What drugs affect T4 and T3?
Several drugs that are widely used in clinical practice (e.g., glucocorticoids, amiodarone, propranolol) inhibit the conversion of T4 to T3 in peripheral tissues. As expected, their most profound effect on thyroid function is a decrease in the serum concentration of T3, usually with a concomitant increase in the rT3 level. An increase in the serum T4 concentration has been observed on occasion. When intrapituitary T4-to-T3 conversion is inhibited, the serum TSH concentration may rise. In the absence of inherent abnormalities in thyroid hormone synthesis or in its secretion, TSH levels should return to normal, and hypothyroidism should not ensue from the chronic administration of compounds that only partially interfere with T 4 monodeiodination. Other mechanisms by which some compounds affect the extrathyroidal metabolism of thyroid hormone involve acceleration of the overall rates of the deiodinative and non-deiodinative routes of hormone disposal. An example of a drug that acts principally through the former mechanism is phenobarbital, 252 and one that acts by way of the latter is diphenylhydantoin. 253 In such circumstances, thyroid hormone concentrations should remain unaltered. Furthermore, it has been anticipated, as well as observed, that hypothyroid patients who receive such drugs require higher doses of exogenous hormone to maintain a eumetabolic state. Some drugs have multiple effects.
How does the extrathyroid system regulate thyroid hormone?
The extrathyroidal systems that mediate thyroid hormone uptake and metabolism work in concert with the hypothalamic-pituitary-thyroid axis to regulate the availability and thus influence the action of thyroid hormones in peripheral tissues. The presence and activity of these metabolic pathways differ significantly between tissues and with developmental state, thus allowing T 3 content to vary from organ to organ, and even from cell type to cell type. These prereceptor processes represent critical adaptive mechanisms that help to maintain T 3 homeostasis in response to environmental and internal stresses. Knowledge of these pathways is important for understanding the changes in tissue and plasma thyroid hormone levels that accompany a variety of thyroidal and nonthyroidal diseases, as well as for optimizing therapy for hypothyroidism and hyperthyroidism. Further studies will likely provide additional insight into the biochemistry and physiologic roles of the enzymes and transporters that mediate these important homeostatic processes.
What are genetically modified mice?
Genetically modified mice are a powerful tool to investigate the individual components of thyroid hormone transport, metabolism and action, and their contributions to skeletal physiology (Table 46.1 ). Thyroid hormone transporters are necessary for the active transport of thyroid hormones into cells. Mice lacking the thyroid hormone transporter MCT8 have elevated T3 but decreased T4 levels [60]. Mct8y/− mice have only a minor delay in postnatal growth suggesting that other transporters may compensate for deficiency of MCT8 [61]. Nevertheless, analysis of Mct8 knockout mice revealed delayed endochondral ossification due to impaired T3 signaling in chondrocytes, and Mct8y/− mice also exhibited decreased bone mineralization and strength in adulthood [62]. Although MCT8 is important for endochondral ossification and adult bone maintenance, other studies provide further evidence to suggest functional redundancy between thyroid hormone transporters in the skeleton. Thus although Mct10 mutant mice and Oatp1c1−/− knockout mice have normal weight gain and linear growth, Mct8 and Oatp1c1 double knockout mice display significant postnatal growth retardation [63–65].
What is the second type of JH transport molecule?
A second type of high affinity, high molecular weight JH transport molecule has been discovered, having the characteristics of a hexamerin . The hexamerins, composed of six 70–80 kDa subunits, are widely distributed throughout the phylum Arthropoda and have been found in insects, crustaceans, and certain chelicerates ( Burmester, 2002 ); however, they are not typically employed as hemolymph JH transporters. To date, only species in the order Orthoptera, including L. migratoria ( Koopmanschap and deKort, 1988; Braun and Wyatt, 1996) and Melanoplus sanguinipes ( Ismail and Gillott, 1995 ), are known to exploit hexamerins as JH transport proteins.
What is the transporter protein for thyroid hormone?
