
Is Staphylococcus epidermidis dangerous to humans?
While S. epidermidis is a mild pathogen, opportunistic only in people with lowered resistance, strains of S. aureus are major agents of wound infections, boils, and other human skin infections and are one of the most common causes of food poisoning.
What is the difference between Staphylococcus aureus and epidermidis?
In staphylococcus aureus and S. epidermidis. While S. epidermidis is a mild pathogen, opportunistic only in people with lowered resistance, strains of S. aureus are major agents of wound infections, boils, and other human skin infections and are one of the most common causes of food poisoning. S. aureus….
Is Staphylococcus epidermidis a nosocomial pathogen?
Staphylococcus epidermidis is the most frequently encountered member of the coagulase-negative staphylococci on human epithelial surfaces. It has emerged as an important nosocomial pathogen, especially in infections of indwelling medical devices.
Where is Staphylococcus epidermidis found in human skin?
S. epidermidis is the most familiar resident staphylococcal species on human skin in terms of population size. It is a ubiquitous inhabitant of human skin and mucous membranes that forms a part of the normal flora of skin in humans, predominantly found in the nasal passage and sweaty areas of the body like the armpits and the back.

Where is Staphylococcus epidermidis commonly found?
skinStaphylococcus epidermidis is a permanent member of the normal human microbiota, commonly found on skin, and mucous membranes.
How serious is Staphylococcus epidermidis?
Staph can cause serious infections if it gets into the blood and can lead to sepsis or death. Staph is either methicillin-resistant staph (MRSA) or methicillin-susceptible staph (MSSA). Staph can spread in and between hospitals and other healthcare facilities, and in communities.
Does everyone have Staphylococcus epidermidis?
Staphylococcus epidermidis lives on everyone's skin. The bacteria prefer sweaty places, such as your armpits, but are also found on your back and in your nostrils. Together with other micro-organisms, they produce substances from sweat, bringing about the body odour associated with perspiration.
Is S. epidermidis difficult to treat?
While S. epidermidis infections only rarely develop into life-threatening diseases, their frequency and the fact that they are extremely difficult to treat represent a serious burden for the public health system. The costs related to vascular catheter-related bloodstream infections caused by S.
How do you get rid of Staphylococcus epidermidis?
Antibiotics commonly prescribed to treat staph infections include cefazolin, nafcillin, oxacillin, vancomycin, daptomycin and linezolid. For serious staph infections, vancomycin may be required. This is because so many strains of staph bacteria have become resistant to other traditional antibiotics.
Does Staphylococcus epidermidis need to be treated?
Staph. epidermidis is an important pathogen in immunocompromised patients and patients who develop nosocomial bacteremia; treatment usually consists of antimicrobial therapy and removal of indwelling catheters or devices.
How did I get staph epidermidis?
Staphylococcus epidermidis can cause infections from implantation of medical devices such as cardiac devices, orthopedic devices, and CNS shunt. Up to 20% of patients with cardiac devices can become infected and can show signs of erythema, pain, purulence around the site of the infection, and sepsis.
Is staph epidermidis contagious?
Staph infections are contagious through person-to-person contact. If an individual with staph has a wound that oozes, someone who comes into contact with this liquid can contract the infection. This includes the following transmission methods: close skin contact.
Is staph epidermidis always a contaminant?
Coagulase-negative staphylococci, particularly Staphylococcus epidermidis, have been recognized as an important cause of health care-associated infections. Concurrently, S. epidermidis is a common contaminant in clinical cultures, which poses a diagnostic challenge.
Is Staph epidermidis the same as MRSA?
Also called “Methicillin-Resistant Staphylococcus epidermidis”, inhabit typically on human epidermis (skin). Like the MRSA is a multidrug resistant organism. The MRSE can be distinguished from the MRSA by its biochemical reaction to the Coagulase (enzyme which coagulates blood plasma). The MRSE is a coagulase negative.
Can S. epidermidis cause sepsis?
epidermidis can cause opportunistic infections, which include particularly biofilm-associated infections on indwelling medical devices. These often can disseminate into the bloodstream; and in fact, S. epidermidis is the most frequent cause of nosocomial sepsis.
