
Pressure ulcers are also called bedsores, or pressure sores. They can form when your skin and soft tissue press against a harder surface, such as a chair or bed, for a prolonged time. This pressure reduces blood supply to that area. Lack of blood supply can cause the skin tissue in this area to become damaged or die.
What are the different stages of pressure ulcers?
There are different stages of pressure ulcers, stage 1 being the least serious and stage 4 being the most serious condition. Medical professionals use stages as a way to categorize the wound. Some pressure ulcers are “unstageable” meaning it cannot be determined. Stage 1 The skin is not broken, but is inflamed.
What is the treatment for Stage 1 pressure ulcer?
- Patient should be repositioned with consideration to the individual’s level of activity, mobility and ability to independently reposition. ...
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
- Provide adequate intake of protein and calories.
- Maintain current levels of activity, mobility and range of motion.
Where on the body do pressure ulcers usually form?
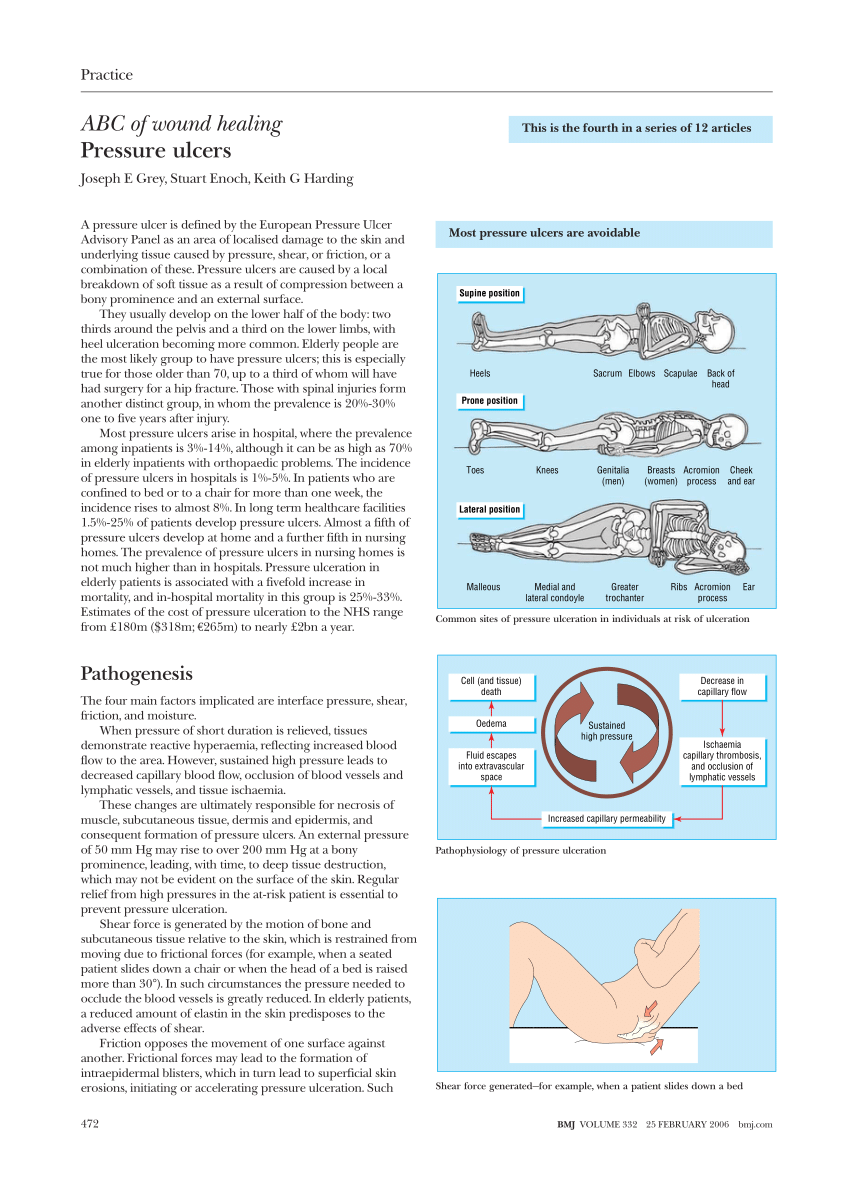
They can happen to anyone, but usually affect people who have to stay in bed or who sit for long periods of time. Pressure ulcers can affect any part of the body. They're most common on bony parts of the body, such as the heels, elbows, hips and base of the spine. They often develop slowly but can form in a few hours.
