Here are some aspiration precautions for dysphagia that will help minimize the risk:
- Your healthcare provider may suggest making a change in liquid/food texture, consistency or temperature.
- It is important to take smaller bites and eat slowly.
- Your caregiver should also follow prompting strategies for increased safety.
- It is important to maintain a proper positioning while eating. The best way is to eat while sitting in an upright position with chink tucked slightly at a 90° angle.
- Stay in an upright position even after you have finished you meal. Don't change your position for at least 45 minutes after your meals.
- Keep the head of the bed at 45° if the patient has been diagnosed with GERD as well.
- Never eat or give a patient of aspiration anything to eat a couple of hours before bedtime.
- Take medications that reduce reflux and promote stomach emptying.
- Taking good care of your mouth and teeth.
- Getting dental treatment (such as dentures) when needed.
- Taking medicines as advised.
- Stopping smoking.
- Sitting with good posture when eating and drinking.
- Doing oral exercises as advised by the SLP.
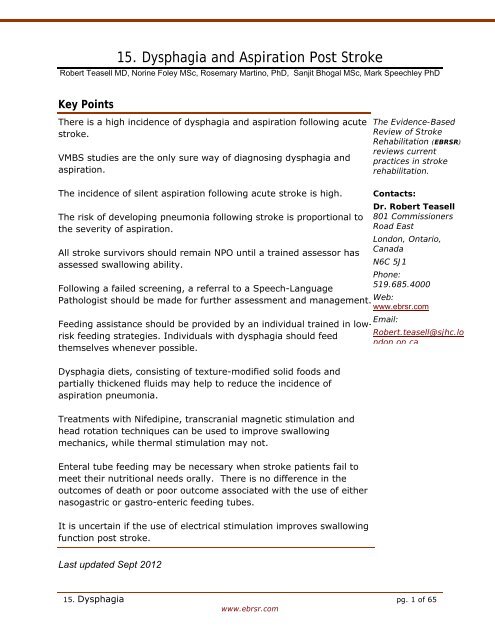
How is aspiration from dysphagia treated?
How is aspiration from dysphagia treated? Your healthcare provider will try to treat the cause of your dysphagia. This may include using medicines. In some cases, surgery may be able to treat the cause of dysphagia.
How do you prevent aspiration in adults?
Follow these guidelines to prevent aspiration when you’re eating and drinking by mouth: Avoid distractions when you’re eating and drinking, such as talking on the phone or watching TV. Cut your food into small, bite-sized pieces. Always chew your food well before swallowing. Eat and drink slowly.
How can I reduce dysphagia after a stroke?
Changing your position while eating (such as eating upright, tilting your head back, or bending your neck forward) As you recover, you may need to use fewer of these methods. Dysphagia after a stroke may improve greatly over time. You may still be at high risk of aspiration even with these methods.
Who is at risk for aspiration from dysphagia?
You may be at risk for aspiration from dysphagia if you have any of these medical conditions: Stroke. Severe dental problems. Conditions that lead to less saliva such as Sjogren syndrome. Mouth sores. Parkinson or other nervous system conditions. Muscular dystrophies. Blockage in the esophagus such as a growth from cancer.

How can patient aspiration be prevented?
Preventing AspirationAvoid distractions when you're eating and drinking, such as talking on the phone or watching TV.Cut your food into small, bite-sized pieces. ... Eat and drink slowly.Sit up straight when eating or drinking, if you can.If you're eating or drinking in bed, use a wedge pillow to lift yourself up.More items...•
What is the most effective way of preventing aspiration?
The primary methods used to prevent aspiration during oral intake in dysphagic stroke patients include texture modification of food/liquids and positional swallowing maneuvers, such as chin-tuck or head rotation (Smithard, 2016).
How can we prevent aspiration pneumonia related to dysphagia?
Interventions to prevent aspiration in older adults with dysphagia living in nursing homes included: more bedside evaluation, modification of dietary, creating an appropriate environment for swallowing, providing appropriate feeding assistance, appropriate posture or maneuver for swallowing, appropriate rehabilitation ...
What should a nurse do to prevent aspiration of feeding contents?
Elevate the head of bed to 30 to 45 degrees while feeding the patient and for 30 to 45 minutes afterward if feeding is intermittent. Turn off the feeding before lowering the head of bed. Patients with continuous feedings should be in an upright position.
How do you drink water with dysphagia?
How to Maintain Proper Nutrition and Hydration on a Dysphagia...Sit upright at 90 degrees when eating and drinking.Do not eat or drink when slouched or lying down.Take small bites of food.Take small sips of fluid.Do not gulp drinks.Eat slowly.Chew foods well before swallowing.More items...•
What side do you lay to prevent aspiration?
