What is mechanical ventilation and how does it work?
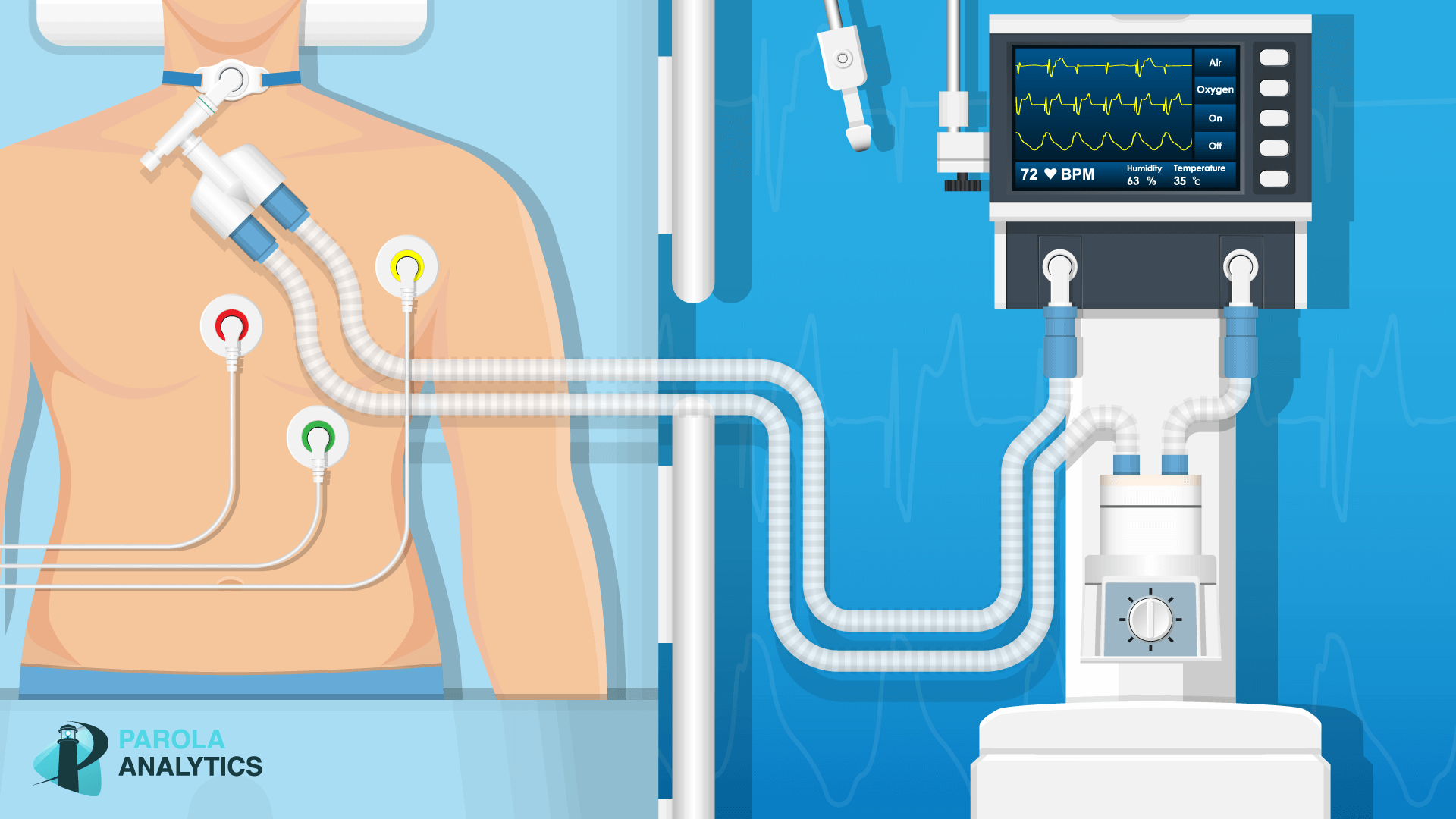
The ventilator can provide a full cycle of breathing during both inspiration and expiration so that the patient does not have to do any work while recovering from the underlying condition. In summary — whenever a patient is unable to ventilate or breathe on their own, this is where Mechanical Ventilation comes into play.
How does a ventilator work in a hospital?
