Does polymyalgia rheumatica increase the risk of heart attack and stroke?
Polymyalgia rheumatica may raise the risk for heart attack and stroke in older adults. Polymyalgia rheumatica is an inflammatory muscle disorder that leads to pain and stiffness.
What is polymyalgia rheumatica?
Polymyalgia rheumatica is an inflammatory disorder that causes muscle pain and stiffness, especially in the shoulders. Signs and symptoms of polymyalgia rheumatica (pol-e-my-AL-juh rue-MAT-ih-kuh) usually begin quickly and are worse in the morning. Most people who develop polymyalgia rheumatica are older than 65. It rarely affects people under 50.
What is the long-term outlook for someone with polymyalgia rheumatica?
People with polymyalgia rheumatica are also more likely to develop peripheral artery disease. This condition impairs blood circulation and often causes leg pain and ulcers. What Is the Long-Term Outlook for Someone with Polymyalgia Rheumatica? There’s no cure for polymyalgia rheumatica.

Can PMR cause inflammation of the heart?
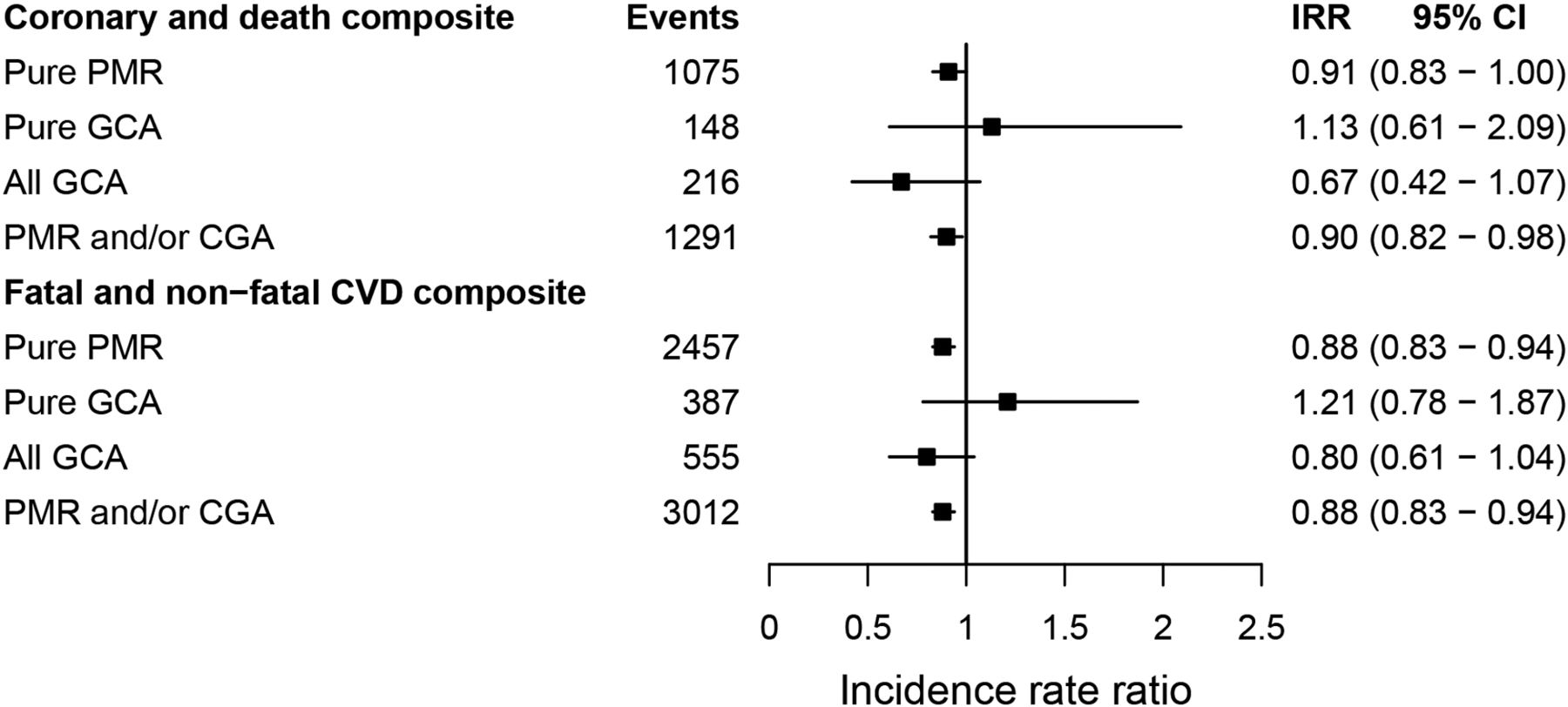
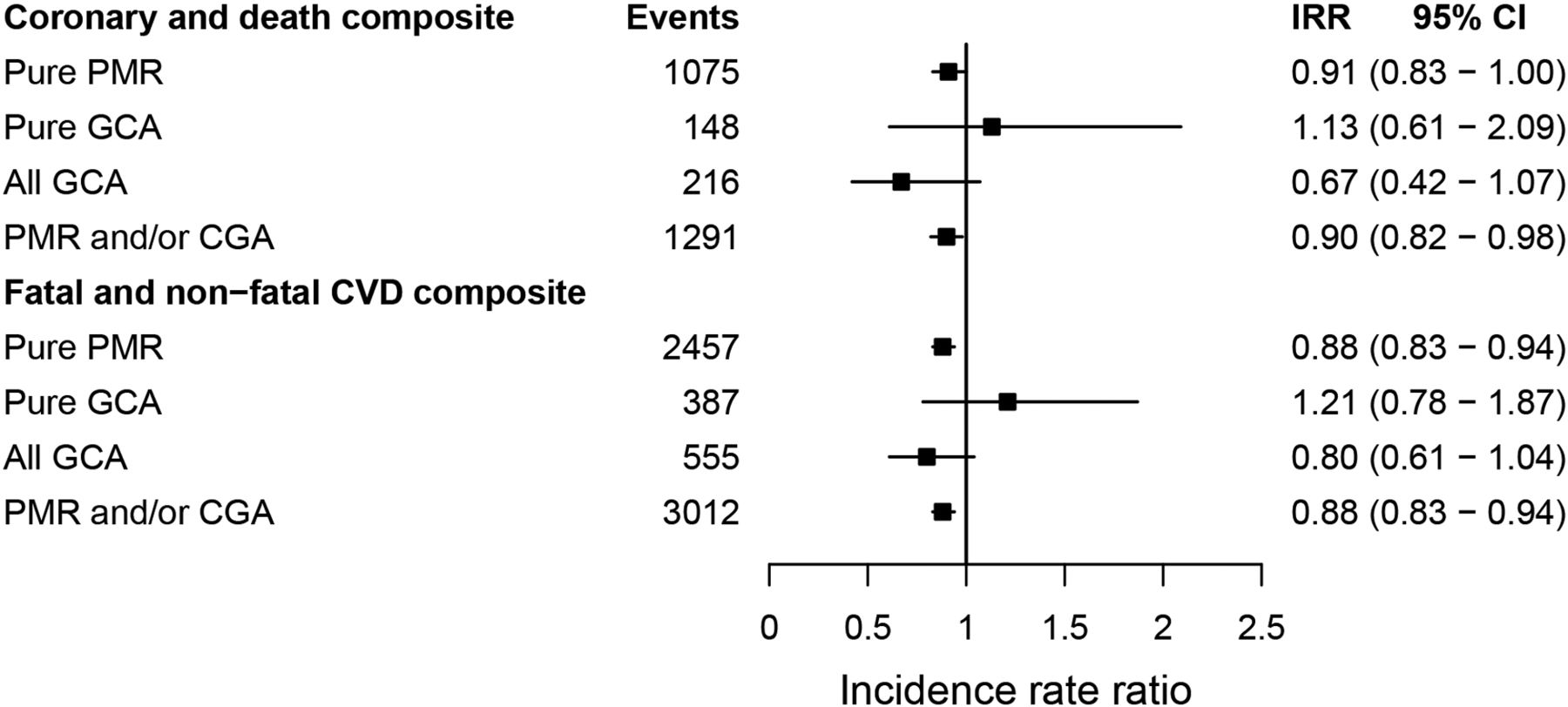
The study, published July 28 in the CMAJ, revealed the patients with polymyalgia rheumatica are at higher risk for all forms of vascular disease, including angina, heart attack, atherosclerosis and stroke. The risk for these conditions peaked six to 12 months after being diagnosed with the inflammatory muscle disorder.
What happens if polymyalgia rheumatica is not treated?
Signs and symptoms include headaches, jaw pain, vision problems and scalp tenderness. If left untreated, this condition can lead to stroke or blindness.
Does polymyalgia rheumatica affect blood pressure?
Alternatively, the excess risk in polymyalgia rheumatica may be mediated by corticosteroids, via adverse effects on blood pressure and lipids.
Can polymyalgia affect the chest?