Elevated right-side lying (with physician/physical therapist approval). Stomach empties more efficiently due to gravity in this position.
What can be done to prevent aspiration pneumonia?
How can I prevent aspiration pneumonia or reduce my risk of getting aspiration pneumonia?Avoid drinking alcohol to excess and using recreational drugs. ... Stay upright when you are eating.Chew slowly and completely.If you have problems swallowing (things often “go down the wrong pipe”), talk to your healthcare provider.More items...•
What is the primary nursing role to prevent aspiration during enteral feeding?
If you find tube feeding contents in the patient's mouth during oral care, assume the presence of reflux, which increases aspiration risk. To help prevent this problem, keep the head of the bed elevated 30 degrees or higher when possible.
What should the nurse do before feeding a patient who is at risk for aspiration?
What should the nurse do before feeding a patient who is at risk for aspiration? Instruct the patient not to eat and to wait for a nurse to administer the food. Inspect the patient's mouth for pockets of food. Turn the patient on his or her side to prevent aspiration.
How can you prevent aspiration during enteral tube feeding a nurse?
If unable to sit up for a bolus feed or if receiving continuous feeding, the head of the bed should be elevated 30-45 degrees during feeding and for at least 30 minutes after the feed to reduce the risk of aspiration.
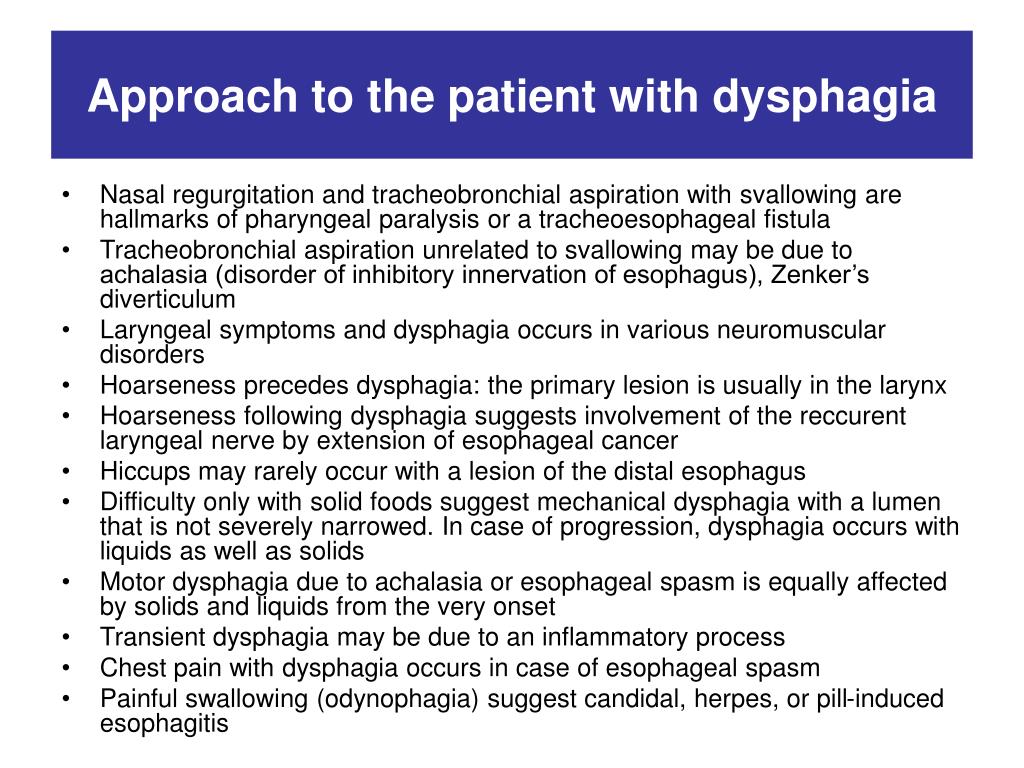
What are the symptoms of aspiration?
Clinical Symptoms of Aspiration: Sudden appearance of respiratory symptoms (such as severe coughing and cyanosis) associated with eating, drinking, or regurgitation of gastric contents. A voice change (such as hoarseness or a gurgling noise) after swallowing. Pocketing of food on one side of the mouth.
Why is aspiration at risk for older adults?
The older adult with one of these conditions is at even greater risk for aspiration because the dysphagia is superimposed on the slowed swallowing rate associated with normal aging. Conditions that suppress the cough reflex ...
How long should you keep your backrest elevated during tube feeding?