The ventilator delivers oxygen via a tube that is inserted through the patient’s nose or mouth in a procedure known as intubation or that is placed directly into the trachea, or windpipe, in a surgical procedure known as tracheostomy.
How does a ventilator work at UAB?
He teaches students at UAB how to use a ventilator. “It’s a machine that breathes for you,” King said. “Usual breathing uses negative pressure, meaning you open your mouth and air flows in. The machine uses positive pressure to force air into your lungs.
Do nurses need to know about mechanical ventilation?
With that said, nurses do receive basic education of the fundamentals of Mechanical Ventilation. But if a problem were to arise with a ventilator, they must call the Doctor or Respiratory Therapist for help. Modes of Mechanical Ventilation A ventilator mode is a way of describing how the machine assists the patient with inspiration.
How long can you be on a mechanical ventilator?
How long does someone typically stay on a ventilator? Some people may need to be on a ventilator for a few hours, while others may require one, two, or three weeks. If a person needs to be on a ventilator for a longer period of time, a tracheostomy may be required.
Can you talk on a mechanical ventilator?
Talking with a Ventilator in Place You may have a ventilator attached to the trach tube to control your breathing. You can still talk if air can get through your vocal folds. However, your voice will sound different. The ventilator pushes air out of your body in cycles.
What to expect when a loved one is on a ventilator?
If your loved one is on a ventilator, they might be sedated or fall in and out of consciousness. If they are alert, they will be unable to speak due to the breathing tube in their throat. Along with the fluctuation in their consciousness, their comprehension might do the same.
Is a ventilator life support?
How Does a Ventilator Work? A ventilator helps get oxygen into the lungs of the patient and removes carbon dioxide (a waste gas that can be toxic). It is used for life support, but does not treat disease or medical conditions.
Can a sedated person on a ventilator hear you?
This will depend on how much sedation they have been given or any injury to their brain that they may have. If they can hear you, they are unable to speak if they have a breathing tube in their mouth.
Can a person talk while intubated?
Can a person talk or eat when intubated? The endotracheal tube passes through the vocal cords, so you won't be able to speak. Also, you cannot swallow when intubated, so you can't eat or drink.
Can an intubated patient speak?
A PATIENT CAN'T SPEAK when she's endotracheally intubated for mechanical ventilation. Problems communicating can increase her anxiety, impairing both the effectiveness of treatment and her ability to cope with stress.
Is patient on ventilator conscious?
Most often patients are sleepy but conscious while they are on the ventilator—think of when your alarm clock goes off but you aren't yet fully awake. Science has taught us that if we can avoid strong sedation in the ICU, it'll help you heal faster.
What Is A Mechanical Ventilator?
A mechanical ventilator is a machine that helps a patient breathe (ventilate) when he or she is recovering from surgery or critical illness, or can...
Why Do We Use Mechanical Ventilators?
A mechanical ventilator is mainly used to make it easier for very sick people to breathe. Another reason is to help raise the oxygen level for thes...
What Are The Benefits of Mechanical Ventilation?
The main benefits of mechanical ventilation are the following: 1. The patient doesn’t have to work as hard to breathe; 2. The patient's breathing h...
What Are The Risks of Mechanical Ventilation?
The main risk of mechanical ventilation is infection, as the artificial airway may allow germs to enter the lung. Another risk factor is lung damag...
What Procedures Can Help A Patient With An Artificial Airway Connected to A Mechanical Ventilator?
1. Suctioning: This is a procedure in which a catheter (a thin, hollow tube) is inserted into the breathing tube to help remove secretions and wast...
How Long Does The Patient Stay Connected to The Mechanical Ventilator?
The main purpose for using a mechanical ventilator is to allow the patient time to heal. Usually, as soon as a patient can breathe effectively on h...
Who Are The Caregivers Who Take Care of The Patient on A Mechanical Ventilator?
1. Physician: The physician is usually an anesthesiologist, pulmonologist, intensivist, or critical care physician. These doctors have special trai...
What is a ventilator?
A ventilator helps a patient breathe in oxygen and blow out carbon dioxide. Depending on the patient’s condition, a ventilator can either partly support a patient’s breathing or breathe entirely for the patient. Ventilation can be administered invasively or noninvasively.
What ventilation do you need for a patient?
