What is a sputum culture?
Other Tests A sputum cultureis a sample of the gooey substance that often comes up from your chest when you have an infection in your lungsor airways. It is mostly made up of white blood cells that fight infection mixed with germs. Doctors use it to figure out what might be causing your illness, whether it’s bacteria, a virus or something else.
How much does a sputum culture test cost?
There is no fixed price for a sputum culture test. Instead, the cost depends on multiple factors including: Charges for testing can include fees for services provided by the doctor during consultation, the health care provider who collects the sputum sample, and the laboratory that performs the test.
How sensitive are sputum-based tests?
Sensitivity of sputum-based tests depends on the bacillary burden of MTB in sputum specimens, and therefore presenting sensitivity estimates separately by smear status is essential to gauge performance in the most difficult-to-diagnose patients and to estimate the potential incremental yield over conventional sputum smear microscopy [ 22 ].
How accurate is sputum culture for the diagnosis of S pneumoniae?
The presence of gram-positive diplococci in gram-stained samples was highly specific (with a specificity of 97.6% and a positive predictive value of 91%) for the persence of S pneumoniae in sputum culture; however, even in patients with bacteremia, sputum provided a diagnosis in only 17.3% of the cases.
What can be detected from a sputum sample?
A sputum culture is most often used to: Find and diagnose bacteria or fungi that may be causing an infection in the lungs or airways. See if a chronic illness of the lungs has worsened. See if treatment for an infection is working.
Can sputum culture detect virus?
Results from a sputum test Your sputum sample will be sent to a laboratory within one to hours of production. A pathologist will run tests to determine if the growth is a bacterium, virus or fungus.
Does a positive sputum culture mean pneumonia?
Abnormal findings on a sputum culture may support a diagnosis of a lung condition like pneumonia, tuberculosis, or bronchiectasis that is tied to an underlying infection. However, a normal or abnormal result is not a definitive diagnosis and must be interpreted carefully by your doctor.
Are sputum cultures required to diagnose pneumonia?
Sputum culture is the most common test needed to be performed when the patient has pneumonia. It is used to identify the bacteria or fungi causing the airways or lung infection.
What happens if sputum test is positive?
A sample of sputum is added to a substance that promotes the growth of bacteria. If no bacteria grow, the culture is negative. If bacteria grow, the culture is positive. If TB bacteria grow, then the person has tuberculosis.
What if my sputum test is negative?
When a patient is “culture negative,” there are no detectable TB organisms in his/her sputum and the patient is considered completely non-contagious. The likelihood of transmission derives primarily from factors related to the TB patient or the environments in which contacts are exposed.
When is sputum culture indicated?
But you might need to give a sputum culture if: Your cough suggests you have an illness caused by bacteria, such as bronchitis, pneumonia or tuberculosis (a potentially serious infection that usually affects your lungs and can cause you to cough up blood).
What is the best time of day to obtain a sputum specimen?
Sputum specimens should be collected in the early morning if possible. Collect 3 sputum specimens on 3 consecutive days unless otherwise instructed. Specimens should be kept in the refrigerator until they are submitted to the laboratory.
Does green sputum mean bacterial infection?
Coughing that starts out dry is often the first sign of acute bronchitis. Small amounts of white mucus may be coughed up if the bronchitis is viral. If the color of the mucus changes to green or yellow, it may be a sign that a bacterial infection has also set in.
How much does a sputum culture cost?
How Much Does a Sputum Culture Cost? On MDsave, the cost of a Sputum Culture ranges from $15 to $72. Those on high deductible health plans or without insurance can save when they buy their procedure upfront through MDsave.
How long does a sputum culture take for pneumonia?
Test results may take from 1 day to several weeks. How long your results take depends on the type of infection your doctor thinks you may have. Some organisms don't grow in a standard culture and need a special growth medium to be found in a sputum culture. (Examples are Chlamydophila pneumoniae and mycoplasma.)
What does white blood cells in sputum mean?
In general, physicians believe that the presence of bacterial engulfment in white blood cells (WBCs) on Gram-stained sputum is a hallmark of lower respiratory infection.