Are antibiotics still effective against Staphylococcus epidermidis?
S. epidermidis strains usually resist against several types of antibiotic classes such as tetracyclines, aminoglycosides, cephalosporins, fluoroquinolones, penicillins, and macrolides [14,15,16,17]. Nowadays, resistant S. epidermidis has become a serious problem in hospitals [14,15,16].
Is Staphylococcus epidermidis the same as MRSA?
Also called “Methicillin-Resistant Staphylococcus epidermidis”, inhabit typically on human epidermis (skin). Like the MRSA is a multidrug resistant organism. The MRSE can be distinguished from the MRSA by its biochemical reaction to the Coagulase (enzyme which coagulates blood plasma). The MRSE is a coagulase negative.
Why is Staphylococcus epidermidis important?
S. epidermidis, a member of the coagulase-negative Staphylococci, is an important commensal organism of the human skin and mucous membranes; and there is emerging evidence of its benefit for human health in fighting off harmful microorganisms.
Is Staph epidermidis contagious?
Staph infections are contagious through person-to-person contact. If an individual with staph has a wound that oozes, someone who comes into contact with this liquid can contract the infection. This includes the following transmission methods: close skin contact.
Is Staph epidermidis always a contaminant?
Coagulase-negative staphylococci, particularly Staphylococcus epidermidis, have been recognized as an important cause of health care-associated infections. Concurrently, S. epidermidis is a common contaminant in clinical cultures, which poses a diagnostic challenge.
What is the biofilm that protects P. acnes from innate immunity?
Moreover, S. epidermidis biofilm formation by releasing the exopolysaccharide intercellular adhesion (PIA) provides the susceptible anaerobic environment to P. acnes colonisation and protects it from the innate human immunity molecules.
What is the main bacterium that causes acne vulgaris?
Staphylococcus epidermidis enters the sebaceous gland (where Propionibacterium acnes the main bacterium that causes acne vulgaris colonizes) and damages the hair follicles by producing lipolytic enzymes that change the sebum from fraction to dense (thick) form leading to inflammatory effect.
What causes biofilms to grow on plastic devices placed within the body?
Staphylococcus epidermidis stained by safranin. (x1000) As mentioned above, S. epidermidis causes biofilms to grow on plastic devices placed within the body. This occurs most commonly on intravenous catheters and on medical prostheses.
How does S. epidermidis help with acne?
epidermidis can interact to protect the host skin health from pathogens colonisation. But in the case of competition, they use the same carbon source (i.e. glycerol) to produce short chain fatty acids which act as antibacterial agent against each other. Also, S. epidermidis helps in skin homeostasis and reduces the P. acnes pathogenic inflammation by decreasing the TLR2 protein production that induces the skin inflammation.
What is a staphylococcus epidermidis?
Staphylococcus epidermidis, 1000 magnification under bright field microscopy. S. epidermidis is a very hardy microorganism, consisting of nonmo tile, Gram-positive cocci, arranged in grape-like clusters. It forms white, raised, cohesive colonies about 1–2 mm in diameter after overnight incubation, and is not hemolytic on blood agar.
How to detect S. epidermidis?
epidermidis is by using appearance of colonies on selective media, bacterial morphology by light microscopy, catalase and slide coagulase testing. On the Baird-Parker agar with egg yolk supplement, colonies appear small and black.
What is quantitative PCR?
Increasingly, techniques such as quantitative PCR are being employed for the rapid detection and identification of Staphylococcus strains. Normally, sensitivity to desferrioxamine can also be used to distinguish it from most other staphylococci, except in the case of Staphylococcus hominis, which is also sensitive.
How does S. epidermidis detach from the biofilm?