Most patients who rely on this type of ventilation will need: Humidification, because the nose and mouth — where air is normally humidified and warmed — are bypassed. Suctioning, because when tube and inflatable cuff are in place it’s hard to cough; coughing is how we normally clear secretions on our own.
How is noninvasive ventilation administered?
Noninvasive ventilation is administered through a mask over the mouth and / or nose, a simple mouthpiece, or nasal pillows/prongs. 1 A harness or system of straps secures the mask to the patient’s face to keep it in place during ventilation.
Why do you need an inflatable balloon cuff?
The tube may have an inflatable balloon cuff to provide a seal inside the trachea (airway). Invasive breathing assistance interferes with the body’s normal mechanisms for humidifying and clearing the airway.
Can ventilators be used invasively?
Ventilation can be administered invasively or noninvasively. Ventilators can help with or provide breaths that are volume or pressure-controlled.
What is a mechanical ventilator?
A mechanical ventilator is a machine that helps a patient breathe (ventilate) when they are having surgery or cannot breathe on their own due to a critical illness. The patient is connected to the ventilator with a hollow tube (artificial airway) that goes in their mouth and down into their main airway or trachea. They remain on the ventilator until they improve enough to breathe on their own.
What is the medical term for a physician who treats mechanical ventilation?
Physician: The physician is usually an anesthesiologist, pulmonologist, or intensivist (critical care physician). These doctors have special training in the art and science of mechanical ventilation and take care of these patients every day.
How does bronchoscopy work?
Bronchoscopy: In this procedure, the doctor inserts a small light with a camera into the airway of the patient through the breathing tube. This is a very effective tool for checking the airways in the lungs. Sometimes the physician will take samples of mucus or tissue in order to guide the patient's therapy.
Why is mechanical ventilation dangerous?
The main risk of mechanical ventilation is an infection, as the artificial airway (breathing tube) may allow germs to enter the lung. This risk of infection increases the longer mechanical ventilation is needed and is highest around two weeks. Another risk is lung damage caused by either over inflation or repetitive opening and collapsing of the small air sacs Ialveoli) of the lungs. Sometimes, patients are unable to be weaned off of a ventilator and may require prolonged support. When this occurs, the tube is removed from the mouth and changed to a smaller airway in the neck. This is called a tracheostomy. Using a ventilator may prolong the dying process if the patient is considered unlikely to recover.
When do you take a patient off a ventilator?
Usually, as soon as a patient can breathe effectively on their own , they are taken off the mechanical ventilator. The caregivers will perform a series of tests to check the patient's ability to breathe on their own.
What is a respiratory therapist?
Respiratory therapist: The respiratory therapist is trained in the assessment, treatment, and care of patients with respiratory (breathing) diseases and patients with artificial airways who are connected to mechanical ventilators.
Do patients have to work as hard to breathe?
The patient does not have to work as hard to breathe – their respiratory muscles rest.
How does mechanical ventilation work?
Mechanical ventilation works by applying a positive pressure breath and is dependent on the compliance and resistance of the airway system , which is affected by how much pressure must be generated by the ventilator to provide a given tidal volume (TV). The TV is the volume of air entering the lung during inhalation.[1] Compliance and resistance are dynamic and can be affected by the disease state(s) that led to the intubation. Understanding the changes in compliance and resistance will allow you to pick the proper ventilator strategies.
How does mechanical ventilation affect hemodynamics?
When placing a patient on mechanical ventilation, there is a change in their natural negative pressure ventilation to one of positive pressure ventilation; this will affect the heart-lung physiology and can alter the patient's hemodynamic status. The addition of positive pressure ventilation increases interthora cic pressure. The increase in interthoracic pressure will lead to a decrease in right ventricular preload and left ventricular preload and afterload. It will also increase the right ventricular afterload.[6] While these effects could have a minimal change on a healthy person's hemodynamics, they can cause profound alterations in the hemodynamics of a critically ill patient. For example, a patient with acute pulmonary edema will benefit from the reduced preload while someone in septic shock would not.
How to manage ventilator for obstructive patient?