What bacteria is found in sputum?
The most common pathogens detected with a sputum culture are bacteria such as Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus, and Klebsiella species. Fungi are slow-growing eukaryotic organisms that can grow on living or nonliving organisms and are subdivided into molds and yeasts.
Why is sputum test necessary?
Why is a sputum test necessary? Your doctor wants to collect some of the sputum ("phlegm") that you cough up from your lungs. The laboratory will test the sputum for tuberculosis (TB) germs. Checking your sputum is the best way to find out if you have TB disease.
When is the best time to collect a sputum culture?
Sputum specimens should be collected in the early morning if possible. Collect 3 sputum specimens on 3 consecutive days unless otherwise instructed. Specimens should be kept in the refrigerator until they are submitted to the laboratory.
Does green sputum mean bacterial infection?
Coughing that starts out dry is often the first sign of acute bronchitis. Small amounts of white mucus may be coughed up if the bronchitis is viral. If the color of the mucus changes to green or yellow, it may be a sign that a bacterial infection has also set in.
What is a bacterial sputum culture?
A bacterial sputum culture is used to detect and diagnose bacterial lower respiratory tract infections such as bacterial pneumonia or bronchitis. It is typically performed with a Gram stain to identify the bacteria causing a person’s infection.
What is the first step in sputum analysis?
Typically, the first step in the routine analysis of a sputum sample is a Gram stain to identify the general type of bacteria that may be present. The sample is then placed on or in appropriate nutrient media and incubated. The media encourages the growth of bacteria that are present, allowing for further testing and identification.
What does a positive culture report indicate?
A positive culture report typically identifies the pathogen that was detected.
Why do we need antimicrobial susceptibility testing?
Antimicrobial susceptibility testing is frequently required to guide the treatment and to determine whether the bacteria present are likely to respond to specific antibiotics.
What is testing.com?
Testing.com is an award-winning patient education website offering information on laboratory tests. The content on the site, which has been reviewed by laboratory scientists and other medical professionals, provides general explanations of what results might mean for each test listed on the site, such as what a high or low value might suggest to your healthcare practitioner about your health or medical condition.
How long should you wait to rinse your mouth before collecting a blood sample?
You may be instructed to rinse your mouth out with water prior to collection and to avoid food for 1-2 hours before the sample is collected.
Why is there variability in lab tests?
While accuracy of laboratory testing has significantly evolved over the past few decades, some lab-to-lab variability can occur due to differences in testing equipment, chemical reagents, and techniques. This is a reason why so few reference ranges are provided on this site. It is important to know that you must use the range supplied by the laboratory that performed your test to evaluate whether your results are “within normal limits.”
How to obtain sputum culture?
Samples for sputum culture may be obtained noninvasively, via tracheal aspiration, or invasively with bronchoscopy and either bronchoalveolar lavage (BAL) or a protected specimen brush (PSB). Positive tracheal cultures may reflect simple tracheal colonization, and overestimate the rate of pneumonia. Invasive cultures are more accurate in diagnosing pneumonia. In one multicenter, randomized trial of 413 patients, those receiving invasive, bronchoscopic management had a lower mortality at day 14, but not at 28, and lower mean sepsis-related organ failure assessment scores on days 3 and 7. At 28 days, the invasive management group had significantly more antibiotic-free days (11 ± 6 vs. 7 ± 7). A multivariate analysis showed a significant difference in mortality (hazard ratio 1.54, 95% confidence interval 1.10–2.16). Both BAL and PSB have sensitivities and specificities greater than 80%. Studies have shown these two techniques yield similar results (Table 3 ).
What is expected sputum culture?
Expectorated (sometimes induced) sputum cultures or cultures obtained at bronchoscopy and lavage will be required to identify resistant pathogens. Pseudomonas aeruginosa is almost impossible to eradicate from patients with bronchiectasis. Strategies for suppression are noted in the previous paragraph. Treatment of ABPA includes augmentation or introduction of systemic steroids. Itraconazole, 400 mg daily, may reduce the burden of Aspergillus but is less effective in individuals with bronchiectasis (see Chapter 52 ). Decisions about the diagnosis and therapy of Mycobacterium avium complex (MAC) are discussed in a Statement of the American Thoracic Society. Therapy with a macrolide, rifampin or rifabutin, and ethambutol is required for many months (see Chapter 31 ).