How to reduce the risk of pressure ulcers?
- The results of the risk and skin assessment.
- The need for any extra pressure relief, for example a high-specification foam mattress or cushion.
- The person’s mobility and ability to change position unaided.
- Any other conditions.
- The person’s own views and wishes, including whether they are able to understand the risks and make an informed decision. ...

What is the first signs that a pressure ulcer is forming?
Typical symptoms include red or purple skin in the affected area, skin that is softer and thinner than the surrounding skin, a break in the skin, and an open sore with a wide base. These tend to occur in bony areas, such as over the tailbone, hips ankles and heels, although they can occur in other areas.
How quickly can pressure ulcers form?
A bedsore develops when blood supply to the skin is cut off for more than 2 to 3 hours. As the skin dies, the bedsore first starts as a red, painful area, which eventually turns purple.
How can pressure ulcers be prevented?
Tips to prevent pressure soreschange position and keep moving as much as possible.stand up to relieve pressure if you can.ask your carer to reposition you regularly if you can't move.change position at least every 2 hours.use special pressure relieving mattresses and cushions.More items...
What are the 4 stages of pressure ulcers?
Stage 1 ulcers have not yet broken through the skin. Stage 2 ulcers have a break in the top two layers of skin. Stage 3 ulcers affect the top two layers of skin, as well as fatty tissue. Stage 4 ulcers are deep wounds that may impact muscle, tendons, ligaments, and bone.
Are pressure sores painful?
Pressure ulcer pain was described as a burning sensation and reported as both constant and transient. Contrary to often-held clinical opinion, the studies reviewed suggest that pain increases with pressure ulcer stage.
Why don't we get bed sores when we sleep?
Healthy individuals usually do not develop bedsores. Most of us reposition our bodies without thinking, even while asleep. Traction – Any sheer force can restrict blood flow to the individual skin. Sheer force traction tends to stretch the skin, like when individuals incline or are propped up in bed.
Who is most at risk of developing pressure sores?
Who's most at risk of getting pressure ulcersbeing over 70 – older people are more likely to have mobility problems and skin that's more easily damaged through dehydration and other factors.being confined to bed with illness or after surgery.inability to move some or all of the body (paralysis)obesity.More items...
How long do pressure sores take to heal?
If you see signs of an infection (such as pus, fever, or redness), tell your doctor. Recovery time: A Stage 2 pressure sore should get better in 3 days to 3 weeks.
What is the most common site for pressure ulcers?
They often form on skin that covers bony areas. The most common sites are the back of the head and ears, the shoulders, the elbows, the lower back and buttocks, the hips, the inner knees, and the heels. Pressure injuries may also form in places where the skin folds over itself.
How do you get rid of pressure sores?
Treatments for pressure ulcers (sores) include regularly changing your position, using special mattresses to reduce or relieve pressure, and dressings to help heal the ulcer. Surgery may sometimes be needed.
What does a pressure sore look like?
It can look like a scrape (abrasion), blister, or a shallow crater in the skin. Sometimes this stage looks like a blister filled with clear fluid. At this stage, some skin may be damaged beyond repair or may die. During stage 3, the sore gets worse and extends into the tissue beneath the skin, forming a small crater.
Can you down stage a pressure ulcer?
Once a pressure ulcer is”staged” it can progress to a higher stage but can NEVER be “BACK-STAGED REVERSE STAGED or DOWN STAGED”. Example: A Stage 3 pressure ulcer can worsen and become a Stage 4 but it NEVER becomes a Stage 2 as it heals.
How long does it take for a Stage 1 pressure ulcer to develop?
Findings from the three models indicate that pressure ulcers in subdermal tissues under bony prominences very likely occur between the first hour and 4 to 6 hours after sustained loading.
What are the three most common early signs of pressure damage?
Early symptoms discoloured patches not turning white when pressed. a patch of skin that feels warm, spongy or hard. pain or itchiness in the affected area.
What does a Stage 1 pressure ulcer look like?
Stage 1 sores are not open wounds. The skin may be painful, but it has no breaks or tears. The skin appears reddened and does not blanch (lose colour briefly when you press your finger on it and then remove your finger).
What do Stage 1 bed sores look like?
Bedsores occur in stages: Stage 1 has unbroken, but pink or ashen (in darker skin) discoloration with perhaps slight itch or tenderness. Stage 2 has red, swollen skin with a blister or open areas. Stage 3 has a crater-like ulcer extending deeper into the skin.