The progress in the field of transmembrane thyroid hormone transport has been truly astonishing. It has been assumed for a long time that transport of iodothyronines across the plasma membrane occurs by passive diffusion, but it has become increasingly clear that cellular uptake and efflux of thyroid hormone is mediated by transporter protein.66 Several specific thyroid hormone transporters have been identified, including monocarboxylate transporter 8 (MCT8), MCT10, and organic anion transporting polypeptide 1C1 (OATP1C1). MCT8 and MCT10 are expressed in multiple tissues where they facilitate transport of T 3, T 4, rT 3, and T 2 across cell membranes; OATP1C1 is expressed predominantly in the brain and transports preferentially T 4, wherein it may mediate the entry of T 4 into the astrocytes. A defect in a single thyroid hormone transporter molecule, MCT8, has been shown to cause a severe developmental neurologic phenotype. 66,62 The Allan-Herndon-Dudley syndrome (AHDS) is an X-linked condition characterized by severe mental retardation, dysarthria, athetoid movements, muscle hypoplasia, and spastic paraplegia associated with an elevated serum T 3. All patients tested with this syndrome have mutations in the MCT8 gene. 63,67 More than 200 individuals belonging to some 100 families of all races and diverse ethnic origins harboring more than 70 different mutations have been identified. 68 Although most mutations resulted in a complete functional inactivation of the MCT8 protein, significant residual activity was observed with a number of MCT8 mutations, some of which associated with a milder clinical phenotype. 69 Surprisingly, MCT8-null mice, despite the presence of marked increased T 3 levels, lack any overt neurologic abnormalities, a rather unexpected finding in light of the severe human phenotype. 70,71 Coexistence of thyroid hormone excess and deprivation in different tissues is a distinct characteristic of this syndrome. Tissues expressing transporters other than MCT8, such as liver and kidney, respond to the high circulating T 3 levels resulting in a local hyperthyroid state, whereas tissues depending on MCT8 for thyroid hormone entry into cells, such as the brain, are hypothyroid. 68,72 Two therapeutic options, PTU combined with L-T 468 and a thyromimetic compound, diiodothyropropionic acid (DITPA), which is not dependent on MCT8 for cellular entry, have been used to treat several patients harboring MCT8 gene mutations. 73
How does the kidney regulate thyroid hormone?
The kidney is involved in maintenance of adequate thyroid hormone levels by resorption of filtrated thyroid hormones from primary urine. Free thyroid hormones or hormones bound to plasma transfer proteins are taken up along the tubular epithelium—by direct transport or via endocytosis of plasma proteins. In the absence of Mct8 in mice, renal thyroid hormone levels are increased along with T 3 -dependent gene expression, possibly suggesting that release of thyroid hormones from the cells into the plasma is impaired ( Trajkovic-Arsic, Visser, et al., 2010 ). In contrast, T 3 and T 4 are lost with the urine. Mct10 is coexpressed with Mct8 in kidney tubular epithelium. Combined inactivation of Mct8 and Mct10 exaggerated the thyroid hormone accumulation in the kidney, while paradoxically normalizing plasma T 4 levels ( Muller et al., 2014 ). Lat2 is also expressed in the kidney tubular epithelium. Mice deficient in Lat2 exhibited aminoaciduria, but no changes of plasma thyroid hormone levels ( Braun, Kinne, et al., 2011; Braun, Wirth, et al., 2011 ). These findings suggest that Mct8 and Mct10 both contribute to thyroid hormone efflux from kidney tubular epithelial cells, while Lat2 is more important for amino acid resorption in the same cells.
How do drugs affect thyroid hormone transport?
Some drugs and hormones, such as estrogens and androgens, affect thyroid hormone transport in blood by altering the concentration of binding proteins in serum (see Chapter 76 ). Thyroid hormone transport may also be affected by substances that compete with the binding of thyroid hormone to its carrier proteins (see Table 78-4 ).
What drugs affect T4 and T3?
Several drugs that are widely used in clinical practice (e.g., glucocorticoids, amiodarone, propranolol) inhibit the conversion of T4 to T3 in peripheral tissues. As expected, their most profound effect on thyroid function is a decrease in the serum concentration of T3, usually with a concomitant increase in the rT3 level. An increase in the serum T4 concentration has been observed on occasion. When intrapituitary T4-to-T3 conversion is inhibited, the serum TSH concentration may rise. In the absence of inherent abnormalities in thyroid hormone synthesis or in its secretion, TSH levels should return to normal, and hypothyroidism should not ensue from the chronic administration of compounds that only partially interfere with T 4 monodeiodination. Other mechanisms by which some compounds affect the extrathyroidal metabolism of thyroid hormone involve acceleration of the overall rates of the deiodinative and non-deiodinative routes of hormone disposal. An example of a drug that acts principally through the former mechanism is phenobarbital, 252 and one that acts by way of the latter is diphenylhydantoin. 253 In such circumstances, thyroid hormone concentrations should remain unaltered. Furthermore, it has been anticipated, as well as observed, that hypothyroid patients who receive such drugs require higher doses of exogenous hormone to maintain a eumetabolic state. Some drugs have multiple effects.
What is the second type of JH transport molecule?
