
- Assigning ICD codes. Every medical code is specifically definition. Diagnosis coding accurately portrays the medical condition that a patient is experiencing.
- ICD Reports Data. Diagnostic codes are usually reported in conjunction with procedure codes. The diagnostic codes are used to justify why medical procedures are performed.
- Medical Documentation is Key. The diagnosis code assigned is assigned based on the information available to the coder when the code is assigned.
- Primary and Secondary ICD Codes. Some diagnoses are the natural complications of pre-existing conditions. In these cases, the underlying condition is the primary diagnosis.
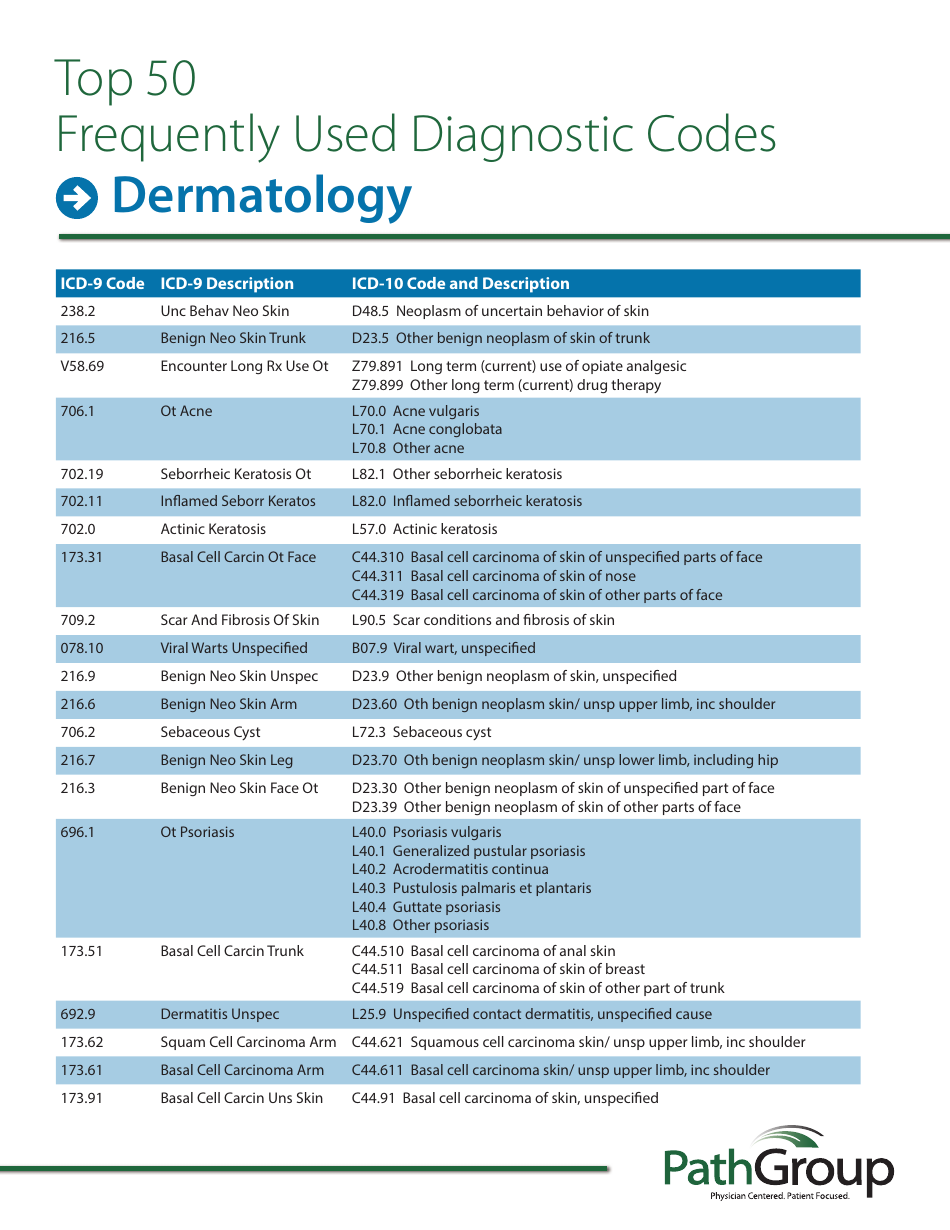
- ICD-9-CM and ICD-10 Structure. The International Classification of Diseases in every version is arranged by type of disease. The first section deals with infectious diseases.
