
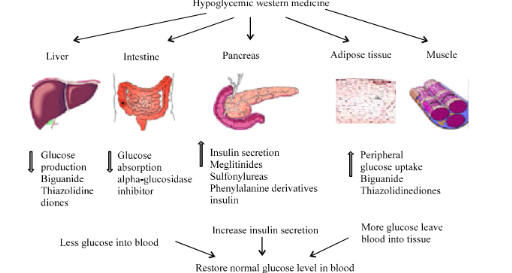
Oral antidiabetic agents work in various ways to reduce blood sugar levels in people with type 2 diabetes; some stimulate insulin secretion by the pancreas, others improve the responsiveness of cells to insulin or prevent glucose production by the liver. Others slow the absorption of glucose after meals.
How to reverse diabetes naturally?
- Avoid ALL refined carbohydrates. ...
- Avoid ALL added sugar. ...
- Avoid ALL sweet drinks. ...
- Do not be scared of good quality, healthy, natural fat – avocados, olives, almonds etc. ...
- Do not waste your energy counting calories. ...
- FEED YOUR GUT BUGS, not just yourself. ...
- Do my 5 minute kitchen workout once a day. ...
What are the best diabetic medicines?
The Best Statins to Lower Non-HDL Cholesterol in Diabetes? A network meta-analysis of 42 clinical trials concludes that rosuvastatin, simvastatin, and atorvastatin are the statins most effective at lowering non-high-density-lipoprotein cholesterol (non-HDL-C) in people with diabetes and at risk for cardiovascular disease.
What is the best treatment for diabetes?
In April 2021, the National Institute for Health and Care Excellence (NICE) in the United Kingdom updated guidelines for adults with diabetes to recommend that non-HDL-C should replace LDL-C as the primary target for reducing the risk for cardiovascular disease with lipid-lowering treatment. Currently, NICE is alone in its recommendation.
What are the most common diabetes medications?
- insulin degludec (Tresiba)
- insulin detemir (Levemir)
- insulin glargine (Lantus)
- insulin glargine (Toujeo)
HOW DO ANTIDIABETIC BIGUANIDES WORK?
Antidiabetic biguanides are a class of drugs used with a proper diet and exercise to control high blood sugar in people with type 2 diabetes mellitus (T2DM). T2DM is a long-term medical condition in which the body does not use insulin normally and, therefore, cannot control the amount of sugar in the blood. Controlling high blood sugar helps in preventing kidney damage, blindness, nerve problems, loss of limbs, and sexual function problems and may also reduce the risk of a heart attack or stroke. Biguanides are a group of oral antihyperglycemic drugs that work by preventing the production of glucose in the liver, improving the body’s sensitivity to insulin, and reducing the amount of sugar absorbed by the intestines. The only available biguanide medication is “ metformin ,” which is commonly used as a first-line treatment for T2DM.
What is the function of AMPK?
In addition, they activate an enzyme (AMPK) that increases the sensitivity to insulin (a natural substance that controls the amount of glucose in the blood produced by the pancreas ), helping cells to respond more effectively to insulin and use more glucose as energy, and thus reducing the concentration of glucose in the bloodstream.
Can you change your medication without consulting your doctor?
Check with your doctor or pharmacist to make sure these drugs do not cause any harm when you take them along with other medicines. Never stop taking your medication and never change your dose or frequency without consulting your doctor.
Can Biguanides be used for diabetes?
Biguanides are not used to treat insulin-dependent or type 1 diabetes (a condition in which the body does not produce insulin and therefore cannot control the amount of sugar in the blood) and diabetic ketoacidosis (increased ketones in the blood or urine ).
How is insulin given?
Insulin Main article: insulin (medication) Insulin is usually given subcutaneously, either by injections or by an insulin pump. Research of other routes of administration is underway. In acute-care settings, insulin may also be given intravenously. In general, there are three types of insulin, Continue reading >>.
What is the best treatment for diabetes mellitus?
The exact treatment algorithms are reviewed in the treatment section of diabetes mellitus. The drug of choice for all type 2 diabetic patients is metformin. This drug has beneficial effects on glucose metabolism and promotes weight loss or at least weight stabilization.
What are the different types of hypoglycemic drugs?