A second type of high affinity, high molecular weight JH transport molecule has been discovered, having the characteristics of a hexamerin . The hexamerins, composed of six 70–80 kDa subunits, are widely distributed throughout the phylum Arthropoda and have been found in insects, crustaceans, and certain chelicerates ( Burmester, 2002 ); however, they are not typically employed as hemolymph JH transporters. To date, only species in the order Orthoptera, including L. migratoria ( Koopmanschap and deKort, 1988; Braun and Wyatt, 1996) and Melanoplus sanguinipes ( Ismail and Gillott, 1995 ), are known to exploit hexamerins as JH transport proteins.
How does the kidney help with thyroid hormone?
The kidney is involved in maintenance of adequate thyroid hormone levels by resorption of filtrated thyroid hormones from primary urine. Free thyroid hormones or hormones bound to plasma transfer proteins are taken up along the tubular epithelium—by direct transport or via endocytosis of plasma proteins. In the absence of Mct8 in mice, renal ...
What is the transporter protein for thyroid hormone?
The progress in the field of transmembrane thyroid hormone transport has been truly astonishing. It has been assumed for a long time that transport of iodothyronines across the plasma membrane occurs by passive diffusion, but it has become increasingly clear that cellular uptake and efflux of thyroid hormone is mediated by transporter protein.66 Several specific thyroid hormone transporters have been identified, including monocarboxylate transporter 8 (MCT8), MCT10, and organic anion transporting polypeptide 1C1 (OATP1C1). MCT8 and MCT10 are expressed in multiple tissues where they facilitate transport of T 3, T 4, rT 3, and T 2 across cell membranes; OATP1C1 is expressed predominantly in the brain and transports preferentially T 4, wherein it may mediate the entry of T 4 into the astrocytes. A defect in a single thyroid hormone transporter molecule, MCT8, has been shown to cause a severe developmental neurologic phenotype. 66,62 The Allan-Herndon-Dudley syndrome (AHDS) is an X-linked condition characterized by severe mental retardation, dysarthria, athetoid movements, muscle hypoplasia, and spastic paraplegia associated with an elevated serum T 3. All patients tested with this syndrome have mutations in the MCT8 gene. 63,67 More than 200 individuals belonging to some 100 families of all races and diverse ethnic origins harboring more than 70 different mutations have been identified. 68 Although most mutations resulted in a complete functional inactivation of the MCT8 protein, significant residual activity was observed with a number of MCT8 mutations, some of which associated with a milder clinical phenotype. 69 Surprisingly, MCT8-null mice, despite the presence of marked increased T 3 levels, lack any overt neurologic abnormalities, a rather unexpected finding in light of the severe human phenotype. 70,71 Coexistence of thyroid hormone excess and deprivation in different tissues is a distinct characteristic of this syndrome. Tissues expressing transporters other than MCT8, such as liver and kidney, respond to the high circulating T 3 levels resulting in a local hyperthyroid state, whereas tissues depending on MCT8 for thyroid hormone entry into cells, such as the brain, are hypothyroid. 68,72 Two therapeutic options, PTU combined with L-T 468 and a thyromimetic compound, diiodothyropropionic acid (DITPA), which is not dependent on MCT8 for cellular entry, have been used to treat several patients harboring MCT8 gene mutations. 73
How is thyroid hormone regulated?
Availability of biologically active thyroid hormone is regulated within tissues by the monodeiodinases and the expression of these enzymes could be modified either directly or indirectly by environmental factors ( Figure 10 ). An example of indirect regulation of monodeiodinases by environmental factors is by corticosteroids, which have been shown to increase 5′D activity, with the result that more of the active hormone T 3 is generated. This regulatory relationship suggests that stress and stress hormones can accelerate metamorphosis by upregulating 5′D. Similarly, TR synthesis might be regulated directly or indirectly by environmental factors which would then influence metamorphic timing. Currently, there is little known about what factors, either physiological or environmental, regulate nuclear receptor expression in any species. As for monodeiodinase, evidence suggests that corticosteroids can enhance TH action by upregulating TR expression, and so TR biosynthesis is an additional site where stress and stress hormones may modulate timing of metamorphosis.
How do drugs affect thyroid hormone transport?
Some drugs and hormones, such as estrogens and androgens, affect thyroid hormone transport in blood by altering the concentration of binding proteins in serum (see Chapter 76 ). Thyroid hormone transport may also be affected by substances that compete with the binding of thyroid hormone to its carrier proteins (see Table 78-4 ).
What hormones are involved in inner ear development?