We know that biofilm detachment in S. epidermidis is controlled by the quorum-sensing system agr, as biofilms that are agr -dysfunctional produce thicker biofilms and have an obvious defect in detachment 68, 78. In S. aureus a model has been proposed that involves agr expression at the exposed layers of a biofilm, promoting detachment of cell clusters from the biofilm surface, thereby controlling biofilm expansion 42. Likewise, S. epidermidis agr activity is limited to the biofilm surface 43, indicating a common staphylococcal mechanism of quorum-sensing-controlled biofilm detachment. Two detachment mechanisms have been proposed: enzymatic degradation of biofilm exopolymers and disruption of non-covalent interaction by detergent-like molecules ( Fig. 1 ). With regard to enzymatic degradation of proteinaceous biofilm factors as suggested in S. aureus 44, evidence for such a function of proteases in biofilm detachment in S. epidermidis has not been obtained. However, S. epidermidis produces a series of exoproteases with relatively low substrate specificity that may serve to degrade surface proteins 81 – 83. As for degradation of biofilm exopolysaccharide, staphylococci do not appear to have a dedicated enzyme for PNAG/PIA hydrolysis in contrast to several other bacteria with PNAG/PIA production 84, 85. Alternatively, detergent-like molecules may disrupt non-covalent such as electrostatic and hydrophobic interactions, as for example between the cationic PNAG/PIA and anionic surface polymers, or between hydrophobic parts of the bacterial surface. The short amphipathic phenol-soluble modulins (PSMs) that include the S. epidermidis δ-toxin have been proposed to have such a function 45 ( Fig. 4 ). Both S. epidermidis PSMs and exoproteases are strictly agr -regulated 87, 88, lending support to the idea that they may be candidates for biofilm structuring activity.
How are SDRG and AAP attached?
Proteins such as SdrG and Aap may be attached to the cell surface via sortase-catalyzed covalent anchoring. These proteins harbor a characteristic LPXTG motif at the C-terminus, of which the threonine residue is linked to peptidoglycan. Many autolysins such as AtlE are anchored non-covalently, likely via interaction with teichoic acids. Furthermore, lipoproteins are surface-attached via their fatty acid anchor that penetrates the cytoplasmic membrane. AtlE is a bifunctional adhesin/autolysin that contributres to biofilm formation by its surface hydrophobicity and to host matrix protein binding. SdrG is an example of the Sdr protein family of MSCRAMMs. It stretches the peptidoglycan layer by its SD repeat region and binds fibrinogen via its A region. The B repeats harbor a Ca 2+ binding EF-hand domain. Aap proteins aggregate via Zn 2+ -dependent G5 domains and form fibrils that likely connect cells in the biofilm matrix. G5 domains also bind N-acetylglucosamine and may thus interact with the N-acetylglucosamine exopolysaccharide PNAG/PIA. PNAG/PIA is cationic and likely interacts with negatively charged surface polymers such as teichoic acids (lipoteichoic acids, LTA and wall teichoic acids, WTA) and poly-γ-glutamic acid (PGA).
What is the most common cause of nosocomial infections?
In particular, S. epidermidis represents the most common source of infections on indwelling medical devices.
What is the difference between AIPs and non-self AIPs?
In general, AIPs of self activate, whereas AIPs of non-self (different species or subgroups) inhibit the agr response, unless the groups are closely related (e.g. S. aureus agr types I and IV) 138, 143. The S. epidermidis agr type I is by far the most frequently isolated type from infections.
How do cationic AMPs attach to the cytoplasmic membrane?
Cationic AMPs attach to the negatively charged bacterial surface and membrane by electrostatic interaction, a prerequisite for AMP antimicrobial activity, which is often based on pore formation in the bacterial cytoplasmic membrane. The S. epidermidis ApsS AMP sensor has one short extracellular loop with a high density of negatively charged amino acid residues that interacts with cationic AMPs. Transduction of this signal via ApsS and the accessory, essential ApsX, which has a yet unknown function, triggers expression of key AMP resistance mechanisms. The D-alanylation of teichoic acids, encoded by the products of the dlt operon, and lysylation of phosphatidylglycerol, catalyzed by the MprF enzyme, result in a decreased negative charge of the cell surface and membrane, respectively, leading to decreased attraction, or repulsion, of cationic AMPs. The VraFG ABC transporter also promotes resistance to AMPs and likely functions as an AMP exporter.
How does biofilm form?