The most important thing to accomplish when managing the ventilator for an obstructive patient is to increase the expiratory phase, allowing for more time to exhale, which will reduce auto-PEEP and dynamic hyperinflation. [1][3][11] It is important to recall that most patients will require deep sedation in order not to over-breathe the ventilator and inspire too often. The tidal volume should be set at 8ml/kg, while the respiratory rate should start at ten breaths per minute.[3] These settings will allow for ample time for a full expiration and hence decreased auto-PEEP, which tends to employ the above described permissive hypercapnia strategy by focussing on lowered tidal volumes and oxygenation over elevated PaCO2. The inspiratory flow rate should be set at 60 L/minute. FI02 should be set at 40% after the initiation of ventilation. As obstructive lung disease is typically a problem with ventilation and not oxygenation, the FIO2 should not need to be increased. Minimal PEEP should be employed, with some studies advocating for a PEEP of zero while some advocate for a small amount of PEEP to help overcome auto-PEEP. The plateau pressure should be less than 30.
How to set up APRV?
Setting up APRV requires adjusting four main variables, P-high, P-low, T-high, and T-low. [17][18] P-high is the continuous pressure set, while P-low is the pressure release part of the cycle. T-high is how long the continuous pressure is set to last, while T-low is the release phase duration. The patient should initially be set on AC/VC immediately post intubation until paralysis wears off. Then, an inspiratory hold should be performed to determine the plateau pressure. This plateau pressure becomes the P-high and should generally be around 27-29cm H2O, though obese patients may require higher pressure. The P-low is generally set to 0. However, there is generally intrinsic PEEP as full exhalation does not occur. The T-high is generally set to 4-6 seconds, while the T-low to .2-.8 seconds in restrictive lung disease and .8-1.5 seconds in obstructive lung disease. To properly set the T-low, you should examine the Flow-Time Waveform on the ventilator. The T-low should be set to approximately 75% of the Peak Expiratory Flow Rate (PEFR). [19][17](See Figure 3) The T-low needs to be continuously readjusted to 75% of the PEFR as lung recruits over time. FI02 should be titrated downwards once the patient is on APRV and comfortable.
What are the stages of mechanical ventilation?
There are four stages of mechanical ventilation. There is the trigger phase, the inspiratory phase, the cycling phase, and the expiratory phase. The trigger phase is the initiation of an inhalation which is triggered by an effort from the patient or by set parameters by the mechanical ventilator. The inhalation of air into the patient defines the inspiratory phase. The cycling phase is the brief moment when inhalation has ceased but before exhalation has begun. The expiratory phase is the passive exhalation of air from the patient.
What is APRV in CPAP?
APRV is a form of continuous positive airway pressure (CPAP) characterized by a timed pressure release while allowing for spontaneous breathing.[16] ( See Figure 1) While previously considered a rescue strategy, APRV has recently gained acceptance as a primary ventilatory mode. Its indications for Acute Lung Injury (ALI)/Acute Respiratory distress syndrome (ARDS), multifocal pneumonia, and severe atelectasis make it a very attractive ventilatory option.
How does APRV work?
APRV functions by providing continuous pressure to keep the lungs open with a timed-release to lower set pressure. [17][18] The continuous pressure phase of APRV transmits pressure to the chest wall, which allows for the recruitment of both proximal and distal alveoli. The prolonged continuous pressure phase with the short release phase avoids the continuous cycles of recruitment-derecruitment in pressure/volume control vent settings.[19] This helps to avoid atelectrauma, barotrauma, and resulting ventilator-induced lung injury.[19] ( See Figure 2) The timed release allows for a passive exhalation and improved clearance of CO2. Since APRV relies upon spontaneous ventilation, it requires less sedation than conventional modalities, thus mitigating adverse events due to sedation. Spontaneous breathing has the benefit of increasing end-expiratory lung volume, decreasing atelectasis, and improves ventilation to dependent lung regions. [19]Spontaneous breathing further improves the hemodynamic profile by decreasing intrathoracic pressure, thus improving preload and cardiac output.
What is mechanical ventilation?
FREMONT, CA: Mechanical ventilation is a procedure that assists a person in breathing while they are unable to do so on their own. A mechanical ventilator helps patients breathe by pushing airflow into their lungs. Mechanical ventilation comprises:
Why do ventilators stop?
The ventilator blows and stops at regular intervals to allow the lungs to absorb oxygen and remove carbon dioxide. Positive-pressure ventilators include: Volume-Controlled: Releases a preset volume of air into the patient's trachea, even though the airway pressure is high.
