
What services typically require prior authorizations?
The other services that typically require pre-authorization are as follows:MRI/MRAs.CT/CTA scans.PET scans.Durable Medical Equipment (DME)Medications and so on.
Does Medicare ever require prior authorization?
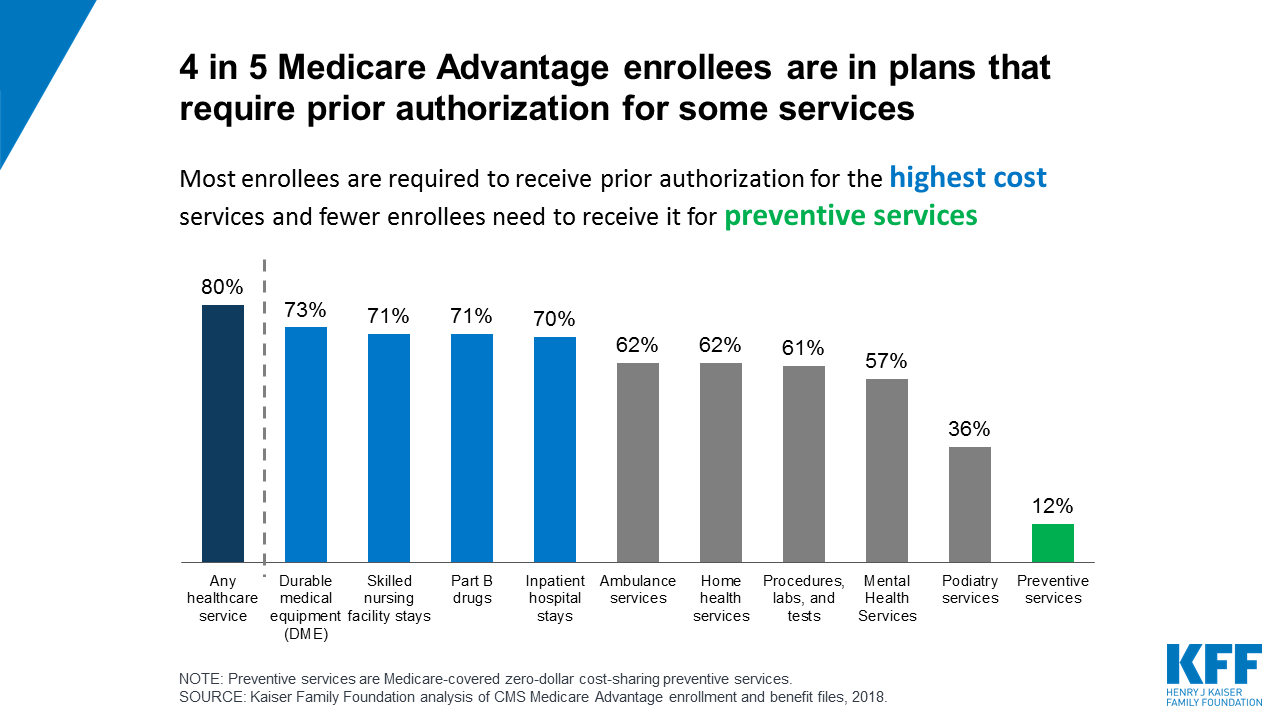
Traditional Medicare, in contrast, does not require prior authorization for the vast majority of services, except under limited circumstances, although some think expanding use of prior authorization could help traditional Medicare reduce inappropriate service use and related costs.
What triggers a prior authorization?
When it comes to a medication prior authorization, the process typically starts with a prescriber ordering a medication for a patient. When this is received by a pharmacy, the pharmacist will be made aware of the prior authorization status of the medication. At this point, they will alert the prescriber or physician.
Why does my prescription need prior authorization?
Your insurance company may require prior authorization before covering certain prescriptions. This is to ensure that the medication is appropriate for your treatment. It also helps to make sure it's the most cost-effective option. When prior authorization is granted, it is typically for a specific length of time.
Does Medicare require a prior authorization for MRI?
Medicare replacement plans require a prior authorization for CTs, MRIs and Pet scans.