What diagnosis codes should be reported?
Codes for signs and symptoms that are not routinely associated with a definitive diagnosis should be reported, according to ICD-10-CM guidelines 1.B.4 and I.B.5. The rash is reported because it is not related or associated with croup. Look for Croup in the ICD-10-CM Alphabetic Index referring you to code J05.0.
Which coding system is used to code diagnosis?
- Adherence to the guidelines when assigning diagnosis codes is required under HIPAA.
- ICD-10-CM diagnosis codes are adopted under HIPAA for all healthcare settings.
- Diagnoses are reported at their highest number of characters available.
Is a CPT code a diagnosis code?
The CPT codebook should be updated every 3-5 years. In a concise statement, ICD-9 is the code used to describe the condition or disease being treated, also known as the diagnosis. CPT is the code used to describe the treatment and diagnostic services provided for that diagnosis.
What is diagnosis code u07.1?
U07.1 is a billable diagnosis code used to specify a medical diagnosis of covid-19. The code U07.1 is valid during the fiscal year 2022 from October 01, 2021 through September 30, 2022 for the submission of HIPAA-covered transactions.
How are ICD codes used today?
Clinical terms coded with ICD are the main basis for health recording and statistics on disease in primary, secondary and tertiary care, as well as on cause of death certificates. These data and statistics support payment systems, service planning, administration of quality and safety, and health services research.
How do insurance companies use diagnosis codes?
ICD-10 codes identify medical diagnoses and help insurance companies understand why the care you were provided was necessary. They work in tandem with CPT Codes and are required on every claim submission. At Better, we validate the accuracy of the ICD-10 codes on every claim we file.
What is the greatest benefit of diagnosis coding?
The diagnosis code supports the medical necessity for the service and tells the payer why the service was performed. It can be the source of denial if it doesn't show the medical necessity for the service performed.
Why is the order of diagnosis codes important?
Each diagnosis code should be linked to the service (CPT) code to which it relates; this helps to establish medical necessity. Any changes to codes or to the order in which they are listed on the claim should be approved by the physician. In some cases, the ICD-9 guidelines may require that certain codes be reordered.
How important is it to provide accurate diagnosis and procedure codes to insurance claims?
When a claim is coded accurately, it lets the insurance payer know the particular illness or injury and the method of treatment that is necessary. While this may be an oversimplified explanation, it does an excellent job of stressing the vital importance of accuracy when coding.
Are ICD-10 codes used for billing?
ICD procedure codes are used only on inpatient hospital claims to capture inpatient procedures. Entities that will use the updated ICD-10 codes include hospital and professional billing, registries, clinical and hospital departments, clinical decision support systems, and patient financial services. 4.
What are ICD codes used for billing?
ICD codes, or International Classification of Disease codes, are used to describe the client's diagnosis. In other words, they refer to the condition that's being treated. ICD codes are developed by WHO, the World Health Organization, and used around the world.
What is diagnostic code?
Diagnostic coding is the translation of written descriptions of diseases, illnesses and injuries into codes from a particular classification. In medical classification, diagnosis codes are used as part of the clinical coding process alongside intervention codes. Both diagnosis and intervention codes are assigned by a health professional trained in medical classification such as a clinical coder or Health Information Manager.
Why are diagnostic codes updated?
As the knowledge of health and medical advances arise, the diagnostic codes are generally revised and updated to match the most up to date current body of knowledge in the field of health. The codes may be quite frequently revised as new knowledge is attained.
How does experience affect coding?