How long does it take for sputum to turn negative?
Sputum cultures should have converted to negative within 2–3 months of chemotherapy in 75–90% of patients taking a regimen that includes isoniazid and rifampin. Failure of the sputum cultures to become negative by this time should prompt further investigation, and may indicate that either the patient is not taking the drugs or the organisms are resistant to the drugs being used. Patients who continue to have M. tuberculosis in their sputum after 2–3 months of treatment should be started on DOT, if not already being supervised in this manner, and should have drug susceptibility tests performed. If resistance is found, the regimen should be modified based on the results. If sputum samples are still positive after 4 months of therapy, the regimen should be considered to have failed and a new regimen begun, ideally, based on recent drug susceptibility test results ( Nahid et al., 2016 ).
What is the pooled rate of SCC?
In patients with M. kansasii, a meta-analysis of 6 previous studies reported a pooled rate of SCC of 80.2% (95% CI, 58.4%–95.2%) ( Diel et al., 2017 ).
What is the threshold for a positive culture?
Most studies involving BAL have used 10 4 or 10 5 CFU/ml as the threshold for a positive culture. The presence of numerous squamous epithelial cells suggests upper pharyngeal contamination, and calls into question the utility of the specimen. The presence of intracellular organisms can be detected by Gram stain, and is particularly useful as it provides a rapid result with high predictive value (see Table 3 ).
Which bacteria grow in sputum culture?
Sputum culture grew Pseudomonas aerugionosa in more than 60% of patients, and Hemophilus influenzae, Klebsiella pneumonia, and Streptococcus pneumoniae in a smaller percentage of patients.
When was supraglottitis first reported?
Fulminant meningococcal supraglottitis was first reported in 1995 , with five more reports subsequently, and is characterized by fever, sore throat, muffled voice, and dysphagia with swollen supraglottic tissues seen on fiberoptic laryngoscopy, plain films, or cervical CT scans. 63
What is a sputum culture?
A sputum culture is a test that checks for bacteria or another type of organism that may be causing an infection in your lungs or the airways leading to the lungs. Sputum, also known as phlegm, is a thick type of mucus made in your lungs. If you have an infection or chronic illness affecting the lungs or airways, it can make you cough up sputum.
What happens during a sputum culture?
Your health care provider will need to get a sample of your sputum. During the test:
Will I need to do anything to prepare for the test?
You may need to rinse your mouth out with water before the sample is taken. If you will be getting a bronchoscopy, you may be asked to fast ( not eat or drink) for one to two hours before the test.
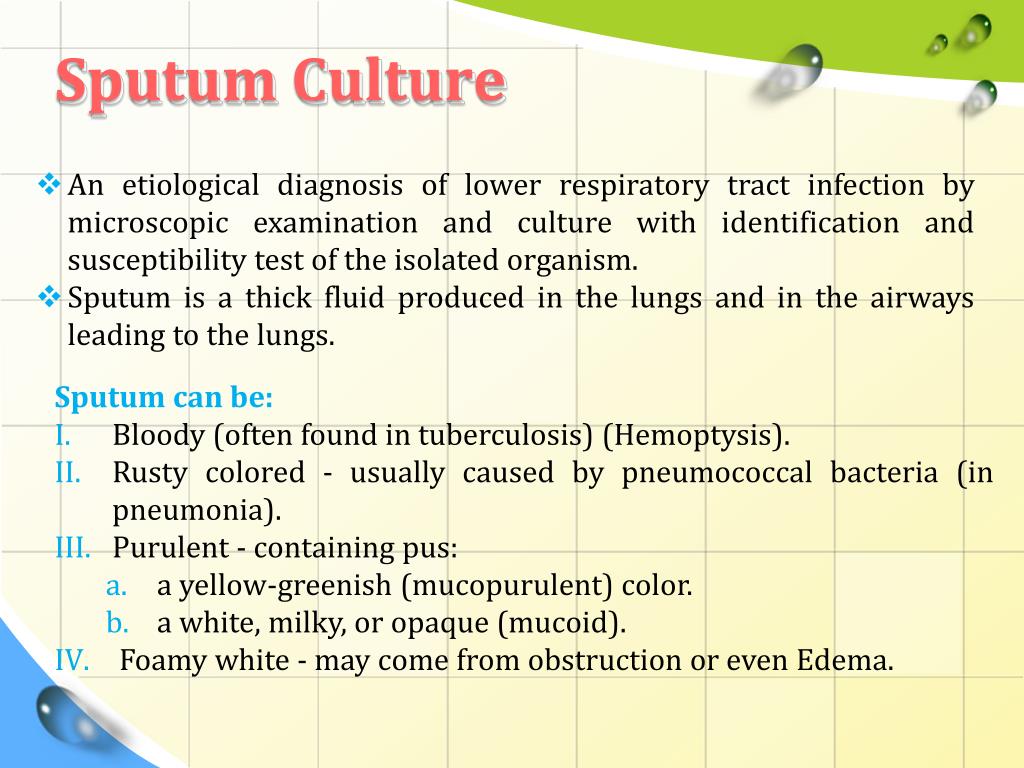
What does it mean when sputum is clear?
Clear. This usually means no disease is present, but large amounts of clear sputum may be a sign of lung disease.