What are the complications of pressure ulcers?
Complications of pressure ulcers, some life-threatening, include: Cellulitis. Cellulitis is an infection of the skin and connected soft tissues. It can cause warmth, redness and swelling of the affected area. People with nerve damage often do not feel pain in the area affected by cellulitis. Bone and joint infections.
How to treat pressure sores on skin?
Protect the skin. Use moisture barrier creams to protect the skin from urine and stool. Change bedding and clothing frequently if needed. Watch for buttons on the clothing and wrinkles in the bedding that irritate the skin. Inspect the skin daily. Look closely at your skin daily for warning signs of a pressure sore.
How to tell if you have a bedsore?
Warning signs of bedsores or pressure ulcers are: Unusual changes in skin color or texture. Swelling. Pus-like draining. An area of skin that feels cooler or warmer to the touch than other areas. Tender areas. Bedsores fall into one of several stages based on their depth, severity and other characteristics.
What is a bedsore?
Close. Bedsore. Bedsore. Bedsores are areas of damaged skin and tissue caused by sustained pressure — often from a bed or wheelchair — that reduces blood circulation to vulnerable areas of the body. Bedsores — also called pressure ulcers and decubitus ulcers — are injuries to skin and underlying tissue resulting from prolonged pressure on the skin.
Where do bedsores occur?
For people who use wheelchairs, bedsores often occur on skin over the following sites: Tailbone or buttocks. Shoulder blades and spine. Backs of arms and legs where they rest against the chair. For people who need to stay in bed, bedsores may happen on: The back or sides of the head. The shoulder blades.
Where does pressure occur in the body?
For people with limited mobility, this kind of pressure tends to happen in areas that aren't well padded with muscle or fat and that lie over a bone, such as the spine, tailbone, shoulder blades, hips, heels and elbows.
Can pressure sores cause bone and joint infections?
Bone and joint infections. An infection from a pressure sore can burrow into joints and bones. Joint infections (septic arthritis) can damage cartilage and tissue. Bone infections (osteomyelitis) can reduce the function of joints and limbs.
What are the stages of a pressure ulcer?
hips. ankles. heels. If you develop a pressure ulcer, you may notice that they form in a series of four stages. These stages are based on how deep the sore is. In some severe cases, there are two kinds of pressure ulcers that cannot fit into one of the four stages: suspected deep pressure injury. unstageable sores.
How to treat a swollen ulcer?
The first step to treating an ulcer in this stage is to remove pressure from the area. Any added or excess pressure can cause the ulcer to break through the skin surface. If you are lying down, adjust your position or use pillows and blankets as extra padding.
What does it mean when a stage 2 ulcer is swollen?
A stage 2 ulcer may appear as a serum-filled (clear to yellowish fluid) blister that may or may not have burst. The surrounding areas of the skin may be swollen, sore, or red. This indicates some tissue death or damage.
Why is it hard to diagnose an unstageable ulcer?
Unstageable pressure ulcers are also hard to diagnose because the bottom of the sore is covered by slough or eschar. Your doctor can only determine how deep the wound is after clearing it out. The ulcer may be yellow, green, brown, or black from slough or eschar.
What does it mean when your sores are black?
Your skin may turn black, exhibit common signs of infection, and you may notice a dark, hard substance known as eschar (hardened dead wound tissue) in the sore. Share on Pinterest.
How long does it take for a skin ulcer to heal?
These foods help with skin health. If treated early, developing ulcers in stage one can heal in about three days.
How long does it take for a stage 4 pressure ulcer to heal?
Your doctor will likely recommend surgery. Recovery for this ulcer can take anywhere from three months to two years to completely heal.
How does pressure ulcers develop?
Pressure ulcers can develop when a large amount of pressure is applied to an area of skin over a short period. They can also occur when less pressure is applied over a longer period. The tissue distortion occurs either because the soft tissues are compressed and/or sheared between the skeleton and a support, such as a bed or chair when the person is sitting or lying, or because something is pressing into the body, such as a shoe, a prosthesis, a surgical appliance or clothing elastic. Blood vessels within the distorted tissue are compressed, angulated or stretched out of their usual shape and blood is unable to pass through them.[4] The tissues supplied by these blood vessels become ischaemic. Besides occluding the blood flow, tissue distortion also obstructs lymphatic flow, which in turn leads to accumulation of metabolic waste products, proteins and enzymes in the affected tissue. This too can compound the tissue damage.[5,6]
Why do ulcers have oxygen?