There are seven distinct classes of hypoglycemic agents ( Table 1 ): biguanides, sulfonylureas, meglitinides, thiazolidinediones, -glucosidase inhibitors, incretin mimetics and DPP-4 inhibitors. Aim of this review is to describe the pathophysiological basis of their mechanism of action, to allow physicians to individualize treatment of diabetic people. Table 1. Oral hypoglycemic drugs and their class. Table 1. Oral hypoglycemic drugs and their class. Biguanides are old agents that work by reducing hepatic glucose output and, to a lesser extent, enhancing insulin sensitivity in hepatic and peripheral tissues (ie, antihyperglycemics, hepatic insulin sensitizers). Phenformin was taken off the market in the United States in the 1970s because of its risk of causing lactic acidosis and the associated mortality (rate of approximately 50%). In contrast, metformin has proved effective and safe [ 1 ]. It has been used in Europe for over thirty years, whereas in the United States it has been available since 1995. Metformin should be prescribed to all people with type 2 diabetes, unless contraindicated. Current recommendations of the American Diabetes Association (ADA) and European Association for the Study of Diabetes (EASD) include metformin, diet and exercise as first-line therapy for the treatment of patients with type 2 diabetes, irrespective of the presence of overweight Continue reading >>
What are the different types of glucosidase inhibitors?
Alpha glucosidase inhibitors: Acarbose, Miglitol, Voglibose. New antidiabetic drugs: Exenatide (Byetta), Sitagliptin (Januvia). Combinations: Glibomet (metformin + glibenclamide), Avandamet (rosiglitazone + metformin), Competact (pioglitazone + metformin), Janumet (sitagliptin + metformin). Sulphonylurea drugs used by almost half a century, to treat type 2 diabetes, are indicate in normal weight patients who have type 2 diabetes and in obese patients if they can not tolerate metformin. After ingestion, sulphonylurea drugs are rapidly absorbed in the intestine, pass into the bloodstream, where they bind to specific proteins (albumin, in particular) and reach the liver where they are metabolized into inactive byproducts. Elimination is predominantly renal, with the exception of gliquidone that is eliminated in the bile in proportion of 95%. Mechanism of action. Sulphonylureas are fixing on specific receptors and acts through the potassium channel from the pancreatic and the extra-pancreatic level. At pancreatic level, increase insulin secretion and at the level of pancreatic beta cells, they increase the number of insulin receptors. At extra-pancreatic sulphonylurea drugs decrease hepatic gluconeogenesis (glucose synthesis from non-carbohydrate sources), increased glycolysis and enhances insulin action in skeletal muscle and in adipose tissue. Adverse effects. The main side effect of sulphonylureas is hypoglycaemia (favored by a high dose, kidney failure, liver failure, alcohol consumption, intense physical effort, age over 70 years). Other adverse effects consist of digestive manifestations (nausea, epigastric pain, liver pain) and of haematological manifestations (pancytopenia, autoimmune hemolytic anemia, thrombocytopenia). Sulphonylureas can not be associate with eac Continue reading >>
How does sulphonylurea work?
Mechanism of action. Sulphonylureas are fixing on specific receptors and acts through the potassium channel from the pancreatic and the extra-pancreatic level. At pancreatic level, increase insulin secretion and at the level of pancreatic beta cells, they increase the number of insulin receptors.
What is the difference between diabetes mellitus type 1 and type 2?
Insulin must be used in Type I, which must be injected. Diabetes mellitus type 2 is a disease of insulin resistance by cells. Type 2 diabetes mellitus is the most common type of diabetes.
What is the target A1C level?
If lifestyle modifications (weight loss, dietary modification, and exercise) do not sufficiently reduce A1C levels (target level: ∼ 7% ), pharmacological treatment with antidiabetic drugs should be initiated. These drugs may be classified according to their mechanism of action as insulinotropic or non-insulinotropic.
How do insulin medications lower blood glucose?
These medications lower blood glucose by causing the pancreas to release more insulin.
What is the name of the medication that lowers blood glucose levels?
Acarbose (Precose®,) miglitol (Glyset®) These medications lower blood glucose by delaying the breakdown of carbohydrates and reducing glucose absorption in the small intestine. They also block certain enzymes in order to slow down the digestion of some starches.
What is the name of the drug that helps the body get insulin?
Pioglitozone (Actos®), rosiglitozone (Avandia®) These medications improve the way insulin works in the body by allowing more glucose to enter into muscles, fat, and the liver. Cleveland Clinic is a non-profit academic medical center.
What is the purpose of oral medicine?
Oral diabetes medicines (taken by mouth) help control blood sugar (glucose) levels in people whose bodies still produce some insulin, such as some people with type 2 diabetes.
What are the different types of antidiabetic medications?