Why is sputum color important?
The thickness of sputum helps trap the foreign material. This allows cilia (tiny hairs) in the airways to push it through the mouth and be coughed out. Sputum can be one of several different colors. The colors can help identify the type of infection you may have or if a chronic illness has become worse: Clear.
What causes yellowish green sputum?
Yellowish-green sputum is also common in people with cystic fibrosis. Cystic fibrosis is an inherited disease that causes mucus to build up in the lungs and other organs. Brown. This often shows up in people who smoke. It is also a common sign of black lung disease.
What are the most common types of bacteria found in sputum culture?
The most common types of harmful bacteria found in a sputum culture include those that cause: Pneumonia. Bronchitis. Tuberculosis. An abnormal sputum culture result may also mean a flare-up of a chronic condition, such as cystic fibrosis or chronic obstructive pulmonary disease (COPD).
What is sputum culture?
Sputum analysis and culture is the most common method of specific diagnosis of lower respiratory tract infections. Culture of a properly screened, expectorated sputum sample will identify the pathogen in most cases of bacterial pneumonia. Expectorated sputa, as well as those obtained by aspiration from the upper airway, are subject to oropharyngeal bacterial contamination. Other techniques, such as transtracheal aspiration, are more "sterile," but have a much higher incidence of morbidity. Microscopic screening of expectorated or aspirated sputum samples will reduce the number and increase the diagnostic accuracy of cultures, resulting in considerable cost savings. Mucopurulent material is selected by gross inspection, and microscopic examination of a wet mount and Gram stain yields information about cell type and predominant organism. More important, however, the presence of fewer than 25 squamous epithelial cells per low-power field indicates that true lower respiratory tract secretions have been collected. Culture results must be correlated carefully with semiquantitative grading, initial microscopic screening, clinical presentation, and response to initial therapy. When properly performed and interpreted, sputum analysis and culture are valuable tools in the diagnosis and treatment of lower respiratory tract infection.
What is sputum analysis?
Sputum analysis and culture is the most common method of specific diagnosis of lower respiratory tract infections. Culture of a properly screened, expectorated sputum sample will identify the pathogen in most cases of bacterial pneumonia. Expectorated sputa, as well as those obtained by aspiration f …
What is a sputum culture?
If you experience any of these symptoms, your doctor may recommend a sputum culture. This fast, relatively painless test helps laboratory technicians study the bacteria or fungi that might be growing in your lungs and causing the production of the sputum. This can help them find the cause of your illness. Often the most difficult part of ...
How to get a good sputum sample?
