What are the adverse effects of ACE inhibitors?
The most serious, but rare, side effects of ACE inhibitors are:
- Kidney failure
- Allergic reactions
- Pancreatitis
- Liver dysfunction
- A decrease in white blood cells
- Swelling of tissues ( angioedema ).
What are the types of ACE inhibitors?
Types of ACE inhibitors
- captopril, also called Capoten
- cilazapril, also called Zapril, Apo-Cilazapri
- enalapril, also called Enalapril (Ethics), Renitec M
- lisinopril, also called Arrow-Lisinopril, Lisinopril (Ethics)
- perindopril, also called Coversyl, Apo-Perindopril
- quinapril, also called Arrow-Quinapril, Accupril
Do ACE inhibitors slow the heartbeat?
ACE-inhibit-ing drugs, used for about thirty years in the treatment of high blood pressure, slow down ACE activity, result-ing in relaxation of blood vessel walls, lower blood pressure, and a reduced burden on the heart. Benefits. ACE inhibitors are effective in heart failure and after heart attacks, particularly for patients who also have high ...
Is Aricept an ACE inhibitor?
Aricept (donepezil hydrochloride) is a reversible inhibitor of the enzyme acetylcholinesterase, known chemically as (±)-2, 3-dihydro-5, 6-dimethoxy-2-

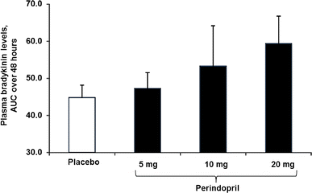
Why do ACE inhibitors increase bradykinin?
Angiotensin-converting enzyme inhibitors are widely used in the treatment of heart failure and hypertension. ACE inhibition not only reduces the generation of angiotensin II but is also associated with increased levels of bradykinin1 because ACE is identical to kininase II, which inactivates bradykinin.
Do ACE inhibitors inhibit bradykinin?
ACE inhibitors prevent the breakdown of a natural chemical in the body called bradykinin. Increased levels of bradykinin, which can cause swelling, may contribute to the development of angioedema.
What happens when bradykinin is increased?
Increased bradykinin levels lead to vasodilation, increased tissue permeability and edema. Degradation of bradykinin is mediated by kininases. ACE, which plays a role in degradation of bradykinin, can be inhibited by ACEIs.
What drugs increases bradykinin?
A class of drugs called angiotensin converting enzyme inhibitors (ACE inhibitors) increase bradykinin levels by inhibiting its degradation, thereby increasing its blood pressure lowering effect. ACE inhibitors are FDA approved for the treatment of hypertension and heart failure.
What is the mechanism of action of ACE inhibitors?
ACE inhibitors prevent an enzyme in the body from producing angiotensin II, a substance that narrows blood vessels. This narrowing can cause high blood pressure and forces the heart to work harder.
What is the role of bradykinin?
The activation of the kinin system-bradykinin is particularly important in blood pressure regulation and in inflammatory reactions, through bradykinin ability to elevate vascular permeability and to cause vasodilatation in some arteries and veins.
How does ACE affect bradykinin?
ACE also breaks down bradykinin (a vasodilator substance). Therefore, ACE inhibitors, by blocking the breakdown of bradykinin, increase bradykinin levels, which can contribute to the vasodilator action of ACE inhibitors.
What stimulates bradykinin release?
Bradykinin produced by the action of kallikrein on kininogen is present both in the lumen of the CD and in the interstitial fluid. Renal bradykinin formation is normally low, and is increased during sodium restriction and water deprivation. Bradykinin is inactivated by kininase II, the same enzyme as ACE.
Do ACE inhibitors inactivate bradykinin?
ACE inactivates bradykinin, and therefore ACE inhibitors can prolong the biologic activities of bradykinin. These membranes have since been chemically modified, thereby reducing this risk.
Does ACE breakdown bradykinin?
Angiotensin-converting enzyme (ACE) is an enzyme that breaks down and inactivates bradykinin. ACE is present in the lungs and the kidneys and also converts angiotensin I to angiotensin II.
Why does ACE inhibitors cause cough?
The means by which ACE inhibitors affect the respiratory system is thought to be through an increase of substance P, which is released from the vagal and glossopharyngeal sensory nerves in the pharynx and upper airways, and is naturally degraded by ACE [7,47]. In this case, this will increase the cough reflex.
How does bradykinin cause dry cough?