Inner ear development depends on thyroid hormone signaling ( Forrest, 1996 ). Lack of TRβ or Dio2 expression leads to hearing impairment in mice ( Ng et al., 2004 ). Several thyroid hormone transporters are expressed in the inner ear in a cell type-specific and developmentally regulated pattern ( Sharlin, Visser, & Forrest, 2011 ).
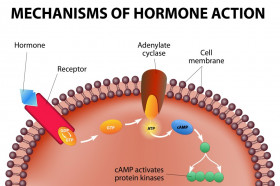
What holds hormones inactive in the systemic circulation?
Transport proteins hold hormones inactive in systemic circulation and create a reservoir within the circulation that facilitates an even distribution of hormones throughout the tissue or organ.
What is the role of transport proteins in the circulatory system?
Therefore, transport proteins can act as a reservoir within the circulatory system and help insure an even distribution of hormones within an organ or tissue.
What is transport protein?
transport protein: A protein that binds with a hormone in systemic circulation that facilitates its efficient transport. The endocrine system is a system of ductless glands that secrete hormones directly into the circulatory system to be carried long distances to other target organs that regulate key body and organ functions. ...
Which system of the body allows the direct targeting of hormones?
Some endocrine glands secrete into a portal system rather than the systemic circulation that allows for the direct targeting of hormones. For example, hormones secreted by the pancreas pass into the hepatic portal vein that transports them directly to the liver. Once within the circulatory system a small proportion of hormones circulate freely, ...
Where are hormones secreted?
Hormones are typically secreted into systemic circulation. However, some are secreted into portal systems that allow for direct hormone targeting. Hormones can exist freely in systemic circulation, but the majority are bound with transport proteins. Transport proteins hold hormones inactive in systemic circulation and create a reservoir within ...
Where do hormones come from?
Hormones are released from the endocrine glands directly into the bloodstream via which they travel to reach the target sites. Hormones are the chemical messenger molecules that are produced in the endocrine glands of the body.
What is target site?
target sites: a cell that is receptive to a secreted hormone.
Do endocrine glands have ducts?
The endocrine glands do not have duct, so they release these hormones directly into the blood. The hormones travel in the blood circulation to reach their target sites (cells, tissues or organs) they can also travel in the lymphatic system when they are destroyed in the liver and removed by the kidneys.
What is the total hormone concentration in plasma?
The total hormone concentration in plasma is the sum of the free and bound hormone. It is important to realize, however, that only the free hormone can diffuse across capillary walls and encounter its target cells. Accordingly, the concentration of the free hormone is what is physiologically important rather than the concentration of the total hormone, most of which is bound. As we shall see, the degree of protein binding also influences the rate of metabolism and the excretion of the hormone.
Do steroid and thyroid hormones exist in plasma?
Even though the steroid and thyroid hormones exist in plasma mainly bound to large protein s, small concentrations of these hormones do exist dissolved in the plasma. The dissolved, or free, hormone is in equilibrium with the bound hormone:
Is peptide soluble in plasma?
Peptide and catecholamine hormones are water-soluble. Therefore, with the exception of a few peptides, these hormones are transported simply dissolved in plasma ( Table 10-2). In contrast, the steroid hormones and the thyroid hormones circulate in the blood largely bound to plasma proteins.
What hormone is released from the hypothalamus?
Cortisol - Corticotropin-releasing hormone from hypothalamus and adrenocorticotropic hormone from anterior pituitary.
What is resistance stage?
Resistance stage - Release of CRH from the hypothalamus causing increase ACTH and cortisol secretion; increased blood levels of amino acid and fatty acid release; formation of glucose from noncarbohydrates.
What are the two types of nervous systems?
1) The endocrine system only. 2) The sympathetic nervous system only. 3) Both the endocrine system and the parasympathetic ner vous system. 4) Both the endocrine system and the sympathetic nervous system. Both the endocrine system and the sympathetic nervous system.
What receptors sense the movement of a baby against and through the cervix during labor?
Baroreceptors in the arteries sense the pressure change and stimulate the brainstem to send signals to dilate blood vessels and counter the effect, decreasing blood pressure. Pressure receptors sense the movement of a baby against and through the cervix during labor.
What is the alarm stage?
Alarm stage - "Fight or flight response", increase blood glucose, glycerol, and fatty acids; increase of heart rate, blood pressure, and breathing rate; dilation of air passages; shift of blood from skin and digestive organs to the skeletal muscles; increase of epinephrine secretion.
How does a syringe affect blood glucose?
2) It promotes protein synthesis in tissues, decreasing the blood concentration of amino acids. 3) It releases fatty acids to to be used as an energy source. 4) It stimulates glucose formation from noncarbohydrates, such as amino acids and gycerol , increasing the blood glucose concentration.