What does prior authorization required mean?
What is a Prior Authorization? A prior authorization (PA), sometimes referred to as a “pre-authorization,” is a requirement from your health insurance company that your doctor obtain approval from your plan before it will cover the costs of a specific medicine, medical device or procedure.
What is the procedure to obtain pre authorization from Medicare?
Prior authorization works by having your health care provider or supplier submit a prior authorization form to their Medicare Administrator Contractor (MAC). They must then wait to receive a decision before they can perform the Medicare services in question or prescribe the prescription drug being considered.
What is Medicare prior authorization form?
A Medicare prior authorization form, or drug determination request form, is used in situations where a patient's prescription is denied at the pharmacy. Medicare members who have prescription drug coverage (Part D) will be covered for almost all their medication costs.
How long is a prior authorization good for?
A PA for a health care service shall be valid for a period of time that is reasonable and customary for the specific service, but no less than 60 days from the date the health care provider receives the PA, subject to confirmation of continued coverage and eligibility and to policy changes validly delivered.
What's the difference between precertification and prior authorization?
Pre-authorization is step two for non-urgent or elective services. Unlike pre-certification, pre-authorization requires medical records and physician documentation to prove why a particular procedure was chosen, to determine if it is medically necessary and whether the procedure is covered.
When did prior authorizations start?
Prior authorizations actually originated from the use of utilization reviews in the 1960s. Utilization reviews started at the beginning of Medicare and Medicaid legislation. Their primary use was to verify an admission in the hospital, which verified the need for treatment based on a confirmed diagnosis by two doctors.
What are the types of authorization in medical billing?
The amount of information about a project that's displayed to a specific user is defined by one of three authorization levels: full, restricted, or hidden.
For which POS prior authorization is an exception?
Exceptions: Emergency, Radiology, Anesthesiology, and Pathology (ERAP) specialties do not require authorization when billed with POS 21, POS 22, POS 23, or revenue code 0450 for all providers.
What is prior authorization in health care?
Prior authorization (also called “preauthorization” and “precertification”) refers to a requirement by health plans for patients to obtain approval of a health care service or medication before the care is provided. This allows the plan to evaluate whether care is medically necessary and otherwise covered.
What's the difference between precertification and prior authorization?
Pre-authorization is step two for non-urgent or elective services. Unlike pre-certification, pre-authorization requires medical records and physician documentation to prove why a particular procedure was chosen, to determine if it is medically necessary and whether the procedure is covered.
When is prior approval required for Medicaid?
Prior approval is required for Medicaid for Pregnant Women beneficiaries when the physician determines that services are needed for the treatment of a medical illness, injury or trauma that may complicate the pregnancy.
How long does a provider have to request a continuing care authorization?
Providers must request authorization of a continuing services 10 calendar days before the end of the current authorization period for authorization to continue without interruption for 10 calendar days after the date an adverse decision notice (change notice) is mailed to the Medicaid beneficiary or to the beneficiary's legal guardian and copied to the provider.
What is retroactive prior approval?
Retroactive prior approval is considered when a beneficiary, who does not have Medicaid coverage at the time of the procedure, is later approved for Medicaid with a retroactive eligibility date. Exceptions may apply.
What is Medicaid research?
Medicaid researches requests to determine the effectiveness of the requested service, procedure or product to determine if the requested service is safe, generally recognized as an accepted method of medical practice or treatment, or experimental/investigational.
What does Medicaid notify?
Medicaid notifies the provider following established procedures of approvals, including service , number of visits, units, hours or frequency.
When is a beneficiary eligible for medicaid?
A beneficiary must be eligible for Medicaid coverage on the date the service or procedure is rendered. It is the responsibility of the provider to clearly document that the beneficiary has met the clinical coverage criteria for the service, product or procedure. Services must be performed and billed by the rendering provider.
When do you have to request reauthorization of a service?
Providers must request reauthorization of a service before the end of the current authorization period for services to continue. The date that the request is submitted affects payment authorization for services that are denied, reduced or terminated.
What is CMS in Medicare?