Bradykinin induces sensitization of airway sensory nerves via rapidly adapting stretch receptors and C-fiber receptors that releases neurokinin A and substance P. This causes airway smooth muscle to constrict leading to bronchoconstriction and cough.
Why does ACE inhibitors cause angioedema?
ACE inhibitor-induced angioedema is due to the inhibition of bradykinin degradation resulting in elevated plasma bradykinin. As most people on ACEi are able to normalise the bradykinin level by other pathways, a genetic susceptibility is assumed.
Do ARBs increase bradykinin?
An increase in bradykinin levels results in continued prostaglandin E2 synthesis, vasodilation, increased vascular permeability, and increased interstitial fluid. In contrast, the angiotensin II receptor blockers (ARBs) do not increase bradykinin levels.
What causes dry cough with ACE inhibitors?
Taking ACE inhibitors can lead to an increase in a substance called bradykinin. This can irritate the airways, triggering inflammation and coughing.
Why does ACE inhibitor make you cough?
The means by which ACE inhibitors affect the respiratory system is thought to be through an increase of substance P, which is released from the vagal and glossopharyngeal sensory nerves in the pharynx and upper airways, and is naturally degraded by ACE [7,47]. In this case, this will increase the cough reflex.
What is ACE inhibitor?
Angiotensin-converting enzyme (ACE) is an enzyme that breaks down and inactivates bradykinin. ACE is present in the lungs and the kidneys and also converts angiotensin I to angiotensin II. This conversion is a crucial step in blood pressure control as angiotensin II causes vasoconstriction and increases blood pressure and constriction of efferent arterioles in the kidneys. Therefore, inhibition of ACE has clinical application as a mechanism for decreasing blood pressure. ACE inhibitors such as captopril, enalapril, lisinopril, and ramipril all inhibit ACE. They are clinically used to manage patients with hypertension, leading to decreased mortality in patients with heart failure, patients with proteinuria, and patients with diabetic nephropathy. ACE inhibitors can reduce heart remodeling that is caused by chronic hypertension. ACE inhibitors are used in patients with chronic kidney disease such as those with diabetic nephropathy, as they decrease intraglomerular pressure, thereby slowing the thickening of the glomerular basement membrane.
What is the role of bradykinin in inflammation?
Bradykinin plays a prominent role in inflammation. Bradykinin, along with prostaglandins, and histamine, are mediators of vasodilation, in which the arteriolar smooth muscle relaxes, and in turn, increases blood flow. This increased blood flow causes the rubor, or redness, and calor, or warmth, components of the inflammation process. Bradykinin, along with prostaglandin E2 (PGE2), also plays a role in the sensitization of sensory nerve endings, which causes the dolor, or pain, the component of the inflammation process. Thus in the process of inflammation, bradykinin causes an increase in vasodilation, and an increase in permeability, and an increase in pain. [3]
What is Bradykinin in biology?
Bradykinin is a product of kallikrein induced breakdown of high-molecular-weight kininogen (HMWK) in the kinin cascade. HMWK also serves as an inducer of the conversion of factor seven to factor seven A in the intrinsic pathway, or contact activation, of the coagulation cascade. Bradykinin is inactivated by angiotensin-converting enzyme (ACE) in the lungs and kidneys. [2]
What is C1 esterase deficiency?
C1 esterase deficiency is a complement regulatory protein deficiency that causes hereditary angioedema . C1 esterase is a protein inhibitor; it inhibits the complement system to prevent spontaneous activation of the complement system. Without the C1 esterase inhibitor, there is unchecked activation of C1, C2, and C4 complement proteins before other inhibitors can stop the cascade.
Why does kallikrein cause angioedema?
Angioedema is due to the unregulated activation of kallikrein. This activation of kallikrein increases levels of bradykinin because kallikrein activates bradykinin. This excessive bradykinin induces increases permeability, increased vasodilation, and increased pain. [2]
Does inhibition of ACE decrease angiotensin II?
Inhibition of ACE decreases the amount of angiotensin II formed from angiotensin I. This decrease in angiotensin II causes a reduction in the glomerular filtration rate by preventing the constriction of efferent arterioles. This dilation of efferent arterioles causes an increase in renin due to the loss of negative feedback. Inhibition of ACE, however, also inhibits the inactivation of bradykinin. Because bradykinin is a potent vasodilator, the prevention of bradykinin inactivation causes excessive amounts of bradykinin to build-up. This increased bradykinin can cause the side effect of angioedema, which can be seen in some patients taking ACE inhibitors and is the reason for the contraindication of ACE inhibitors in C1 esterase deficiency. [7]
Can angiotensin II blocker be used instead of ACE inhibitors?