What is the most effective form of mechanical ventilation?
Positive-Pressure Ventilation. In hospitals today, positive pressure ventilation is the most effective form of mechanical ventilation. Air is forced into the patient's airway by positive-pressure ventilators. The ventilator blows and stops at regular intervals to allow the lungs to absorb oxygen and remove carbon dioxide.
How does a vacuum pump work?
By changing the air pressure inside a chamber that envelops the body up to the neck, the iron lung of the past forces the chest cavity to expand and contract. A vacuum pump produces a negative pressure in the iron lung chamber, allowing the patient's chest to expand and draw air in.
Is the iron lung ventilator negative pressure?
The stomach and heart are both impacted by the negative pressure created in the chamber, which is an issue for the iron lung. The patient's movement is still limited by the iron lung ventilator, making caregiving impossible.
How does a ventilator work?
Here’s how ventilators work: An endotracheal tube goes through the mouth and into the windpipe. When the doctor inserts this tube into your throat, this process is called intubation. You will have this tube in your throat the entire time you are using the ventilator.
What Is a Mechanical Ventilator?
A mechanical ventilator is a bedside machine that assists with breathing. It can help treat respiratory failure, which is when you’re not getting enough oxygen to your blood. Your organs need oxygen to function. As a result, low oxygen levels deprive organs of oxygen and can cause health problems. Respiratory failure can be fatal, and it’s one of the life-threatening complications of COVID-19.
Why are ventilators important?
Mechanical ventilators have played an important role in the treatment of COVID-19 patients. Early in the pandemic, a major concern was making sure that hospitals had enough ventilators to assist the sudden influx in patients. As the pandemic has progressed, many people mistakenly believe that these machines are the same as a simple oxygen mask—but this is far from true.
Is a ventilator the same as a mask?
One of the myths about ventilators is that they are the same as a simple oxygen mask. Supplemental oxygen therapy simply provides concentrated oxygen through a face mask or nasal prongs. The patient can then breathe in the oxygen on their own. Ventilators, on the other hand, require a tube that goes into the throat. They manually force the lungs to inhale and exhale.
Is it bad to be on a ventilator?
To put it simply, being on a ventilator is a big deal. However, the confusion between ventilators and oxygen masks has made some people dismiss the seriousness of ventilators. Some people even shrug off the risk of COVID-19 altogether because they don't see why being intubated is "that bad."
What is a Mechanical Ventilator?
As I mentioned, a Mechanical Ventilator is a machine that aids in a patient’s ability to ventilate. That’s where it gets its name. In other words, it helps the patient take in oxygen and remove carbon dioxide from the lungs.
What is ventilator mode?
A ventilator mode is a way of describing how the machine assists the patient with inspiration. The characteristics of a particular mode essentially control how the ventilator functions.
What is Ventilator-Associated Pneumonia?
Ventilator-Associated Pneumonia (VAP) is a lung infection that develops 48 hours or more after a patient has been intubated and placed on the ventilator.
How Long is a Patient Connected to a Ventilator?
As I mentioned earlier, the primary use of a Mechanical Ventilator is to keep the patient stable long enough to heal.
What are the Risks and Complications of Mechanical Ventilation?
While Mechanical Ventilation has its benefits, it also comes with associated risks and complications as well. Some of which can actually endanger a patient’s life. The following are the most common complications of Mechanical Ventilation:
What is Noninvasive Mechanical Ventilation?
Noninvasive ventilation (NIV) involves the administration of ventilatory support without using any type of invasive artificial airway. Instead, NIV uses a mask that tightly seals to the face in order to provide ventilatory support.
What is the flow setting on a ventilator?
It’s a setting on the ventilator that can be adjusted depending on the patient’s inspiratory needs and demands.
What is a ventilator machine?
Ventilators, often referred to as life support machines, are used in intensive care units for patients who cannot breathe on their own.
How long does a syringe blow air in?
King says the machine typically blows air in for one second, than pauses for roughly three seconds to allow the patient to exhale, then repeats for as long as the machine is in use. And that could be a long time.
Does a ventilator save your life?
King says, while a ventilator might save your life, it is certainly not a pleasant experience. And while a young and healthy person with COVID-19 might not need a ventilator, there are others who will.