OPQRST is easy to remember, because these letters follow each other in the alphabet. Find out what exact questions you can ask to get a clearer picture in each category. Onset of the Symptom or Pain The “O” in OPQRST stands for onset. The healthcare professional is trying to determine what brought on the symptom or the pain.
What is the OPQRST mnemonic?
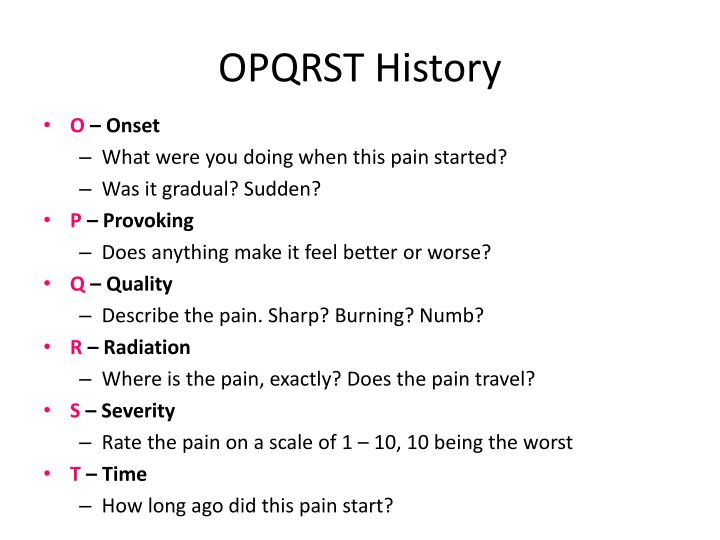
Novice students might use the well-known OPQRST mnemonic (onset, provocation, quality, radiation, severity, and time) to assess the characteristics of the patient's symptom.
What does each letter in OPQRST stand for?
Each letter of OPQRST stands for an essential question in the patient's assessment. O: Onset of the event. P: Provocation/palliation. Q: Quality. R: Region/radiation.
What questions should I ask OPQRST?
OPQRST.O Onset of.event.• What was the patient doing when it started? Were they active, inactive, and or stressed? • Did that specific activity prompt or start the onset of pain? ... P Provocation.and. palliation of. ... • Is the pain better or worse with:• Activity. Does walking, standing, lifting, twisting, reading, etc…More items...
How do you remember a patient's medical assessment?
Memorizing the Medical AssessmentB-SMAC is the first section of the assessment, they are the first thing you do on a scene. ... GACCAT - is your initial assessment. ... OPQRST-I : These are slightly different based upon the type of medical call. ... SAMPLE : This should be familiar!More items...
How do you remember history of present illness?
“OLD CARTS” is a mnemonic device used by providers to guide their interview of a patient while documenting a history of present illness. The letters stand for onset; location; duration; characteristic; alleviating and aggravating factors; radiation or relieving factors; timing; and severity.
When do you use OPQRST and sample?
SAMPLE (History) SAMPLE history is an acronym for remembering what questions are important to ask during your assessment of a patient. ... OPQRST. This acronym is often used in conjunction with SAMPLE as a guide for asking questions regarding a patient's symptoms, specifically pain, during acute illness. ... AEIOU TIPS.
Why is OPQRST important?
OPQRST is a useful mnemonic (memory device) used by EMTs, paramedics, as well as nurses, medical assistants and other allied health professionals, for learning about your patient's pain complaint. It is a conversation starter between you, the investigator, and the patient, your research subject.
What does the mnemonic sample?
“SAMPLE” is a first aid mnemonic acronym used for a person's medical assessment. ... The questions that are asked to the patient include Signs & Symptoms, Allergies, Medications, Past medical history, Last oral intake, and Events leading up to present injury (SAMPLE).
WHAT ARE THE ABCs OF EMT?
First responders are trained to assess three essentials of people in an emergency: airway, breathing and circulation, often referred to as the ABCs.
What are the five steps of patient assessment?
emergency call; determining scene safety, taking BSI precautions, noting the mechanism of injury or patient's nature of illness, determining the number of patients, and deciding what, if any additional resources are needed including Advanced Life Support.
How do you practice patient assessment?
How EMT and paramedic students can practice patient assessmentUse your imagination with simulation and case-based learning. Verbalization and visualization are effective training tools. ... Try some books and apps. ... Standalone patient case study books. ... Live online training. ... Patient assessment study group. ... Read EMS blogs.
What does the mnemonic rows stand for?
What does the mnemonic ROWS stand for? Rule Out Worst-case Scenario.
What does quality mean in OPQRST?
Q. Quality. Description of what the patient is feeling. For example, the pain can be described as dull, sharp, crushing, aching, tearing, throbbing, etc.
What does onset mean in OPQRST?
Onset: “Did your pain start suddenly or gradually get worse and worse?” This is also a chance to ask, “What were you doing when the pain started?” Provokes or Palliates: Instead of asking, “What provokes your pain?” use real, casual words. Try, “What makes your pain better or worse?”