Biofilm formation proceeds via initial adhesion and subsequent aggregation into multicellular structures ( Fig. 1 ). Thus, the development of a biofilm requires adhesive forces for the colonization of surfaces and the interaction of cells among each other. Disruptive forces are needed for the formation of fluid-filled channels that are important for nutrient delivery to all biofilm cells and give the mature biofilm its typical three-dimensional structure. Disruptive forces are also involved in the detachment of cell clusters from the biofilm, which limits biofilm expansion and may lead to the dissemination of infection 18.
What is the most frequently isolated ST2?
Most isolates belong to clonal complex (CC) 2 , which comprises the most frequently isolated ST2. Possibly, the successful spread of ST2 may be due to the fact that all ST2 isolates contain IS256 insertion sequences and ica genes 7, two factors found correlated with S. epidermidis invasiveness 13 – 16.
What are the most common causes of burns?
Staphylococcus aureus and Staphylococcus epidermidis are natural pathogens found on skin and therefore are the most common cause of infections in burn populations. These microbes generally produce penicillinases which break the penicillin β-lactam ring and make natural pencillins ineffective against these bacteria.
What is the biofilm produced by Staphylococcus epidermidis?
Staphylococcus epidermidis, normally found on human skin, is capable of biofilm formation when it expresses poly saccharide intracellular adhesin (PIA). Production of PIA is a virulence factor that is associated with S. epidermidis strains found in opportunistic infections.
What is the diameter of a S. epidermidis colony?
Colonies of S. epidermidis are round, raised, shiny, gray, and have complete edges. The diameter is approximately 2.5 mm. They usually do not produce a hemolytic zone. Strains that can produce mucus form translucent sticky colonies.
What is the epidermidis?
S. epidermidis mainly colonizes human skin and is a health concern due to its involvement in hospital-acquired infections. The organisms are frequently detected in saliva and dental plaque and are thought to be associated with periodontitis, acute and chronic pulpitis, pericoronitis, dry socket, and angular stomatitis.
What is the PIA in staph?
Staphylococcus epidermidis, normally found on human skin, is capable of biofilm formation when it expresses polysaccharide intracellular adhesin (PIA). Production of PIA is a virulence factor that is associated with S. epidermidis strains found in opportunistic infections. Phase variation of PIA can occur by transposition of IS 256 into biosynthetic genes for PIA, icaA, or icaC ( Ziebuhr et al., 1999 ). However, unlike IS 492 and IS 1301, insertion does not appear to be targeted to a specific target sequence within these loci, and precise excision occurs at a very low frequency (10 −8 per cell per generation). Thus, the phase variation of PIA in S. epidermidis appears to reflect the plasticity that most insertion elements confer to their resident genomes.
What are the cells of Staphylococcus spherical?
The cells of Staphylococcus are characterized as spherical (0.5–1.5 μm in diameter), gram-positive, aflagellar, and nonmotile cocci organized as single cells, pairs, tetrads, and clusters. However, they tend to form botryoid clusters.
What was the result of the analysis of biochemical reactions in the early 1980s?
In the early 1980s, analysis of biochemical reactions (e.g., mannitol fermentation) and cellular components (e.g., the availability of coagulase) resulted in the division of the Staphylococcus genus into subgroups of pathogenic and nonpathogenic species.
How to identify infection by S. epidermidis
The main type of infection by S. epidermidis it is sepsis, which corresponds to infection in the blood, since this bacteria can easily enter the body, especially when the immune system is compromised, in addition to being associated with endocarditis. Thus, infection by S.
What is S. epidermidis resistant
Often contamination of the sample by S. epidermidis it is misinterpreted by the laboratories and indicated as an infection in the exam result, which makes the doctor indicate the use of antibiotics against "infection". The inappropriate use of antibiotics can favor the formation of resistant bacteria, making treatment difficult.
How the treatment is done
Treatment for infection by Staphylococcus epidermidis it is usually done with the use of antibiotics, however, the antimicrobial of choice varies according to the characteristics of the bacteria, since many have resistance mechanisms. Thus, the use of Vancomycin and Rifampicin, for example, may be recommended by the doctor.