There are a few techniques you can try to get a good sputum sample, however. Drinking plenty of fluids can help loosen the secretions and make it easier to cough up sputum. Your doctor may ask you to rinse out your mouth with clear water to help get rid of any other bacteria and extra saliva.
How much sputum do you need for a lab?
The laboratory needs at least 2 milliliters of sputum for testing. To cough deeply from your lungs, you might need to take three deep breaths before you cough forcefully. If you’re having trouble coughing up enough sputum, your doctor may try tapping on your chest to loosen the sputum.
How long does it take for a sputum sample to be taken to the lab?
Once you’ve produced a sputum sample for analyzing, it should be taken to the laboratory within one to two hours of coughing it up. The laboratory will place the sample on a special plate that has a nutrient that helps bacteria or other pathogens present in your sputum grow.
Where does sputum collect?
Sputum collects in the lower parts of your lungs and bronchi, which are the tube-like pathways that air moves through to reach your lungs. Symptoms that may indicate the need for a sputum culture test include: The test can reveal what may be causing the cough and other symptoms. These include:
Can you test saliva from your lungs?
You simply need to provide the sample for the lab to test. You’ll be asked to cough deeply to bring up the sputum from your lungs. Saliva that can come up when someone is asked to cough is typically from the mouth and upper airways and isn’t useful for this test.
Can you cough after giving a sputum sample?
When you aren’t feeling well, the deep coughing associated with a sputum culture may feel uncomfortable. You may experience some chest discomfort after giving the sample.
Why do we do sputum culture?
Clinical diagnostic sputum tests aim to detect the causes of lower respiratory tract infections and some other diseases. It also provides an efficacious tool for monitoring the effectiveness of clinical treatment. Sputum culture is the most common test needed to be performed when the patient has pneumonia. It is used to identify the bacteria or fungi causing the airways or lung infection.
Why is it important to collect a sputum sample?
Collecting a good quality sputum sample is the first step for getting an , the pathogens identified from sputum culture do not always originate from lower respiratory tract infections because they may be part of contaminant sites or preexisting in the oral flora. Thus, standard microbiological procedures for organisms' isolation and identification are critical for the sputum quality assessment (QA).
What is a sputum smear microscopy?
Sputum smear microscopy is the initial step taken in laboratory sputum analysis. It is a fast and inexpensive technique, precisely, in resource-limited settings. Gram stain is used to differentiate bacteria into two broad groups (gram-positive and gram-negative microorganisms). The Gram stain is the first staining technique performed in preliminary bacterial identification, which helps determine if there is an adequate amount of pathogens in the culture and make a definitive diagnosis. It is also crucial because it can address antibiotic therapy more specifically. With the Gram stain, the bacterial species are distinguished into gram-positive and gram-negative groups by the differences of cell walls' physical and chemical properties. Some bacteria have a thick peptidoglycan layer cell wall stained with crystal violet (gram-positive).
How to use a nebulizer cup?
Moreover, the patients wear the nebulizer cup to cover the face and nose after sitting in an upright position. The patients inhale and exhale through the mouthpiece. An expectorate saliva into an emesis bowl and expectorate sputum coughed up are collected into a sterile well-closed container. The medical staff turns on the nebulizer device to allow the patient to inhale the hypertonic mist for approximately five minutes. Then the patients take several deep breaths before attempting to cough. If there are difficulties for the patients to cough up the sputum, the medical staff may use gentle chest physiotherapy to aid the patients to produce sputum. During the procedure, the patients should be observed closely by the medical staff to identify any potential rupture of pleural bullae, triggering a life-threatening pneumothorax. The patients should stop when 1 to 2 mL sputum specimen is collected for each sample or reach 15 minutes of nebulization, or the patient complains of chest tightness, dyspnoea, or wheeze. Imaging is advised if there is the persistence of these symptoms at the end of the sputum collection.
How is sputum induction used?
Sputum inductionis a procedure used to collect adequate lower respiratory secretions from patients who have trouble producing sputum to aid the diagnosis of TB. In particular, patients with suspicion of miliary tuberculosis and/or tuberculous pleural effusion are often targeted using this adjuvant procedure. In such settings, the patient inhales nebulized hypertonic saline solution to liquefy airway secretions. This solution stimulates the patient coughing and promotes expectoration of airway secretions. The medical professionals prepare a 20 ml 3% hypertonic saline solution and inject it into the nebulizer cup filled with water. Similar to the non-adjuvant procedure, the patients are always required to wash their mouth thoroughly.