What does sample stand for?
“SAMPLE” is a first aid mnemonic acronym used for a person's medical assessment. ... The questions that are asked to the patient include Signs & Symptoms, Allergies, Medications, Past medical history, Last oral intake, and Events leading up to present injury (SAMPLE).
What does rows stand for in EMS?
What does the mnemonic ROWS stand for? Rule Out Worst-case Scenario.
What does it mean when your chest hurts when you palpate?
A patient that is experiencing chest pain that hurts more when you palpate their chest (also called reproducible pain, if it is similar to the pain they were feeling before palpation) is likely experiencing muscle pain.
What is an OPQRST?
This is an assessment tool for a patient that is experiencing pain, and is information you will need to gather from the patient in certain situations. This assessment is especially useful for patients with possible cardiac problems . This is what OPQRST stands for:
What is the onset of pain?
Onset. The “onset” of the pain is what the patient was doing when the pain started. For example, if the patient is experience chest pain, it is important to know if the patient was active (running, mowing the lawn, chopping wood, etc…) or inactive (sitting on the couch) when the chest pain started.
Why is asking a patient if they have allergies important?
Asking a patient if they have any allergies is very important during the patient assessment. The patient may need medication (s) during their treatment, and they may not be able to answer this question for long if they lose consciousness. The hospital you bring the patient to may not have any medical records for the patient, and will not know what the patient is allergic to if the patient can no longer answer this question when they arrive.
When a patient is having chest pain, should you ask them what they were doing when the pain started?
When a patient is having chest pain, you should ask them what they were doing when the pain started; if they were active at this time (example: running), it is more likely to be cardiac related then if they were inactive (watching t.v.).
What is quality of pain?
The “quality” of a patient’s pain is asking them to describe the pain. Examples of this are:
What is a sample history?
A “SAMPLE” history is a mnemonic used in the medical field, and is a useful tool that is easy to remember for EMTs. The SAMPLE history is usually gathered during the secondary assessment during EMT school, after you have managed the patient’s ABCs (Airway, Breathing, Circulation), after you have managed any immediate life-threats during your primary assessment. Here is what SAMPLE stands for:
Spring 2014 Tour Dates – Everyday EMS Tips
By Greg Elearning designer, writer, podcaster, blogger, presenter and …
EMS Blogs I Read – Everyday EMS Tips
My list of EMS blogs I read has gotten pretty short in the last couple of years. …
What is the O onset?
O → Onset: During this part of the pain assessment the EMT will determine what the patient was doing when the pain began. This is especially important for cardiac patients with angina symptoms.
What is the NREMT medical assessment?
The NREMT medical assessment exam will require candidates to perform the SAMPLE history portion of the patient assessment themselves. When taking a SAMPLE history after completing the OPQRST assessment, the EMT should already have determined the signs and symptoms relating to the history of present illness. In fact, the NREMT medical assessment ...
What is an OPQRST assessment?
The OPQRST pain assessment should be a conversation between the EMT and the patient. You want to ask the patient a lot of questions without it feeling like an interrogation. It’s important to give the patient time to respond to your questions and to actually listen to the patient’s response.
How many points does the NREMT medical assessment give?
In fact, the NREMT medical assessment awards two points for asking clarifying questions about the associated signs and symptoms related to OPQRST. Because of this, the patient assessment following OPQRST becomes the AMPLE mnemonic instead of SAMPLE.
What is OPQRST in EMT?
OPQRST. When the patient has pain as the chief complaint, EMTs can use OPQRST as a memory tool for continuing the patient assessment. The OPQRST pain assessment is usually done after the primary assessment and before the SAMPLE history is completed. During the National Registry of EMT (NREMT) Patient Assessment Medical Exam ...
What is a sample history?
The SAMPLE history is a mnemonic that Emergency Medical Technicians (EMT) use to elicit a patient’s history during the early phases of the patient assessment. It’s common for emergency medical service (EMS) personnel to use mnemonics and acronyms as simple memory cues. These help EMS remember the order of medical assessments ...
Why do EMTs use sample history?
The SAMPLE history allows EMTs to gather information related to the chief complaint in a quick efficient matter which is not only beneficial to the EMT, but also to the hospital staff once the patient is dropped off. The SAMPLE history is used during the patient assessment to identify what happened that caused the patient to call for help.
What is OPQRST in FTO?
OPQRST is one of the main mnemonics for the history of present illness (part of the subjective part of the assessment). What does your FTO suggest as an alternative? What are his problems with OPQRST?
How does OPQRST work?
OPQRST just helps you ask the right questions. When you identify a problem make sure you ask the right questions to work on your differential. You can use what you want to remember, once you start getting a few calls you will not have to think to much about the questions to ask. For example you get abd pain. You can ask where it hurts (have them point to it), the kind of pain, if it hurts upon palp. If it is in a certain quadrant then you can start making your differential. Our service works with a lot of new EMTs we use a check off sheet that helps people ask all the right questions, if you want it you can PM me and I can send it to you.