The Centers for Medicare & Medicaid Services (CMS) runs a variety of programs that support efforts to safeguard beneficiaries’ access to medically necessary items and services while reducing improper Medicare billing and payments. Through prior authorization and pre-claim review initiatives, CMS helps ensure compliance with Medicare rules.
What is pre claim review?
Under pre-claim review, the provider or supplier submits the pre-claim review request and receives the decision prior to claim submission; however, the provider or supplier can render services before submitting the request. A provider or supplier submits either the prior authorization request or pre-claim review request with all supporting medical ...
How does a preclaim review work?
Under pre-claim review, the provider or supplier submits the pre-claim review request and receives the decision prior to claim submission; however, the provider or supplier can render services before submit ting the request. A provider or supplier submits either the prior authorization request or pre-claim review request with all supporting medical documentation for provisional affirmation of coverage for the item or service to their Medicare Administrator Contractor (MAC). The MAC reviews the request and sends the provider or supplier an affirmed or non-affirmed decision.
Managed Care Prior Authorization
The MCEs are responsible for processing medical and pharmacy PA requests for managed care members enrolled in Healthy Indiana Plan (HIP), Hoosier Care Connect, and Hoosier Healthwise and for notifying members about PA decisions. For information about PA criteria, processes, and procedures, contact the MCE with which the member is enrolled.
Prior Authorization Status Information
Learn how the high-level PA status codes displayed on the IHCP Provider Healthcare Portal (Portal) and reported in 278 transactions and by the Interactive Voice Response (IVR) system translate to the working statuses associated with each standard response.
What is prior authorization?
Prior authorization refers to services that require Department authorization before they are performed. Prior authorization has specific requirements. Some services may require both Passport referral and prior authorization. If a service requires prior authorization, the requirement exists for all Medicaid members. Prior authorization is usually obtained through the Department or a prior authorization contractor.
How long before a procedure can you provide documentation?
Documentation should be provided at least two weeks prior to the procedure date.
What is MPQH documentation?
Documentation that supports medical necessity. This varies based on circumstances. MPQH will instruct providers on required documentation on a case-by-case basis.
Does Montana Medicaid reimburse for off label drugs?
Montana Medicaid does not reimburse for convenience, off label or experimental use of drugs, per Administrative Rules of Montana (ARM) 37.85.207.
Do you need a copy of a member's plan of care?
For members being treated by a licensed therapist, a copy of the member’s plan of care in relation to the item/service is required; video if possible.
Does Montana require prior authorization for pulmonary rehabilitation?
Montana Medicaid requires prior authorization for pulmonary and cardiac rehabilitation and for out-of-state inpatient rehabilitation.
What is prior authorization in Texas?
Prior authorization is a type of approval that is required for many services that providers render for Texas Medicaid. If a service requires prior authorization but the request for prior authorization is not submitted or is denied, the claim will not be paid.
Where to submit prior authorization PA?
You can submit prior authorizations through PA on the Portaland on paper.
When will OPDs receive notice of exemption?
Hospital OPD providers who met the affirmation rate threshold of 90% or greater will receive a written Notice of Exemption no later than March 1, 2021. Those hospital OPDs will be exempt from submitting prior authorization requests for dates of service beginning May 1, 2021.
Does prior authorization for OPD help Medicare?
CMS believes prior authorization for certain hospital OPD services will ensure that Medicare beneficiaries continue to receive medically necessary care – while protecting the Medicare Trust Fund from improper payments and, at the same time, keeping the medical necessity documentation requirements unchanged for providers.
What is CHNCT prior authorization?
Prior authorization refers to the Community Health Network of Connecticut, Inc. ® (CHNCT) process for approving covered services prior to the delivery of the service or initiation of the plan of care based on a determination by CHNCT as to whether the requested service is medically necessary.
How to view authorization units?
View your authorization units used by visiting the secure portal. Once you have logged in to the secure portal, click the "Authorizations"link to access this new feature. You will then be granted access via our Web Support Help Desk.
Do you need prior authorization for Medicare?
Prior authorization is NOT required for dual eligible members (Medicare/Medicaid coverage) unless the good or service is not covered by the member’s Medicare plan.