Oxygen is required for all stages of wound healing thus any condition that is associated with a low tissue oxygen tension is a major cause of pressure ulcers. These include: Heart failure, atrial fibrillation, myocardial infarction, and chronic obstructive pulmonary disease.
What is the most common grading system for pressure ulcers?
Healthcare professionals use several grading systems to describe the severity of pressure ulcers; most common is the EPUAP grading system. Pressure sores are categorised into four stages [Table 2] corresponding to the depth of damage.[22,23,24] It must however be emphasised that when an eschar is present, accurate staging is not possible.
How do living tissues change over time?
As the living tissues are not static, the way they are distorted change over time. When constant pressure is maintained, soft tissues mould themselves to accommodate the external shape. This is known as tissue creep.[10] This may reduce the external pressures but may also exaggerate internal distortions of soft tissues that further reduce the vascular supply of already compromised area due to vascular kinking. This distortion of internal conjugation of soft tissues are significantly high in paraplegic patients[11] and particularly in these susceptible patients, If ischaemia persists for 1-2 h, necrosis takes place and pressure ulcers can occur within 1-2 h.[12] Due to prolonged and constant pressure, the chances of atrophy of the skin with thinning of this protective barrier, making the skin more susceptible to minor compression.
What age group is most likely to have pressure ulcers?
Age is also a factor that the majority (approximately two-third) of pressure ulcers occur in old age people (60-80 years of age).[7] .
What is the most accurate description of a pressure ulcer?
Pressure ulcers are a type of injury that breaks down the skin and underlying tissue when an area of skin is placed under constant pressure for certain period causing tissue ischaemia, cessation of nutrition and oxygen supply to the tissues and eventually tissue necrosis. Constant pressure resulting in ‘distortion or deformation damage’ is probably the most accurate description of a pressure ulcer.[1] There is a localised, acute ischaemic damage to any tissue caused by the application of external force (either shear, compression or a combination of the two).
How do contractures and spasticity contribute to joint flexion?
Contractures and spasticity can contribute by repeatedly exposing tissues to pressure through flexion of a joint.
What is a pressure ulcer?
Pressure Ulcers (Pressure Injuries) Pressure ulcers occur when your skin is damaged due to pressure. Other terms include pressure injuries, pressure sores, bed sores, or decubitus ulcers. There are three primary risk factors to developing a pressure ulcer: immobility, increased pressure on a section of skin, and an interruption ...
How does pressure sore develop?
How Pressure Sores Develop. Blood flows through the body’s tissues, including the skin. If you press your finger down on a spot your arm and then quickly remove your finger, you will see that the skin changes color for a second or so in that spot because you stopped the blood flow.
How to prevent pressure sores?
The only way to prevent pressure sores is to ensure there is no or little pressure on specific parts of the body for prolonged periods. This means if someone is confined to bed, they must be turned and positioned regularly if they cannot do it themselves. People who use wheelchairs for mobility should shift their position at least every 15 minutes. Special seating cushions can also help alleviate pressure.
What causes pressure to be added to a bed?
Watch for objects that could cause added pressure. Wrinkles in sheets or clothing can be irritating, as can tiny things like crumbs or items you could easily drop on the seat or in the bed without noticing.
Where is the pressure sore located?
Any pressure sore where the skin has broken is susceptible to infection, but the risk is higher when the sore is located around the coccyx (tailbone) or buttocks, particularly if the patient is incontinent, unable to control bowel or bladder.
Can you get pressure ulcers from lying in bed?
One or more ulcers can develop if you lie in bed and don’t change positions often enough or if you sit still for extended periods without moving. A pressure ulcer can also develop in other ways. For example, one could form under your arms if you use crutches incorrectly, on the skin where your leg rests on a prosthetic, or behind your ear if your glasses or oxygen tubing are too tight.
Can you move in a chair with a pressure ulcer?
This is how a pressure ulcer forms. Someone who cannot move about in bed or on a chair is at highest risk of developing pressure ulcers wherever their body is in contact with the bed or chair, no matter how soft the mattress or cushioning may be.
What is Pressure Ulcer?
Also known as Bedsore , Pressure Sore , or Decubitus Ulcer , a Pressure Ulcer is an area of damaged skin & underlying tissue caused by prolonged pressure on the skin that cuts-off blood flow to the parts of the body and results in injuries to the skin and tissues. A Pressure Ulcer is an open wound on the skin that often occurs on the skin covering bony areas but the most common places for a Pressure Ulcer are: hips, back, ankles, and buttocks.