Abstract. We report a patient with polymyalgia rheumatica (PMR) who initially presented with chest pain pleural and pericardial effusions. A history was then obtained of shoulder girdle aching and stiffness, suggestive of PMR, and laboratory investigations supported the diagnosis.
Does polymyalgia rheumatica ever go away?
Polymyalgia rheumatica often improves on its own after this time. However, there's a chance it will return after treatment stops. This is known as a relapse. Do not suddenly stop taking steroid medicine unless your doctor tells you it's safe to stop.
What foods make polymyalgia worse?
Polymyalgia rheumatica is an inflammatory condition that causes pain and stiffness around the joints....Foods to avoidrefined carbohydrates, such as white bread or white rice.fried foods, such as french fries.sugary drinks.processed meats, such as salami or hotdogs.red meat.margarine.foods with added sugar.alcohol.
Can polymyalgia cause a stroke?
Conclusions: PMR was associated with a significantly higher risk of stroke in the three-year follow-up period. Physicians should be aware of this potential association in clinical settings.
Can polymyalgia rheumatica cause atrial fibrillation?
A highest association of AF was found with gout followed by vasculitis, and polymyalgia rheumatica when compared to other RD.
Can polymyalgia affect your breathing?
If your chest muscles are affected by the disease, you may experience breathing problems, such as shortness of breath or, in severe cases, respiratory failure.
What is the long term prognosis for polymyalgia rheumatica?
With early diagnosis and correct therapy, patients have an excellent prognosis. The average length of disease is 3 years. However, exacerbations may occur if steroids are tapered too rapidly, and relapse is common, affecting up to 25% of all treated patients.
What is the difference between polymyalgia and polymyalgia rheumatica?
Polymyalgia, or polymyalgia rheumatica, is an inflammatory disease of muscle. The cause is uncertain but it is believed to be an autoimmune disease in which the body's own immune system attacks the connective tissues.
Can a blood test detect polymyalgia rheumatica?
Tests. There's no specific test for polymyalgia rheumatica, but it's likely that a series of blood tests will be done. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are blood tests that can be used to check the levels of inflammation in your body.
Is polymyalgia rheumatica a serious condition?
PMR is usually a self-limiting disease. If untreated, patients will have an impaired quality of life. With early diagnosis and correct therapy, patients have an excellent prognosis. The average length of disease is 3 years.
How long can you take steroids for polymyalgia?
Most people with polymyalgia rheumatica will need a course of corticosteroid treatment that lasts for 18 months to 2 years to prevent their symptoms returning.
How long does a flare up of polymyalgia last?
The pain and stiffness is worse in the morning, usually lasts for one hour or more and may be accompanied by systemic features, such as fever, fatigue and anorexia. The onset of symptoms is typically between two weeks and two months.
Can polymyalgia cause bowel problems?
Conclusions. Patients with polymyalgia may have perforated colonic diverticular disease which mimics their rheumatic pathology. In such cases steroid therapy, which is the mainstay of polymyalgia therapy, can be detrimental.
How does polymyalgia rheumatica affect patients?
Complications of polymyalgia rheumatica affect patients’ daily life, making it difficult for them to move and perform tasks on their own due to stiffness and pain. It may become difficult to get in and out of bed, bathe oneself, or even comb their hair and get dressed.
What are the risk factors for polymyalgia rheumatica?
Risk factors for polymyalgia rheumatica include gender – women are twice as likely as men to develop it, – age, race, and geographic location. White Northern European populations are at a higher risk of developing polymyalgia rheumatica.
What is the most common inflammatory rheumatologic condition in older adults?
Author Dr. Christian Mallen wrote, “Polymyalgia rheumatica is one of the most common inflammatory rheumatologic conditions in older adults, with a lifetime risk of 2.4% for women and 1.7% for men.”
Which inflammatory disease increases the risk of vascular disease?
Other inflammatory diseases, such as rheumatoid arthritis, have also been shown to increase the risk of vascular diseases.
Is giant cell arteritis the same as polymyalgia?
Giant cell arteritis has also been found to contribute to the onset of polymyalgia rheumatica. In fact, some suggest the two diseases may actually be the same condition with different manifestations. Signs and symptoms of giant cell arteritis are common in polymyalgia patients, and vice versa.
Does polymyalgia rheumatica increase risk?
The authors wrote, “Our results showed that patients with polymyalgia rheumatica had an increased risk of all types of vascular events, even after traditional risk factors for vascular disease were controlled for. This excess risk was present soon after diagnosis, was present in both men and women.”
What are the risk factors for polymyalgia rheumatica?