For patients with tube feedings, the following considerations are important: Keep the bed’s backrest elevated to at least 30 o during continuous feedings. Keep the bed’s backrest elevated to at least 30 o during intermittent feedings and for at least an hour afterward.
Is thickened liquid better for dysphagia?
Thickened liquids are easier for many patients to control intra-orally, thus preventing premature spillage into the pharynx (Murray et al., 2013). The positional swallowing maneuver prescribed for dysphagic patients varies with the type of swallowing disorder.
Is tube feeding necessary for stroke patients?
Tube feeding is not necessary for all patients who aspirate. However, in the early weeks of acute stroke, nasogastric (NG) feedings are appropriate for patients with severe dysphagia (Moran & O’Mahony, 2015). Percutaneous gastrostomy (PEG) feedings are generally reserved for stroke patients who have persisting dysphagia at two to three weeks ...
Is aspiration pneumonia underdiagnosed?
Aspiration Pneumonia: Older persons with pneumonia often complain of significantly fewer symptoms than their younger counterparts; for this reason, aspiration pneumonia is under-diagnosed in this group . Delirium may be the only manifestation of pneumonia in elderly persons.
Does dysphagia screening replace assessment?
While dysphagia screening by nurses does not replace assessment by other health professionals, it enhances the provision of care to at-risk patients by allowing for early recognition and intervention (Hines et al., 2016; Palli et al., 2017). Assessment may begin at the bedside, using a variety of tools. Most swallow screens use varying volumes of ...
How to know if you have dysphagia?
This may include doing things such as: Changing your diet (such as thickening liquids or not having liquids) Changing your position while eating (such as eating upright, tilting your head back, or bending your neck forward) Not eating in bed.
What are the symptoms of dysphagia?
Aspiration from dysphagia can cause signs and symptoms such as: Feeling that food is sticking in your throat or coming back into your mouth. Pain when swallowing. Trouble starting a swallow. Coughing or wheezing after eating. Coughing while drinking liquids or eating solids. Chest discomfort or heartburn.
Why does food go down when you swallow?
Aspiration from dysphagia is caused when the muscles in the throat don't work normally. This lets food or drink enter the trachea when you swallow. This can happen as food goes down when you swallow. Or it can happen if food comes back up from your stomach.
What is dysphagia in swallowing?
Dysphagia happens when there is a disruption in the swallowing process as food and liquids pass through your mouth, throat, and esophagus. The pharynx is also part of the system that brings air into your lungs.
What is it called when you swallow something and you have trouble swallowing?
This can cause serious health problems, such as pneumonia. Aspiration can happen when you have trouble swallowing normally. This is called dysphagia.
Why do you need to be checked for aspiration?
You will need to be checked for aspiration from dysphagia if you have signs or symptoms. You may also need to be checked if you have had a stroke or other health problem that can cause trouble swallowing. If your healthcare provider thinks you may be aspirating, you may be told to not eat or drink until you are tested.
How many people have dysphagia after a stroke?
About 50% of people who have had a stroke also have dysphagia. About 50% of people with dysphagia have aspiration. About one-third of these people will need treatment for pneumonia at some point.
How to stop aspiration when drinking?
Cut your food into small, bite-sized pieces. Always chew your food well before swallowing. Eat and drink slowly.
How to prevent aspiration when tube feeding?
Follow these guidelines to prevent aspiration if you’re tube feeding: Sit up straight when tube feeding, if you can. If you’re getting your tube feeding in bed, use a wedge pillow to lift yourself up. You can buy a wedge pillow online or at your local surgical supply store.
What is the term for when food goes into your airway instead of your esophagus?
About Aspiration . Aspiration is when food or liquid goes into your airway instead of your esophagus. Your esophagus is the tube that carries food and liquid from your mouth to your stomach. Aspiration can happen when you’re eating, drinking, or tube feeding. It can also happen when you’re vomiting (throwing up) or when you have heartburn.
How to lift yourself up after eating?
Sit up straight when eating or drinking, if you can. If you’re eating or drinking in bed, use a wedge pillow to lift yourself up. You can buy a wedge pillow online or at your local surgical supply store. Stay in an upright position (at least 45 degrees) for at least 1 hour after you eat or drink (see Figure 1).
How do you know if you have aspiration?
Signs of aspiration. Signs of aspiration include: Coughing. Choking. Gagging. Throat clearing. Vomiting. You and your caregiver should watch for these signs before, during, and after you eat, drink, or tube feed. If you have any of these signs, stop eating, drinking, or tube feeding.
Why does food get stuck in the back of my throat?
This is because food or liquid can get stuck in the back of your throat and go into your airway. Aspiration can lead to pneumonia, respiratory infections (infections in your nose , throat, or lungs), and other health problems .