The experience of the health professional coding a medical record is an essential variable that must be accounted for when analysing the accuracy of coding. Generally a coder with years of experience is able to extract all the relevant information from a medical record whether it is paper, scanned or semi-electronic. The diagnoses codes selected from the extraction are generally compiled and sequenced in order to represent the admission. An experienced coder may incorrectly assign codes due a lack of application of a classification systems relevant standards. An example to highlight clinical coding experience would be the standard within the Australian Coding Standards 0010 General Abstraction Guidelines. These guidelines indicate that a coder must seek further detail within a record in order to correctly assign the correct diagnoses code. An inexperienced coder may simply just use the description from the discharge summary such as Infarction and may not use the correct detail which could be further found within the details of the medical record. This directly relates to the accuracy of diagnoses codes as the experience of the health professional coder is significant in its accuracy and contribution to finance.
How is intelligence achieved in coding?
Intelligibility of results of coding is achieved by semantic design principles and with ontologies to support navigating in the codes. One major aspect despite the fuzziness of language is the bijectivity of coding. Escape is with explaining the code structure to avoid misinterpreting and various codes for the very same condition (as e.g., yet not served at all with SNOMED3).
Why is accuracy important in diagnosis codes?
The accurate assignment of diagnoses codes in clinical coding is essential in order to effectively depict a patients stay within a typical health service area.
What is a hospital based on?
Hospitals that are based on Activity Based Funding and Diagnoses-Related Group Classification systems are often subjected to high end decision making that could affect the outcome of funding. It’s important to look at the scope of diagnoses codes in terms of their application in finance.
What is a principal diagnosis?
The principal diagnosis, additional diagnoses alongside intervention codes essentially depict a patient's admission to a hospital. Diagnoses codes are subjected to ethical considerations as they contribute to the total coded medical record in health services areas such as a hospital.
Why is it important to include diagnostic codes in a fee for service?
This information is important for CMS to identify, measure and evaluate Medicaid participants’ health and associated health care services delivery. Diagnosis codes are used in conjunction with procedure information from claims to support the medical necessity determination for the service rendered and, sometimes, to determine appropriate reimbursement. This information is critical and is associated with the T-MSIS priority item (TPI) Completeness of Key Claims Service Data Elements – TPI-20.
What should be left blank in a diagnosis code?
Any unused diagnosis code or flag field should be left blank. If the diagnosis code is blank, the corresponding diagnosis code flag should also be blank. If the diagnosis code is not blank, the corresponding diagnosis code flag should be populated with a valid value.
What is the T-MSIS document?
This document outlines the specifications for reporting diagnosis and procedure codes in T-MSIS claims files. The specifications in the guidance provide an explanation on how the data elements should be populated to ensure that diagnoses and procedures covered by Medicaid are accurately reported in the state’s T-MSIS file submission.
What is the procedure code for IP claims?
IP claims are expected to have procedure codes reported in T-MSIS as coded and identified by the medical service provider when procedures are performed during an inpatient stay. The principal procedure should be reported in T-MSIS using the PROCEDURE-CODE-1 field with secondary and other procedures reported in fields PROCEDURE-CODE-2 through 6. The fields PROCEDURE-CODE-FLAG-1 through PROCEDURE-CODE-FLAG-6 are used to indicate the type of procedure code reported by the provider and should be coded either “02” (ICD-9 CM) or “07” (ICD-10 CM PCS) [1].
Do OT claims have diagnostic codes?
Several types of services on OT claims, such as transportation services, DME, and lab work, are not expected to have diagnosis codes. However, OT claim records for medical services, such as outpatient hospital services, physicians’ services, or clinic services are generally expected to have at least one diagnosis code.
Is HHS accessible to disabled people?
HHS is committed to making its websites and documents accessible to the widest possible audience, including individuals with disabilities. We are in the process of retroactively making some documents accessible. If you need assistance accessing an accessible version of this document, please reach out to the Section 508 Help Desk.
Do all claims need to be populated with diagnosis codes?
However, not all claims and encounters require, or should be populated with diagnosis and procedure codes. This can lead to confusion in how states should submit data to T-MSIS. This guidance is intended to address that confusion.