Why is sputum important in medicine?
The sputum is examined grossly and microscopically to aid medical diagnosis. The sputum contains various cells and molecular compounds such as soluble lipids and proteins. Its analysis is crucial in medicine. The sputum analysis involves an analytical approach to investigate the cellular and acellular components expelled from the patient's upper respiratory tract. This procedure is essential in the evaluation and management of lower respiratory infections or other longstanding health conditions.[1] Clinically, sputum molecular biomarkers or gene sequencing of the microorganisms have increased medicine accuracy and represent a milestone in the current evaluations of the algorithms running for precision medicine.
How to identify a suspected organism?
To identify a suspected organism, at first, the bacteria will be inoculated in a series of differential media. Then use different indicators to observe the specific end products of metabolism inside of the medium.
Why is sputum sensitivity important?
Sensitivity of sputum-based tests depends on the bacillary burden of MTB in sputum specimens, and therefore presenting sensitivity estimates separately by smear status is essential to gauge performance in the most difficult-to-diagnose patients and to estimate the potential incremental yield over conventional sputum smear microscopy [ 22 ]. Providing accuracy estimates for PWH, children, or patients with early disease separately is also important (even if numbers are small), to allow inclusion in meta-analyses. Studies focusing specifically on these patient groups are also needed as a next step, once performance in adults with respiratory symptoms has been established.
Why is sputum smear microscopy suboptimal?
Despite its ubiquity, microscopy is suboptimal because it has low sensitivity, high interoperator variability, is largely unhelpful in extrapulmonary and childhood TB, and does not detect drug resistance [ 1–7 ].
What is the target population for a smear replacement test?
The target population for initial accuracy studies of a new smear-replacement test should be adults self-presenting with respiratory symptoms suggestive of TB (ie, passive case finding), including people living with HIV (PLHIV). For patients without HIV, cough ≥2 weeks is used to identify patients with suspected TB [ 19, 20 ], whereas less stringent criteria (cough of any duration, fever, night sweats, or weight loss) is used for PWH and other high-risk groups [ 21 ]. Adults with suspected pulmonary TB represent the optimal initial study population because (1) the reference standard (culture) has good sensitivity in this patient group, (2) it represents the largest proportion of the target population to which the test would later be applied in practice, and (3) sufficient volume of sputum can usually be obtained from such patients. Patients in whom TB has already been diagnosed by another test or who have already started on TB treatment should be excluded, because enriching with patients that are positive by sputum smear microscopy or Xpert will lead to overestimates of sensitivity of the test under investigation.
What is the need for a sputum smear test?
Tests that can replace sputum smear microscopy have been identified as a top priority diagnostic need for tuberculosis by the World Health Organization. High-quality evidence on diagnostic accuracy for tests that may meet this need is an essential requirement to inform decisions about policy and scale-up.
What is the reference standard for smear replacement?
We recommend using at least 1 automated liquid culture as the primary reference standard for diagnostic accuracy studies of smear-replacement tests (please refer to discussion on this in “Paper 1” of this series [ 25 ]), and all those who received the index test should also receive the same reference standard to avoid partial or differential verification bias. It is important to acknowledge (1) that there can be large variability of bacillary load between specimens and even within specimens and (2) that even culture is not a perfect reference standard and thus that, because new assays are becoming increasingly more sensitive, false-negative culture results need to be considered—in particular after lengthy specimen transport or overly harsh decontamination of specimens.
How does accuracy of index test differ between studies?
Accuracy estimates will vary between studies not only due to variation in patient spectrum but also as procedures for culture and microscopy var y [ 26 ]. For example, sensitivity estimates for the index test will decrease when using liquid rather than solid culture, with increasing number of cultures done, increasing number of specimens on which culture is performed, and increasing number of days on which specimens are obtained. In addition, estimates of sensitivity of the new test among smear-negative patients will be lower when (1) using a more sensitive process for smear analysis (ie, using fluorescence microscopy instead of Ziehl-Neelsen), (2) using multiple smears to classify a patient as smear negative (instead of a single smear), and (3) highly proficient operators are preparing and reading the smears.