Therefore, clinically, angiotensin II receptor blockers (ARB) can be used instead of ACE inhibitors for blood pressure control in hypertensive patients, heart failure, proteinuria, chronic kidney disease, including diabetic nephropathy, or patients with intolerance to ACE inhibitors such as those who have excessive coughing or angioedema.[8] In contrast to ACE inhibitors, angiotensin II receptor blockers, such as losartan, candesartan, and valsartan, selectively block the binding of angiotensin II to the AT1 receptor. Though ultimately, the effects are similar to ACE inhibitors, ARBs do not increase bradykinin as they are not inhibiting ACE. Therefore angioedema is not an adverse effect for patients using ARBs. [9]
What is the relationship between kinin breakdown and the potentiating effect of ACE inhibitors?
Finally, there is a quantitative relationship between kinin breakdown and the potentiating effect of ACE inhibitors. For instance, when stimulation is performed with bradykinin analogues that are partially resistant towards ACE, the potentiation of their actions by ACE inhibitors is impaired to about the same extent as their degradation ( Dendorfer et al., 2001, Dendorfer et al., 2001 ). In addition, blockade of only one of the two active sites of ACE (the so-called N- and C-domain) produces bradykinin potentiation that is only half that during blockade of both domains ( Tom et al., 2001a ). The quantitative relation between bradykinin breakdown and potentiation is further demonstrated by the fact that potentiation can also be provoked by inhibition of other kininases, for instance aminopeptidase P in the rat heart ( Dendorfer et al., 2000 ), and NEP following its overexpression in CHO cells ( Deddish et al., 2002 ). Thus, the phenomenon of kinin potentiation by ACE inhibitors can be mimicked by structurally unrelated inhibitors of other kininases, provided that such kininases are equivalent to ACE in their degradation activities and localizations.
What is the interaction between Ang and bradykinin?
The bradykinin–Ang- (1–7) interaction may involve vasodilatory AT 2 receptors ( Schuijt et al., 2001 ), since the AT 2 receptor antagonist PD123319 partially blocked the Ang- (1–7) + bradykinin-induced relaxation in vitro ( Gorelik et al., 1998 ). Alternatively, Ang- (1–7) may act as an ACE inhibitor ( Deddish et al., 1998, Roks et al., 1999, Tom et al., 2001b ). Ang- (1–7) inhibits the ACE C-domain more potently than the N-domain (IC 50 1–8 μmol/l versus 28–71 μmol/l) ( Deddish et al., 1998 ), and is cleaved to Ang- (1–5) by the N-domain ( Chappell, Pirro, Sykes, & Ferrario, 1998 ). Since ACE is predominantly located on endothelial cells, the ACE inhibitory capacity of Ang- (1–7) not only explains why the relaxant effects of Ang- (1–7) are endothelium-dependent ( Brosnihan, Li, & Ferrario, 1996) and why Ang- (1–7) does not potentiate bradykinin in subjects treated with ACE inhibitors ( Davie & McMurray, 1999 ), but also puts into perspective the existence of a low-affinity (IC 50 2.9 μmol/l) binding site for Ang- (1–7) on bovine aortic endothelial cells ( Tallant, Lu, Weiss, Chappell, & Ferrario, 1997 ). This binding site may in fact be ACE. It must be realized that the physiological concentrations of Ang- (1–7) are several orders of magnitude below the range required to block ACE ( Campbell et al., 1993b ), and that beneficial effects of Ang- (1–7) will therefore only be observed when infused in sufficiently high amounts ( Loot et al., 2002 ).
What is the difference between bradykinin and angiotensin?
Ang II is a vasoconstrictor and growth-promoting substance, whereas bradykinin is a potent vasodilator and growth inhibitor.
How is bradykinin generated?