How does S. epidermidis survive?
The mechanisms that S. epidermidis uses to survive during infection are in general of a passive nature, reflecting their possible origin in the commensal life of this bacterium. Most importantly, S. epidermidis excels in forming biofilms, sticky agglomerations that inhibit major host defense mechanisms.
Does S. epidermidis have a cytolytic function?
Moreover, S. epidermidis has the capacity to secrete strongly cytolytic members of the phenol-soluble modulin (PSM) family, but PSMs in S. epidermidis overall appear to participate primarily in biofilm development.
Is Staphylococcus epidermidis a nosocomial pathogen?
Staphylococcus epidermidis is the most frequently encountered member of the coagulase-negative staphylococci on human epithelial surfaces. It has emerged as an important nosocomial pathogen, especially in infections of indwelling medical devices.
Does S. epidermidis control outgrowth?
Conversely, S. epidermidis also has a beneficial role in balancing the microflora on human epithelial surfaces by controlling outgrowth of harmful bacteria such as in particular S. aureus.
Introduction
Staphylococcus epidermidis is a gram-positive, facultative anaerobic bacterium that is present in the skin and mucus membranes of humans and other mammals as part of the microbiota and is usually considered a commensal organism ( Huttenhower et al., 2012; Paharik & Horswill, 2016 ).
Discussion
Nowadays, S. epidermidis is a common HAI etiological agent that causes mainly catheter-related bloodstream infections.
Acknowledgments
The authors would like to thank Ma. Elena Velazquez Meza (National Institute of Public Health) and Maria Román Salgado (Vicente Guerrero Hospital) for providing control strains and clinical isolates, respectively.
What is the habitat of Staphylococcus epidermidis?
Habitat of Staphylococcus epidermidis. S. epidermidis is the predominant coagulase-negative Staphylococcus species found in the material of human origin. Humans are the only natural host for this organism. The physiological habitat of S. epidermidis is the skin and mucous membranes of humans and animals.
What is the most frequently isolated species from human epithelia?
What is Staphylococcus epidermidis? Staphylococcus epidermidis is a Gram-positive bacterium belonging to the genus Staphylococcus and is the most frequently isolated species from human epithelia.
Why is the removal of implant devices the first mode of treatment?
Because most S. epidermidis infections are associated with medical implant devices, the removal of these devices is the first mode of treatment.
What are the biochemical properties of staphylococci?
Besides, other biochemical properties of staphylococci are useful for the differentiation of species, including the production of lactic acid when grown under anaerobic conditions.
What is the classification of a staph?
Classification of species of the genus Staphylococcus is based on various factors like the chemical properties of the cell wall, especially the amino acid composition and sequence of the interpeptide bridges of the peptidoglycan and teichoic acid composition.
What is the cell wall made of?
The cell wall is made up of peptidoglycan and teichoic acid, where the peptidoglycan is the main structural polymer in the wall and plays a vital role in maintaining the spherical shape of the cell. Few wall-associated proteins have also been seen in S. epidermidis, some of which are fibronectin-binding proteins.
What is the habitat of S. epidermidis?
The physiological habitat of S. epidermidis is the skin and mucous membranes of humans and animals. The name ‘epidermidis’ indicates the habitat of the organism. S. epidermidis is the most familiar resident staphylococcal species on human skin in terms of population size.
What are the most common pathogens associated with CRB?
The most frequent pathogens associated with CRB are Staphylococcus epidermidis (37%), S. aureus (13%), Enterococcus (13%), Enterobacter-Klebsiella (11%), Candida spp. (8%), Serratia (5%), and others ( Escherichia coli, Pseudomonas spp.). Gram-negative organisms are especially common in patients with malignancies ( Ropper, 2004 ). According to IDSA guidelines, a blood infection occurring in the presence of a CVC without other apparent source should be suspected CRB ( Mermel et al., 2009 ). Purulence or inflammation at the insertion site is a specific but insensitive sign ( Safdar and Maki, 2002 ). Signs of sepsis, such as hypotension and mental status changes, may also indicate CRB. True confirmation of a catheter source requires the following: (1) the same organism is grown from peripheral blood and the catheter tip culture with growth of > 15 CFUs; or (2) the central blood sample is read as positive ≥ 2 hours earlier than a peripheral blood sample inoculated at the same time; or (3) both catheter and peripheral cultures grow the same organisms and the colony count from the catheter-drawn blood is three to five times greater than that drawn by venepuncture ( Bouza et al., 2007; Mermel et al., 2009 ). Complications by S. aureus bacteremia should be investigated. Echocardiography, preferably by transesophageal echocardiogram, the gold standard, should be performed if there is any suspicions for endocarditis. The best time to look for vegetations is on days 5–7. Other possible complications include osteomyelitis, epidural abscess, and septic arthritis.