The major classes of oral antidiabetic medications include biguanides, sulfonylureas, meglitinide, thiazolidinedione (TZD), dipeptidyl peptidase 4 (DPP-4) inhibi tors, sodium-glucose cotransporter (SGLT2) inhibitors, and α-glucosidase inhibitors. If the HbA1C level rises to 7.5% while on medication or if the initial HbA1C is ≥9%, combination therapy with two oral agents, or with insulin, may be considered (2, 26). Though these medications may be used in all patients irrespective of their body weight, some medications like liraglutide may have distinct advantages in obese patients in comparison to lean diabetics (see below). A schematic of currently approved medications for T2DM is summarized in Table Table1.1. A flowchart for guiding clinical decision making is presented in Figure Figure11.
What are the lifestyle measures for diabetes?
Other lifestyle measures that need to be considered in the treatment plan for patients with diabetes are moderate alcohol consumption (≤1 drink for women, ≤2 drinks/men) and reduction in sodium intake especially in patients with comorbidities such as hypertension , habitual tobacco use , and lacking immunizations (influenza, diphtheria, pertussis, tetanus, pneumococcal, and hepatitis B). Consumption of alcohol, especially in a fasted state, can precipitate life-threatening hypoglycemia and coma and should be explicitly counseled to patients during their visits (23). Moreover, patient education, counseling, and psychosocial support are very important to successfully combat the deleterious effects of diabetes.
What is the HBA1C test?
HbA1C is a chronic marker of hyperglycemia and reflects patient’s blood glucose level over a period of 3–4 months , coinciding with the lifespan of the red blood cells (RBCs). However, in 2009 after its standardization, the International Expert Committee recommended it to be used in diagnosing T2DM but not in T1DM and gestational diabetes (2). HbA1C level is reported in percentages, and a normal level is below 5.7%. The main advantage of the HbA1C test over other blood glucose tests is the convenience it offers to patients; it does not require fasting and can be done at any time of the day. However, this test is more expensive and may not be readily available in certain locations, which may limit its usefulness (14, 15). HbA1C may be inaccurate in conditions such as anemia, hemolysis, and other hemoglobinopathies like sickle cell disease and hemoglobin (Hb) variants like HbC, HbE, and HbD, as well as elevated fetal hemoglobin. Thus, HbA1C assay in people of South Asian, Mediterranean, or African origin merit taking these issues into account (16). In conditions associated with increased RBC breakdown, such as in the advanced trimesters of pregnancy, recent hemorrhage, intravascular hemolysis or transfusion or erythropoietin treatment, only blood glucose estimation should be used to diagnose diabetes. There are limited data supporting the use of A1C in diagnosing T2DM in children and adolescents. Although A1C is not routinely suggested for diagnosis of diabetes in children with cystic fibrosis or symptoms that portend development of acute onset of T1DM, the ADA recommends HbA1C for diagnosis of T2DM in children and adolescents.
How to manage T2DM?
Good glycemic control remains the main foundation of managing T2DM. Such approaches play a vital role in preventing or delaying the onset and progression of diabetic complications. It is important that a patient-centered approach should be used to guide the choice of pharmacological agents. The factors to be considered include efficacy, cost, potential side effects, weight gain, comorbidities, hypoglycemia risk, and patient preferences. Pharmacological treatment of T2DM should be initiated when glycemic control is not achieved or if HbA1C rises to 6.5% after 2–3 months of lifestyle intervention. Not delaying treatment and motivating patients to initiate pharmacotherapy can considerably prevent the risk of the irreversible microvascular complications such as retinopathy and glomerular damage (25). Monotherapy with an oral medication should be started concomitantly with intensive lifestyle management.
What is the condition called when blood glucose is elevated?
Furthermore, a condition called prediabetes or impaired fasting glucose (IFG), in which the fasting blood glucose is raised more than normal but does not reach the threshold to be considered diabetes (110–126 mg/dL), predisposes patients to diabetes, insulin resistance, and higher risk of cardiovascular (CV) and neurological pathologies (2, 3). Type 2 diabetes mellitus (T2DM) can co-occur with other medical conditions, such as gestational diabetes occurring during the second or third trimester of pregnancy or pancreatic disease associated with cystic fibrosis. T2DM may also be iatrogenically induced, e.g., by use of glucocorticoids in the inpatient setting or use of highly active antiretroviral agents like protease inhibitors and nucleoside reverse transcription inhibitors in HIV-positive individuals (4). Chemical diabetes or impaired glucose tolerance (IGT) may also develop with the use of thiazide diuretics, atypical antipsychotic agents, and statins (5, 6).
What are the mechanisms of T2DM?