Risk factors. Risk factors for polymyalgia rheumatica include: Age. Polymyalgia rheumatica affects older adults almost exclusively. It most often occurs between ages 70 and 80. Sex. Women are about two to three times more likely to develop the disorder. Race.
How do you know if you have polymyalgia rheumatica?
Symptoms. The signs and symptoms of polymyalgia rheumatica usually occur on both sides of the body and might include: Aches or pain in your shoulders. Aches or pain in your neck, upper arms, buttocks, hips or thighs. Stiffness in affected areas, particularly in the morning or after being inactive for a time. Limited range of motion in affected ...
What is the condition that causes muscle pain and stiffness in the shoulders and hips?
Polymyalgia rheumatica is an inflammatory disorder that causes muscle pain and stiffness, especially in the shoulders and hips. Signs and symptoms of polymyalgia rheumatica (pol-e-my-AL-juh rue-MAT-ih-kuh) usually begin quickly and are worse in the morning.
What is Polymyalgia rheumatica?
Polymyalgia rheumatica (pain in many muscles) is found to be associated with 733 drugs and 398 conditions by eHealthMe.
What is Heart rate increased?
Heart rate increased is found to be associated with 3,272 drugs and 2,776 conditions by eHealthMe.
How to use the study?
You can discuss the study with your doctor, to ensure that all drug risks and benefits are fully discussed and understood.
How the study uses the data?
The study is based on Heart rate increased and Polymyalgia rheumatica, and their synonyms.
Who is eHealthMe?
With medical big data and proven AI algorithms, eHealthMe provides a platform for everyone to run phase IV clinical trials. We study millions of patients and 5,000 more each day. Results of our real-world drug study have been referenced on 600+ peer-reviewed medical publications, including The Lancet, Mayo Clinic Proceedings, and Nature.
WARNING, DISCLAIMER, USE FOR PUBLICATION
WARNING: Please DO NOT STOP MEDICATIONS without first consulting a physician since doing so could be hazardous to your health.
Why is polymyalgia rheumatica a disease?
In addition, because the disorder occurs in older individuals, polymyalgia rheumatica may be related to the aging process.
What are the symptoms of polymyalgia rheumatica?
Additional symptoms of polymyalgia rheumatica may include muscle tenderness and weakness, low-grade fever, loss of appetite, weight loss, fatigue, a general feeling of ill health (malaise), and/or depression. In some cases, fever or weight loss may be ...
How long does polymyalgia rheumatica last?
These episodes may continue for about six months or up to six years. However, severe impairment or permanent disability, even after months or years, is rare. In most cases, individuals with polymyalgia rheumatica do ...
How old is a person with polymyalgia rheumatica?
Polymyalgia rheumatica is a rare disorder that affects twice as many females as males. Affected individuals are usually over the age of 50 years. This disorder occurs at the rate of about 50 per 100,000 in people over 50 years of age. Polymyalgia rheumatica is estimated to affect 450,000 individuals in the United States.
Why is periodic medical evaluation important?
Periodic medical evaluation is essential to screen for potential side effects of corticosteroid drugs. Individuals with polymyalgia rheumatica who also have other symptoms such as recurring headaches that may be suggestive of giant-cell arteritis, are usually placed on high-doses of corticosteroid drugs (e.g., prednisone). ...
Can you lose muscle strength with polymyalgia rheumatica?
However, severe impairment or permanent disability, even after months or years, is rare. In most cases, individuals with polymyalgia rheumatica do not experience loss of muscle strength.
Is polymyalgia rheumatica related to giant cell arteritis?
Polymyalgia rheumatica is closely related to giant cell arteritis, another inflammatory disorder. Giant cell arteritis is characterized by progressive inflammation of many arteries of the body. These two disorders have been described in the medical literature as possible variants of the same disease process.
What is the name of the condition that PMR causes?
Around 5-15 percent of those with PMR will go on to develop a condition called giant cell arteritis (GCA), also referred to as temporal arteritis (TA). Nearly half of those who are first diagnosed with GCA also have symptoms consistent with PMR.
What are the symptoms of PMR?
Other symptoms often experienced by people diagnosed with PMR include: difficulty getting up from a seated position. pain that worsens with inactivity. joint and muscle aching.
What is the cause of PMR?
A frequent symptom of polymyalgia rheumatica is stiffness in the neck. While the causes of PMR are not well understood, there are many theories as to its cause. It is suggested that the condition is the result of inflammation in the joints and the sacs surrounding the joints known as the bursae. This inflammation may lead to referred pain in other ...