Bradykinin is generated from kininogen by kallikrein, either directly or via the intermediate kallidin ( Fig. 1 ). In vivo, bradykinin is rapidly degraded (half life <0.5 min) ( Cyr et al., 2001) by kininases, the most important of which are the metallopeptidases ACE and NEP, aminopeptidase P, and the carboxypeptidases M and N ( Dendorfer et al., 1997, Kokkonen et al., 2000 ). In view of its short half life, it is generally assumed that bradykinin, in order to have a local effect, is synthesized at tissue sites. In support of this concept, the various components required to generate bradykinin locally are present in heart and vessel wall ( Nolly et al., 1994, Nolly et al., 1992 ), bradykinin is released from tissue sites into the circulation ( Baumgarten, Linz, Kunkel, Schölkens, & Wiemer, 1993; Duncan et al., 2000 ), and tissue bradykinin levels are higher than those in circulating blood ( Campbell, Kladis, & Duncan, 1993a ).
Do ACE inhibitors affect heart function?
The beneficial effect of ACE inhibitors in hypertension and heart failure may relate, at least in part, to their capacity to interfere with bradykinin metabolism. In addition, recent studies have provided evidence for bradykinin-potentiating effects of ACE inhibitors that are independent of bradykinin hydrolysis, i.e. ACE–bradykinin type 2 (B 2) receptor ‘cross-talk’, resulting in B 2 receptor upregulation and/or more efficient activation of signal transduction pathways, as well as direct activation of bradykinin type 1 receptors by ACE inhibitors. This review critically reviews the current evidence for hydrolysis-independent bradykinin potentiation by ACE inhibitors, evaluating not only the many studies that have been performed with ACE-resistant bradykinin analogues, but also paying attention to angiotensin- (1–7), a metabolite of both angiotensin I and II, that could act as an endogenous ACE inhibitor. The levels of angiotensin- (1–7) are increased during ACE inhibition, and most studies suggest that its hypotensive effects are mediated in a bradykinin-dependent manner.
Is bradykinin a tissue compartment?
The existence of a tissue compartment with highly effective bradyk inin degradation has been demonstrated in the isolated rat heart during bradykinin distribution studies ( Dendorfer, Wolfrum, Wellhoner, Korsman, & Dominiak, 1997 ). Following intracoronary bolus application of 3 H -bradykinin, an early fraction was recovered after intravascular passage in which 72% of 3 H -activity represented intact bradykinin, whereas in a delayed fraction (representing redistribution from a tissue compartment) only 8% of 3 H -activity consisted of intact bradykinin ( Dendorfer et al., 1997 ). The 13-fold reduction of bradykinin availability in the delayed fraction corresponds well with the 19-fold potentiation of bradykinin during combined inhibition of the major kininases in the rat myocardium (ACE and aminopeptidase P) ( Dendorfer et al., 2000 ). Interestingly, the high local efficacy of ACE is not restricted to the inactivation of bradykinin; in vessel segments mounted in organ baths, it also effectively activates Ang I locally, resulting in vascular interstitial Ang II levels that are up to 27-fold higher than the Ang II levels in the organ bath ( Schuijt, de Vries, Saxena, Schalekamp, & Danser, 2002 ). Since interstitial rather than circulating Ang II was found to determine vasoconstriction, these data suggest that ACE and AT 1 receptors, like ACE and B 2 receptors, co-localize in the same compartment. Further evidence for the close anatomical localization of ACE, B 2 receptors and AT 1 receptors comes from a recent observation on AT 1 –B 2 receptor heterodimerization, resulting in enhanced G-protein activation and altered receptor sequestration ( AbdAlla, Lother, & Quitterer, 2000 ).
Does Ang- (1–7) relax arteries?
Pörsti, Bara, Busse, and Hecker (1994) initially reported potent vasodilator effects of Ang- (1–7) in porcine coronary arteries, but were unable to confirm these findings when using a second batch of Ang- (1–7), leading the authors to suggest that the presence of small amounts of Ang- (1–7) with retro-inverted peptide bonds in the first batch may have caused the relaxant effects ( Pörsti, Bara, Busse, & Hecker, 1996 ). Remarkably, vasorelaxation of isolated arteries did occur when Ang- (1–7) was added to the organ bath following the application of bradykinin ( Fernandes et al., 2001; Gorelik, Carbini, & Scicli, 1998; Tom et al., 2001b ). An alternative explanation for the discrepant findings of Pörsti et al. might therefore be that the relaxant effects of Ang- (1–7) in their initial report were due to the fact that in this report endothelial integrity had been verified with bradykinin ( Pörsti, Bara, Busse, & Hecker, 1994 ). Co-infusion of Ang- (1–7) with bradykinin in vivo also potentiated the hypotensive effect of bradykinin ( Abbas et al., 1997, Ueda et al., 2001 ), unless an ACE inhibitor had been added before ( Davie & McMurray, 1999; Fernandes et al., 2001 ).