These include (i) reduced insulin secretion from pancreatic β-cells, (ii) elevated glucagon secretion from pancreatic α cells, (iii) increased production of glucose in liver, (iv) neurotransmitter dysfunction and insulin resistance in the brain, (v) enhanced lipolysis, (vi) increased renal glucose reabsorption, (vii) reduced incretin effect in the small intestine, and (viii) impaired or diminished glucose uptake in peripheral tissues such as skeletal muscle, liver, and adipose tissue. Currently available glucose-lowering therapies target one or more of these key pathways.
What is T2DM?
Type 2 diabetes mellitus (T2DM) is a global pandemic, as evident from the global cartographic picture of diabetes by the International Diabetes Federation (http://www.diabetesatlas.org/). Diabetes mellitus is a chronic, progressive, incompletely understood metabolic condition chiefly characterized by hyperglycemia. Impaired insulin secretion, resistance to tissue actions of insulin, or a combination of both are thought to be the commonest reasons contributing to the pathophysiology of T2DM, a spectrum of disease originally arising from tissue insulin resistance and gradually progressing to a state characterized by complete loss of secretory activity of the beta cells of the pancreas. T2DM is a major contributor to the very large rise in the rate of non-communicable diseases affecting developed as well as developing nations. In this mini review, we endeavor to outline the current management principles, including the spectrum of medications that are currently used for pharmacologic management, for lowering the elevated blood glucose in T2DM.
How does diabetes medicine work?
Each class of medicine works in different ways to lower blood sugar. A drug may work by: Stimulating the pancreas to produce and release more insulin. Inhibiting the production and release of glucose from the liver.
What are the best ways to manage type 2 diabetes?
Healthy lifestyle choices — including diet, exercise and weight control — provide the foundation for managing type 2 diabetes. However, you may need medications to achieve target blood sugar (glucose) levels. Sometimes a single medication is effective. In other cases, a combination of medications works better.
Is diabetes a single treatment?
No single diabetes treatment is best for everyone, and what works for one person may not work for another. Your doctor can determine how a specific medication or multiple medications may fit into your overall diabetes treatment plan and help you understand the advantages and disadvantages of specific diabetes drugs. Oct. 24, 2020.
Is it better to take a single medication or a combination?
Sometimes a single medication is effective. In other cases, a combination of medications works better. The list of medications for type 2 diabetes is long and potentially confusing. Learning about these drugs — how they're taken, what they do and what side effects they may cause — will help you discuss treatment options with your doctor.
Does lowering cholesterol help with diabetes?
Lower cholesterol and have a very modest effect in lowering blood glucose when used in combination with other diabetes medications
What type of diabetes is FDA approved for?
FDA-approved indicationsfor the use of oral hypoglycemic drugs primarily focus on type 2 diabetes mellitus.
What is the best way to manage diabetes mellitus?
The most effective management of diabetes mellitus demands an interprofessional approach involving both lifestyle modifications with diet and exercise and pharmacologic therapies as needed to meet individualized glycemic goals. Healthcare practitioners must encourage patients to combine lifestyle modifications with oral pharmacologic agents for optimal glycemic control, particularly as type 2 diabetes mellitus progresses with continued loss of pancreatic beta-cell function and insulin production. [1][2][3][4][5]
What is the role of sulfonylureas in the pancreas?
Sulfonylureasbind to adenosine triphosphate-sensitive potassium channels (K-ATP channels) in the beta cells of the pancreas; this leads to the inhibition of those channels and alters the resting membrane potential of the cell, causing an influx of calcium and the stimulation of insulin secretion.
How does meglitinide affect insulin secretion?
Meglitinidesexert their effects via different pancreatic beta-cell receptors, but they act similarly to sulfonylureas by regulating adenosine triphosphate-sensitive potassium channels in pancreatic beta cells, thereby causing an increase in insulin secretion.
What is the function of thiazolidinediones?
Thiazolidinediones activate peroxisome proliferator-activated receptor gamma (PPAR-γ), a nuclear receptor, which increases insulin sensitivity and resultant peripheral uptake of glucose and increases the level of adiponectin, a fat tissue-secreted cytokine, that increases not only the number of insulin-sensitive adipocytes but also stimulates fatty acid oxidation.
When is fasting blood sugar measured?
Fasting blood sugar, pre-meal blood sugar, and hemoglobin A1c are measured semi-annually in patients with good blood sugar control and quarterly in those who did not meet treatment goals or have a change in therapy. [6][7][8][9]
Does metformin cause lactic acidosis?
Also, in less than 1% of patients, it causes lactic acidosis, which can be life-threatening, and is precipitated by conditions predisposing to hypoperfusion and hypoxemia, such as severe renal failure (eGFR less than 30 ml/min/1.73 m2).