Why are diagnostic codes used?
Diagnostic codes are usually reported in conjunction with procedure codes. The diagnostic codes are used to justify why medical procedures are performed. There are situations when diagnostic codes are reported for purposes other than reimbursement, such as statistical reporting to federal and state health agencies, when submitting reports for drug trials, or for tracking purposes within a healthcare institution to identify patient population needs and trends.
How is the diagnosis code assigned?
The diagnosis code assigned is assigned based on the information available to the coder when the code is assigned . Many dermatologists, for example, bill the procedure code for a skin lesion of uncertain behavior without waiting for a pathology report. If the dermatologist has a strong suspicion of malignancy, he or she may wait until the definitive diagnosis is achieved to support his or her claim of excision of a malignant lesion. As one may assume, the care taken to excise a malignant skin tumor is more extensive than that taken to excise a benign skin fibroma. In the outpatient setting, it is illegal to assign an ICD diagnosis code without definitive documentation that a condition exists. There are many rules to remember.
What is the ICD-10 system?
The International Classification of Diseases is a medical coding system devised by the United Nations’ World Health Organization. The United States is the last industrial country to use the 9th version of ICD. All other advanced healthcare economies have already implemented ICD-10. Each country adapts ICD to its particular needs.
What is the ICd 9 code?
Due to the Health Insurance Portability and Accountability Act of 1996 (HIPPA), ICD-9-CM is mandated as the only set of codes to be used for reporting medical services in the United States. Barring any changes in mandate, ICD-10 will replace ICD-9-CM in 2013. The two coding systems are similar, and medical billers and medical coders who are fluent ...
What is the code for a GI bleed?
In the outpatient setting, when a healthcare provider suspects a condition, such as a gastrointestinal hemorrhage in a patient, a diagnosis code is not assigned to describe a GI bleed until it is confirmed. The patient will usually undergo a radiological or endoscopic examination to confirm the existence and location of the bleed. At the first encounter, when the patient presents with only a complaint of tarry, black stool, the code 578.1 is used to describe why the patient was examined and the plan of care was devised. The healthcare provider may suspect a hemorrhage in the jejunum, but without direct evidence, he or she assigns the code for blood in the stool and orders a radiological test. The patient is referred to a radiologist who identifies a hemorrhage in the sigmoid colon. Because the radiologist has made a definitive diagnosis, he or she reports the reason for the encounter as being 556.5, left-sided, ulcerative colitis. With the radiologist’s report in hand, the primary care provider follows up with the patient, with the confirmed diagnosis of 556.5, and devises a plan of care. For this follow-up encounter, 556.5 is used to explain the cause for medical intervention.
What is diagnostic code?
Every medical code is specifically definition. Diagnosis coding accurately portrays the medical condition that a patient is experiencing. Like all medical codes, ICD diagnostic codes are intended to convey an exact aspect of medical information. ICD diagnostic coding accurately reflects a healthcare providers findings. A healthcare provider’s progress note is composed of four component parts. Firstly, comes the patient’s chief complaint, the reason that initiates the healthcare encounter. Secondly, the provider documents his or observations. This includes a review of the patient’s history, a review of pertinent medical systems, and a physical examination. Following these, the healthcare provider renders an assessment in the form of a diagnosis, and a plan of care.
What is the name of the doctor who diagnoses a hemorrhage in the sigmoid colon?
The patient is referred to a radiologist who identifies a hemorrhage in the sigmoid colon.
What is the ICD code used for?
ICD codes are also used in clinical trials to recruit and track subjects and are sometimes, though not always, included on death certificates. 4
Why is it important to know the ICD code?
Having the right code is important for being reimbursed for medical expenses and ensuring the standardized treatment for your medical issue is delivered.
What is CPT code?
When your doctor submits a bill to insurance for reimbursement, each service is described by a common procedural technology (CPT) code, which is matched to an ICD code. If the two codes don't align correctly with each other, payment may be rejected.
Why use ICD-10?