What is the biofilm produced by Staphylococcus epidermidis?
Staphylococcus epidermidis, normally found on human skin, is capable of biofilm formation when it expresses polysaccharide intracellular adhesin (PIA). Production of PIA is a virulence factor that is associated with S. epidermidis strains found in opportunistic infections. Phase variation of PIA can occur by transposition ...
What bacteria can be found in tilapia?
Staphylococcus epidermidis is another bacterium that has been reported to infect tilapia. Huang et al. (1999) described the epizootiology and pathogenicity of S. epidermidis in cultured tilapia ( Oreochromis spp.) in Taiwan. Diseased fish showed splenomegaly with diffusion of several white nodules and lesions in the spleen and anterior kidney. When blue tilapia ( O. aureus) were challenged with viable S. epidermidis and its supernatant, apoptosis was predominantly detected in the lymphocytes and macrophages in the spleen and kidney, and occasionally in the brain, liver, gonads, mesentery, stomach, intestine and skeletal muscles ( Huang et al., 2000 ). This particular study indicated that the pathogenicity of S. epidermidis for tilapia is due to the toxicity of the bacterial product, which induces the apoptosis.
Why can't bacteria attach to the outer layer of the skin?
The skin is an inhospitable environment for bacterial colonization and growth with the exception of staphylococcus epidermidis, bacteria cannot attach to the outer layer of skin or stratum corneum because it is composed of dead keratinocytes, keratin, ceramides, free fatty acid, and cholesterol.
What is the best treatment for S. aureus?
Tetracycline, nitrofurantoin and erythromycin were found to be effective against S. aureus. This pathogen was reported to increase the susceptibility of tilapia to infection by S. agalactiae ( Amal et al., 2008 ).
What is the waxy substance in the sebaceous gland?
Sebaceous glands also produce a waxlike substance called sebum , which contains lactic acid and propionic acid produced by Propionibacterium acnes —a commensal organism found in the sebaceous gland. Sebum reduces the skin pH to between 3.0 and 5.0, and this acidic environment inhibits bacterial growth.
Is staph epidermidis a pathogen?
Jules J. Berman, in Taxonomic Guide to Infectious Diseases, 2012. Staphylococcus epidermidis is a commensal that lives on human skin. It is non-pathogenic in most circumstances. Chronically ill patients with indwelling catheters are prone to urinary tract infections caused by Staphylococcus epidermidis. This organism can grow as a biofilm, ...