What is the autoimmune disease that affects the lining of the joints?
Symptoms. Diagnosis. Treatment. Polymyalgia rheumatica is a rheumatic autoimmune inflammatory disease that affects the lining of the joints or around the joints (periarthritis) and, in rare cases, the arteries. When polymyalgia rheumatica (PMR) occurs, the body’s immune system attacks its own connective tissues, ...
How long does PMR last?
The disease can last for up to 5 years but usually less and is responsive to low to moderate doses of prednisone (steroid).
What age does PMR start?
On average, the disease tends to develop around the age of 70. The inflammation caused by PMR can lead to generalized aching, stiffness, and flu-like symptoms in both sides of the body. The most commonly affected joints are the shoulders or shoulder girdle and the hips or hip girdle.
How long does it take for PMR to show symptoms?
People with PMR may experience a rapid onset of symptoms, which develop over a few days or weeks. In some cases, the symptoms occur overnight, and the pain and stiffness are severe.
What happens if you have a PMR?
If you have an inflammation disorder like PMR, your body fights its own joints and tissues, even when germs aren’t present.
How to help PMR?
Exercise . If you have PMR, it’s important to make time for physical activity. You may need to avoid strenuous activities, but light exercise can help improve your symptoms and overall sense of well-being. Some exercises may also help you prevent side effects from medications you’re taking.
What is PMR in the body?
Overview. Polymyalgia rheumatica (PMR) is a common inflammatory disorder that causes pain, usually in your shoulders and upper body. Inflammation is your body’s natural response when it’s trying to protect you from harmful germs. Inflammation works by drawing extra blood and white blood cells to whatever part of your body it’s trying to defend.
Can eating a lot of food cause PMR?
A healthy diet is important for everyone, but if you have PMR, the foods you eat may have an impact on your symptoms. That’s because some foods are more likely to cause inflammation in your body. Keep reading to learn more about the types of foods you should eat and the types you may want to avoid.
Does eating right help with PMR?
Eating the right food can support your immune system and may even prevent inflammation before it starts. Some foods may also fight potential side effects from medications you’re taking for your PMR. These side effects can include:
Is PMR better or worse?
bruising. cataracts. No diet is proven to make PMR significantly better or worse for most people, and everyone reacts differently to foods. Pay attention to what foods seem to help you feel your best and keep track of them. It’s also important to have a well-balanced diet and to eat from all major food groups.
Overview
Symptoms
- The symptoms often appear suddenly and tend to be worse in the morning. Some people with polymyalgia rheumatica are also diagnosed with a related disorder called temporal arteritis. This condition causes inflammation of the blood vessels in the scalp, neck, and arms. Temporal arteritis can also cause headaches, jaw pain, and vision problems. Pain a...
Epidemiology
- Polymyalgia rheumatica typically affects people over age 65. It rarely develops in those under age 50. Polymyalgia rheumatica is also more likely to occur in women than in men. People of Northern European and Scandinavian descent are at a higher risk for the condition as well.
Causes
- The cause of polymyalgia rheumatica isnt known. However, its believed that certain genes and gene variations may increase your risk of developing polymyalgia rheumatica. Environmental factors may also play a role in the development of the disorder. New cases of polymyalgia rheumatic are often diagnosed in cycles and usually occur seasonally. This suggests that there …
Diagnosis
- The symptoms of polymyalgia rheumatica can be similar to those of other inflammatory conditions, including lupus and arthritis. To make an accurate diagnosis, your doctor will perform a physical exam and run several tests to check for inflammation and blood abnormalities. During the exam, your doctor may gently move your neck, arms, and legs to evaluate your range of moti…
Treatment
- Theres no cure for polymyalgia rheumatica. With the proper treatment, however, symptoms can improve in as little as 24 to 48 hours. Your doctor will prescribe a low-dose corticosteroid, such as prednisone, to help reduce inflammation. The typical dosage is 10 to 30 milligrams per day. Over-the-counter pain medications, such as ibuprofen and naproxen, arent effective in treating the sy…
Risks
- Although corticosteroids are effective in treating polymyalgia rheumatica, these drugs do have side effects. Long-term use of these medications increases your risk of:
Prevention
- Making healthy lifestyle choices can also help reduce the side effects of corticosteroids. Eating a healthy diet and limiting your salt intake can help prevent high blood pressure. Regular exercise can help strengthen your bones and muscles and prevent weight gain.
Prognosis
- Theres no cure for polymyalgia rheumatica. However, polymyalgia rheumatica often improves once treatment is received. In fact, the condition typically goes away after two to six years of treatment.