ICD codes are used globally to track health statistics and causes of death. This is helpful for gathering data on chronic illnesses as well as new ones. For example, a new code was added to the ICD-10 in 2020 to track vaping-related illnesses. 3
How many ICD-10 codes are there?
The 10th version of the code, in use since 2015, is called the ICD-10 and contains more than 70,000 disease codes. 1 The ICD is maintained by the World Health Organization (WHO) and distributed in countries across the globe.
How many digits are in an ICD-9?
Most ICD-9 codes are three digits to the left of a decimal point and one or two digits to the right of one. For example:
When will the ICD-10-CM be updated?
The ICD receives annual updates in between revisions, which is sometimes reflected in the code title. For example, the 2020 updated version is the ICD-10-CM. The ICD-11 was approved by the WHO in 2019 and goes into effect in 2022. 2
Why do we use medical codes?
Medical codes are used to describe diagnoses and treatments, determine costs, and reimbursements, and relate one disease or drug to another. Patients can use medical codes to learn more about their diagnosis, the services their practitioner has provided, figure out how much their providers were paid, or even to double-check their billing ...
What is the ICD?
International Classification of Diseases (ICD) is published by the World Health Organization (WHO). This diagnostic classification system is the international standard for reporting diseases and health conditions. It uses death certificates and hospital records to count deaths, as well as injuries and symptoms.
What is a level 1 HCPCS code?
Level I HCPCS codes mirror CPT codes and are used to identify medical services and procedures ordered by physicians or other licensed professionals.
Why do you look at CPT codes?
Patients may be interested in looking at CPT codes to better understand the services their doctor provided, to double-check their bills, or negotiate lower pricing for their healthcare services.
What is the ICD classification of health?
The International Classification of Functioning, Disability, and Health, commonly known as ICF, is a framework for measuring health and disability related to a health condition. 4 Where the ICD classifies disease, the ICF looks at how functional a person is in their environment.
What is CPT code?
Current Procedural Terminology (CPT) codes are developed by the American Medical Association to describe every type of service (i.e., tests, surgeries, evaluations, and any other medical procedures) a healthcare provider provides to a patient. 1 They are submitted to insurance, Medicare, or other payers for reimbursement purposes.
How many DRGs are there?
The assumption is made that patients that fit the same profile will need approximately the same care and services. There are about 500 different DRGs. They are updated annually to add new diagnoses or circumstances.

Overview
In health care, diagnosis codes are used as a tool to group and identify diseases, disorders, symptoms, poisonings, adverse effects of drugs and chemicals, injuries and other reasons for patient encounters. Diagnostic coding is the translation of written descriptions of diseases, illnesses and injuries into codes from a particular classification. In medical classification, diagnosis codes are used as part of the clinical coding process alongside intervention codes. Both diagnosi…
Financial aspects of diagnostic coding
Diagnosis codes are generally used as a representation of admitted episodes in health care settings. The principal diagnosis, additional diagnoses alongside intervention codes essentially depict a patient's admission to a hospital.
Diagnoses codes are subjected to ethical considerations as they contribute to the total coded medical record in health services areas such as a hospital. Hospitals that are based on Activity …
Factors affecting accuracy in diagnostic coding
Accuracy is a major component in diagnoses codes. The accurate assignment of diagnoses codes in clinical coding is essential in order to effectively depict a patients stay within a typical health service area. A number of factors can contribute to the overall accuracy coding which includes medical record legibility, physician documentation, clinical coder experience, financial decision making, miscoding, as well as classification system limitations.
Weaknesses in diagnostic coding
Generally, coding is a concept of modeling reality with reduced effort, but with physical copying.
• Hence, the result of coding is a reduction to the scope of representation as far as possible to be depicted with the chosen modeling technology. There will never be an escape, but choosing more than one model to serve more than one purpose. That led to various code derivatives, all of them using one basic reference code for ordering, as e.g., with ICD-10 coding. However, concurrent d…
See also
• Systematized Nomenclature of Medicine
• Diagnosis-related group
• Medical classification
• Major Diagnostic Category