What are the three acute pathologies?
The only 3 acute pathologies are trauma, toxins and infection. The rest of the modern pathology requires years and decades to create an acute event; if possible to manage or reverse, it takes years. (paraphrase of Veneficus)
Is OPQRST an incomplete assessment?
OPQRST would be a incomplete assessment without SAMPLE.
What is the second description of appendicitis?
The first has a number of possible causes. The second is a classic location/radiation description of appendicitis. The third is a classic description of a perforated appy with peritonitis. The rest of OPQRST, as well as associated symptoms (and the physical exam) flesh out the chief complaint further.
What are some examples of non-traumatic abdominal pain?
For example, if someone with non-traumatic abdominal pain comes in, associated symptoms that you would be interested about include things like nausea, vomiting, diarrhea, skin color changes, etc. Those aren't covered under OPQRST.
Is OPQRST good for SOB?
I find that OPQRST is only really useful when assessing patients who have pain. For SOB it doesn't really work too well.
OPQRST-A
O nset – Onset means the beginning of something. Describe the onset in detail with the 5Ws and 1H: When did the pain start? Where were you? What you were doing when the pain started? How did it start or come on (sudden or gradual)? Why does the pt think the pain came on? Also, ask freq and duration of each episode.
Onset
Onset means the beginning of something. Describe the onset in detail with the 5Ws and 1H.
Palliating & Precipitating factors
Does anything make it better or worse? Does any movement, pressure, or other external factors make the problem worse or better? Does rest relieve the symptoms? Is it post-prandial, exertional, pleuritic, positional?
Quality
For pain, what is the pain like? Is it sharp, dull, burning, crushing, pulsating/throbbing, cramping, tearing, pressure-like? Is it constant or does it come and go?
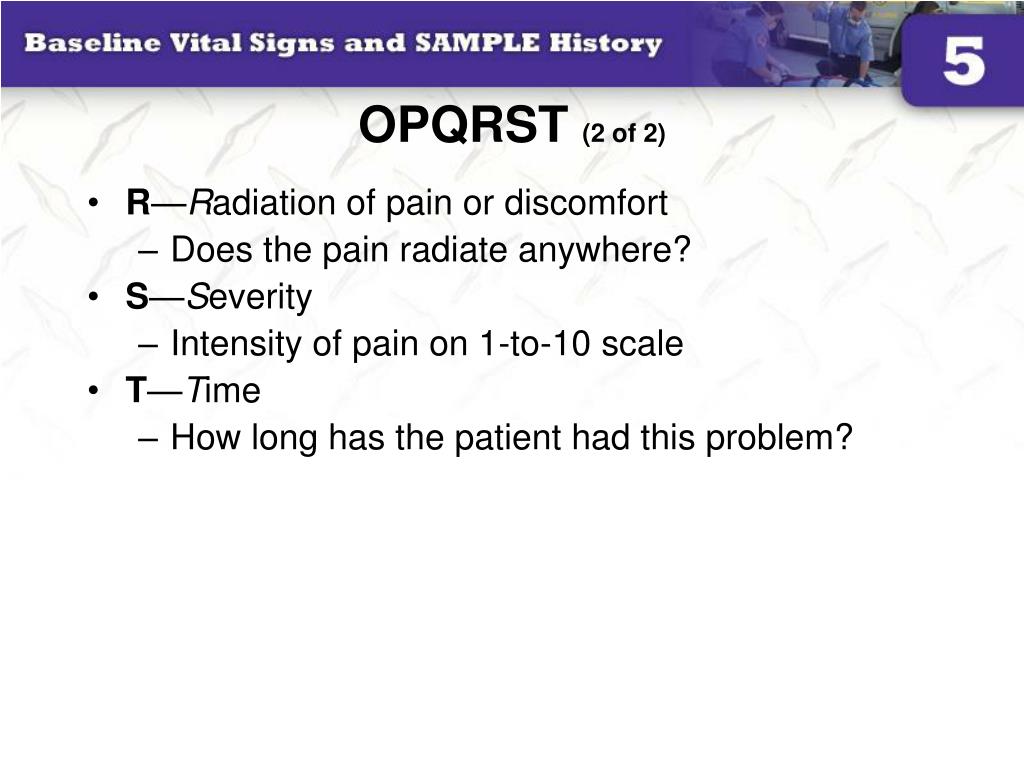
Region and Radiation
What region or location is this pain found? Does it radiate or spread to any other area? You want to also note if it is unilateral or bilateral, proximal or distal, diffuse or localized, radiating vs. non-radiating.
Severity or Quantity
On a scale of 1 to 10, where does it fall? Painful or painless? Can you estimate the amount of phlegm for me? Teaspoon? Tablespoon? Cupful?
Time course
Does the pain follow any pattern? When it starts, how long does it last? How often does it happen? (frequency) Is it continuous or episodic? How has it changed since onset (better, worse, different symptoms)? Has it ever happened before? You want to know whether and how it may have changed since onset, and when the pain stopped if it is no longer currently being felt..