How do ACE inhibitors work?
General Pharmacology. ACE inhibitors produce vasodilation by inhibiting the formation of angiotensin II. This vasoconstrictor is formed by the proteolytic action of renin (released by the kidneys) acting on circulating angiotensinogen to form angiotensin I. Angiotensin I is then converted to angiotensin II by angiotensin converting enzyme.
What are the effects of ACE inhibitors on the cardiovascular system?
This vasodilation reduces arterial pressure, preload and afterload on the heart.
What is ACE inhibitor?
ACE inhibitors are considered "first-line therapy" in the treatment of stage 1 hypertension. They may also be used in hypertension caused by renal artery stenosis, which causes renin-dependent hypertension owing to the increased release of renin by the kidneys. Reducing angiotensin II formation leads to arterial and venous dilation, which reduces arterial and venous pressures. By reducing the effects of angiotensin II on the kidney, ACE inhibitors cause natriuresis and diuresis, which decreases blood volume and cardiac output, thereby lowering arterial pressure.
How does vasodilation reduce arterial pressure?
Dilate arteries and veins by blocking angiotensin II formation and inhibiting bradykinin metabolism. This vasodilation reduces arterial pressure, preload and afterload on the heart.
Why are ACE inhibitors used in myocardial infarction?
Finally, ACE inhibitors have been shown to be effective in patients following myocardial infarction because they help to reduce deleterious remodeling that occurs post-infarction. ACE inhibitors are often used in conjunction with a diuretic in treating hypertension and heart failure.
What are the side effects of ACE inhibitors?
A common, annoying side effect of ACE inhibitors is a dry cough appearing in about 10% of patients. It appears to be related to the elevation in bradykinin. Hypotension can also be a problem, especially in heart failure patients. Angioedema (life-threatening airway swelling and obstruction; 0.1-0.2% of patients) and hyperkalemia (occurs because aldosterone formation is reduced) are also adverse effects of ACE inhibition. The incidence of angioedema is 2 to 4-times higher in African Americans compared to Caucasians. ACE inhibitors are contraindicated in pregnancy.
What receptors does angiotensin II affect?
This effect of angiotensin II augments sympathetic activity on the heart and blood vessels.
How long does it take for ACE I to cause cough?
ACE-I-induced cough may occur within hours after first intake of the dose or even weeks or months later. ACE-I may sensitize the cough reflex. Owing to this reason, it may increase the severity of chronic cough due to other causes [25]. Coughs due to these medications can decrease within 1 to 4 weeks after discontinuation, but in some cases, this can take up to 3 months [26].
Is ACE I a coughing drug?
ACE-I-induced cough only occurs in susceptible individuals independent of the dose of the drug. Therefore, it is an idiosyncratic reaction. It is a non-immune type B hypersensitivity reaction according to the new terminology and is one of the well-defined side effects of ACE-I [21]. This cough is typically dry with a tickling or scratching feeling in the throat. The incidence of cough associated with the drug has been reported to be between 3.9% and 35% among patients using ACE-I [4–6]. On the other hand, ACE-I is responsible for 0%–3% of chronic cough etiology in prospective studies evaluating patients with chronic cough complaints [22–24].
Does ACE affect the respiratory system?
The means by which ACE inhibitors affect the respiratory system is thought to be through an increase of substance P, which is released from the vagal and glossopharyngeal sensory nerves in the pharynx and upper airways, and is naturally degraded by ACE [7,47]. In this case, this will increase the cough reflex. However, in a meta-analysis of ACE-I-induced cough pharmacokinetics, no correlation between ACE insertion/deletion polymorphism and secondary cough development was found [48].
Does capsaicin increase cough reflex sensitivity?
Experimental stimuli with capsaicin showed increased cough reflex sensitivity in patients with ACE-I-induced cough, which decreased with discontinuation of the drug (25,32). Capsaicin cough reflex sensitivity has also been shown to increase in patients with asthma [60,61].
Can ACE I cause cough?
The result of all these studies suggests that there cannot be only one mechanism responsible for ACE-I-induced cough. Only combinations of two or more of the above mechanisms may result in ACE-I secondary cough.