How to evaluate TB sensitivity?
To obtain unbiased and precise estimates of sensitivity and specificity, clinical studies evaluating diagnostic test accuracy should use a cross-sectional or cohort study design, enrolling a sufficient number of consecutive or randomly selected patients requiring TB evaluation ( Figure 1 ). However, before undertaking resource-intensive prospective evaluations, case-control studies using banked specimens from well characterized cohorts and/or studies involving negative sputum specimens spiked with known numbers of Mycobacterium tuberculosis (MTB) bacilli may be performed first. It is important to note that case-control studies should avoid comparing severe cases to healthy controls that can result in overestimations of test accuracy (spectrum bias). Although such “proof-of-concept” studies are not a major focus of this document, investigators should be aware that these types of studies can play an important role in the early assessment of smear-replacement tests, particularly if they include head-to-head studies against assays with well established performance characteristics. If banked specimens are processed and stored appropriately, these specimens can be used to evaluate DNA-based tests. Once promising smear-replacement tests have been identified, they should be evaluated in clinical studies using fresh specimens collected and processed under routine conditions.
What is a sputum culture?
A sputum culture is a sample of the gooey substance that often comes up from your chest when you have an infection in your lungs or airways. It is mostly made up of white blood cells that fight infection mixed with germs.
What is a positive sputum sample?
If the sputum sample is abnormal, the results are called “positive.” Identifying the bacteria, fungus, or virus may help diagnose the cause of:
How to prepare for oropharyngeal biopsy?
Patient Preparation: Have patient rinse his/her mouth with water immediately prior to specimen collection. This reduces the number of contaminating oropharyngeal bacteria.
How many sputum samples are there for CAP?
In a study of 1669 patients with community-acquired pneumonia (CAP), bacterial pathogens could be identified in only 264 cultured sputum samples.
What is the sensitivity and specificity of gram positive diplococci?
The sensitivity and specificity of the gram-positive diplococci identification in the sputum culture of S pneumoniae were 60% and 97.6%, and the positive and negative predictive values were 91% and 85.3%, respectively (for 532 patients who provided good-quality samples, there were 103 samples with gram-positive diplococci and 157 with S pneumoniae ).
What is the specificity of diplococci in gram stained samples?
The presence of gram-positive diplococci in gram-stained samples was highly specific (with a specificity of 97.6% and a positive predictive value of 91%) for the persence of S pneumoniae in sputum culture; however, even in patients with bacteremia, sputum provided a diagnosis in only 17.3% of the cases.
How many weeks apart do you have to take a blood sample?
The standard process included 1 sputum and 2 blood sample cultures, plus evaluation of 2 serum samples, 4 to 8 weeks apart. Pleural puncture, transthoracic needle puncture, tracheobronchial aspiration (in mechanically ventilated patients), and protected specimen brush or bronchoalveolar lavage sampling were performed as needed according to clinical indication or the judgment of the attending physician.
How long does it take for a positive test to show pneumonia?
The clinical and radiographic microbiological diagnoses of pneumonia lack accuracy, 1, 2 cultures take at least 24 hours to produce a positive result, and specific rapid tests based on the detection of soluble antigens of S pneumoniae or Legionella pneumophila in body fluids are not always available.
How old are the patients in the CAP study?
The study population of 1669 consecutive patients with bacterial CAP consisted of 1095 men (65.6%) and 574 women (34.4%) ranging in age from 15 to 101 years (mean, 67 ± 18.17 years).
How many patients were treated with CAP in 2002?
From October 1996 to April 2002, 1669 consecutive patients older than 14 years with acute symptoms consistent with CAP were studied according to a standard protocol in the Respiratory and Infectious Diseases Services at the Hospital Clínic in Barcelona, Spain, a 800-bed university teaching hospital.
