- Log in to your account at bcbsm.com. If you haven't registered, follow the instructions to sign up.
- Your latest EOB will be under Claims on the top menu. You can choose to receive only your EOBs online, eliminating the paper statements that get mailed to your home.
How do I get explanation of benefits?
A health care provider will bill your insurance company after you've received your care. Then you'll receive an EOB. Later, you may receive a separate bill for the amount you may owe. This bill will include instructions on who to direct the payment to—either a health care provider or your health insurance company.
Does Blue Shield send EOB?
Additionally, Blue Shield will send an Explanation of Benefits (EOB) to the billing provider as notification that the claim was forwarded to the appropriate capitated provider.
How long does it take to get an explanation of benefits?
The length of time it takes to process a claim depends on these factors: How soon your doctor or hospital submits the claim. Almost 80 percent of claims are received within 30 days from the date of service. In some cases, it can take up to 60 days before your doctor or hospital submits a claim.
How do you know your EOB?
How to read your EOBProvider—The name of the doctor or specialist who provided the service.Service/Procedure—The type of service you received.Total Cost—The amount we pay for the service. ... Not Covered—The amount of the service not covered (this usually only occurs if the service is denied).More items...
Do you always get an EOB?
Explanation of Benefits (EOB) Typically, you should receive an EOB from the insurance company first and then a bill from your provider if any amount is due. If you ever receive a bill before an EOB, wait until your insurance company processes your claim and sends you an EOB before paying your provider.
What is Blue Cross EOB?
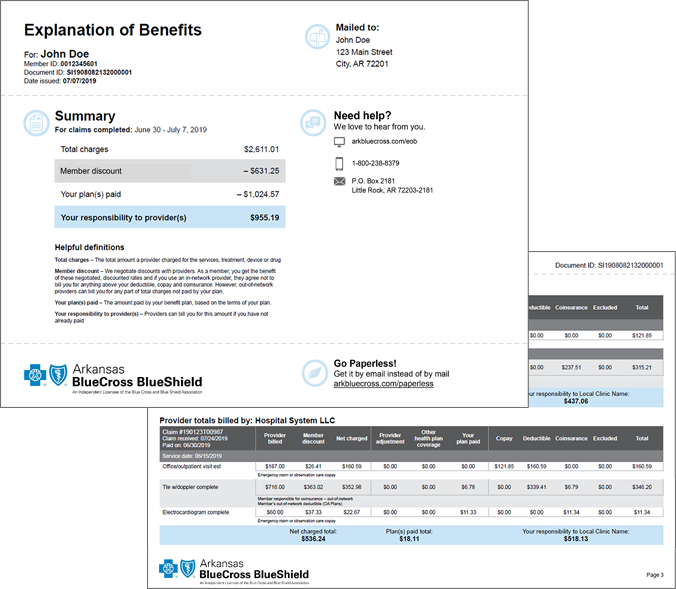
An Explanation of Benefits (EOB) is a notification provided to members when a health care benefits claim is processed by Blue Cross and Blue Shield of Texas (BCBSTX). The EOB shows how the claim was processed. The EOB is not a bill. Your provider may bill you separately.
How often are EOBs sent?
once per monthEOBs are usually mailed once per month. Some plans give you the option of accessing your EOB online. Your EOB is a summary of the services and items you have received and how much you may owe for them.
What is the difference between an EOB and a claim?
What is a claim/EOB? Claim: This is defined as a formal request for your insurance company to provide coverage for your medical expenses. EOB: A document that shows how much the insurance paid, your responsibility and what information may be needed to complete your claim.
How often do you get Explanation of Benefits?
Each month you fill a prescription, your Medicare Prescription Drug Plan mails you an "Explanation of Benefits" (EOB). This notice gives you a summary of your prescription drug claims and costs.
Who receives the EOB?
Usually, the insurer sends the EOB to the primary person on the health plan. If an employer provides the insurance, the employee usually receives the EOB, including EOBs for a spouse and dependents on the plan.
Who receives the Explanation of Benefits EOB report?
Around the time you receive your patient billing statement, you will also receive an explanation of benefits (EOB) from your insurance provider. An explanation of benefits is a document that explains how your insurance processed the claim for the services you received.
What is a copy of EOB?
EOB stands for Explanation of Benefits. This is a document we send you to let you know a claim has been processed. The most important thing for you to remember is an EOB is NOT a bill.
Who will send the EOB?
The insurance companyThe insurance company sends you EOBs to help make clear: Any out-of-pocket medical expenses patient will be responsible for.
Who send EOB to the billing office?
Insurance Payment Posting: All payers either send an EOB (explanation of benefits) or ERA (electronic remittance advice) towards the payment of a claim. The medical billing staff posts these payments immediately into the respective patient accounts, against that particular claim to reconcile them.
How often are EOBs sent?
once per monthEOBs are usually mailed once per month. Some plans give you the option of accessing your EOB online. Your EOB is a summary of the services and items you have received and how much you may owe for them.
What is the difference between a claim and an EOB?
What is a claim/EOB? Claim: This is defined as a formal request for your insurance company to provide coverage for your medical expenses. EOB: A document that shows how much the insurance paid, your responsibility and what information may be needed to complete your claim.
How do I read an EOB?
An EOB from Blue Cross and Blue Shield of Minnesota or Blue Plus includes this information:
Why do I need an EOB?
An EOB gives you a handy snapshot of how you’ve used your benefits and how the claim is being processed. Always compare the EOB to the bill you receive from your provider to make sure they match. If the provider’s bill shows the amount you owe, simply pay the provider. If there’s the amount doesn’t match your EOB, call the number on the back of your member ID card or contact your provider.
Where should I go if I have questions about my EOB?
If you have questions about your EOB, or if you believe there is an error on the EOB, call the number on the back of your member ID card.
What does EOB mean in health insurance?
An EOB is not a bill, but it helps you keep track of some important information: How much your provider charged for services. How much of those charges your health plan covers. The amount your health plan paid.
What does EOB mean in Blue Cross?
After you use your health plan benefits, Blue Cross will send you an Explanation of Benefits (EOB). You may wonder what an EOB is and why you need it. We can help.
How to check if your provider is in your network?
You may pay more or for all of your health care costs if your provider is out of your network or does not have a contract with Blue Cross (this is called a non-participating provider). You can verify if your provider is in your network by calling customer service at the number on the back of your member ID card.
What is a doctor?
The doctor, hospital or other health care professional that provided services