Overview
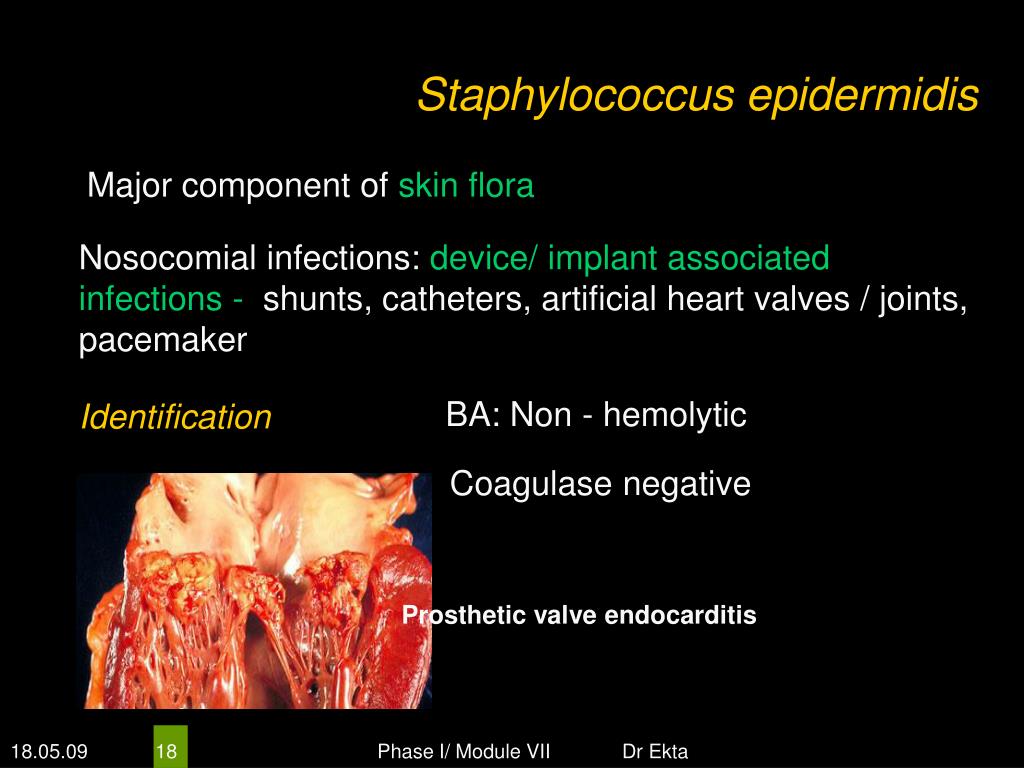
Disease
As mentioned above, S. epidermidis causes biofilms to grow on plastic devices placed within the body. This occurs most commonly on intravenous catheters and on medical prostheses. Infection can also occur in dialysis patients or anyone with an implanted plastic device that may have been contaminated. It also causes endocarditis, most often in patients with defective heart valves. In som…
Etymology
'Staphylococcus' - bunch of grape-like berries, 'epidermidis' - of the epidermis.
Discovery
Friedrich Julius Rosenbach distinguished S. epidermidis from S. aureus in 1884, initially naming S. epidermidis as S. albus. He chose aureus and albus since the bacteria formed yellow and white colonies, respectively.
Cellular morphology and biochemistry
Staphylococcus epidermidis is a very hardy microorganism, consisting of nonmotile, Gram-positive cocci, arranged in grape-like clusters. It forms white, raised, cohesive colonies about 1–2 mm in diameter after overnight incubation, and is not hemolytic on blood agar. It is a catalase-positive, coagulase-negative, facultative anaerobe that can grow by aerobic respiration or by fermentation. So…
Virulence and antibiotic resistance
The ability to form biofilms on plastic devices is a major virulence factor for S. epidermidis. One probable cause is surface proteins that bind blood and extracellular matrix proteins. It produces an extracellular material known as polysaccharide intercellular adhesin (PIA), which is made up of sulfated polysaccharides. It allows other bacteria to bind to the already existing biofilm, creating a multilayer biofilm. Such biofilms decrease the metabolic activity of bacteria within them. This dec…
The role of Staphylococcus epidermidis in acne vulgaris
Staphylococcus epidermidis in the normal skin is nonpathogenic. But in abnormal lesions, it becomes pathogenic, likely in acne vulgaris. Staphylococcus epidermidis enters the sebaceous gland (colonized by Propionibacterium acnes, the main bacterium that causes acne vulgaris) and damages the hair follicles by producing lipolytic enzymes that change the sebum from fraction to dense (thick) form leading to inflammatory effect.
Identification
The normal practice of detecting S. epidermidis is by using appearance of colonies on selective media, bacterial morphology by light microscopy, catalase and slide coagulase testing. Zobell agar is useful for the isolation of Staphylococcus epidermidis from marine organisms. On the Baird-Parker agar with egg yolk supplement, colonies appear small and black. Increasingly, techniques such as quantitative PCR are being employed for the rapid detection and identificatio…