How to prevent pressure ulcers?
An individual can prevent the development of pressure ulcers by frequently repositioning and avoiding stress on the skin. Apart from this, taking good care of skin, good nutrition, and fluid intake, avoiding smoking & stress and daily exercises can help a lot.
How does negative pressure wound therapy work?
Negative pressure wound therapy. The healing process depends on the stage of your ulcer. The sooner it is diagnosed, the sooner treatment can be started and recovery can also be quick. Wound Care Surgeons may suggest you make some small lifestyle changes in your diet while later stages require more aggressive treatment.
Why is it important to have proper nutrition for ulcers?
Proper nutrition is crucial to ensure effective and proper wound healing.
What are the symptoms of bedsore?
Spine. Shoulder blades. Back of arms and legs. But each stage of bedsore has different symptoms. Depending on the stage, the symptoms are the following:
Why do you apply dressings on a wound?
Apply dressing to protect the wound and improve healing.
What are the risks of developing bed sores?
If a person is suffering from any of these conditions, the risk of developing bed sores get even higher. Here they are: Poor Mobility/Immobility - People who are unable to change their position independently or completely immobile are at greater risk of developing pressure ulcers.
What is pressure ulcer?
Pressure ulcers are sores that occur when pressure cuts off the blood supply to the skin. Stress caused by the body’s weight and the impact of striking the ground place the ball of the foot, the big toe, and the heel at the greatest risk. Left untreated, an ulcer may allow infection to enter your body. If infection reaches the bloodstream ...
How to prevent pressure ulcers?
By taking care of yourself , you may be able to prevent pressure ulcers. At the very least, you can reduce your risk of getting one. Try to check your feet daily and improve your overall health. Also, protect your feet by wearing shoes and socks that don’t rub.#N#Checking Your Feet#N#Use a mirror to look at the bottom of your feet each day. By doing so, you can catch small skin changes before they turn into ulcers. Call your doctor if you notice any hot spots, red streaks, swelling, or any cracks or sores. Also, check the soles and insides of your shoes before putting them on. Remove any objects, such as pebbles.#N#Improving Your Overall Health#N#Do your best to control health problems that may affect your feet, such as diabetes and kidney disease. Eat right and exercise. If you are given medications, take them as directed. If you smoke, stop. Smoking reduces blood flow and slows healing. Limiting alcohol intake may also be helpful.
What causes a white discharge?
Infected Ulcers. If bacteria enter the ulcer, infection sets in. This causes more healthy tissue to die. The infected ulcer may begin to drain. The discharge may be white, yellow, or greenish. Some infected ulcers bleed or have a bad odor. If you develop an infected ulcer, call your doctor right away.
What causes red spots on the skin?
As healthy skin dies, an ulcer forms. Ulcers may progress from hot spots to infected wounds very quickly. A callus pressing into the foot may kill healthy tissue and cause an ulcer. Red “hot” spots on the skin are signs of pressure or friction. They are a warning that you need to take care of your feet.
How to treat a sore in a hot spot?
Surgery may also be needed if the infection has spread.#N#Cleaning the Ulcer#N#To assist healing, thickened skin around the ulcer may be cleaned away. Medicated ointment or cream may be applied to prevent infection. Sometimes a special dressing isused to help keep the wound dry.#N#Reducing Force#N#To take pressure off hot spots and ulcers, your doctor may prescribe orthoses. These custom-made shoe inserts absorb or divert pressure from problem areas. Special shoes or temporary casts may also be used.#N#Using Antibiotics#N#To control or prevent infection, your doctor may prescribe antibiotics. Take them all, and take them as directed. If you stop using an antibiotic too soon, the infection may come back.#N#If Surgery Is Needed#N#Surgery may be needed if infection enters deep tissues or bone. In such cases, your doctor cleans away the infection while removing as little tissue or bone as possible. You may also be given intravenous (IV) antibiotics to fight the infection.
What causes a callus on the bottom of the foot?
Force or friction against the bottom of your foot causes the skin to thicken, forming a callus. If the skin keeps thickening, the callus presses up into the foot. This kills healthy tissue and causes pain.
How to reduce pressure on hot spots?
To take pressure off hot spots and ulcers, your doctor may prescribe orthoses. These custom-made shoe inserts absorb or divert pressure from problem areas. Special shoes or temporary casts may also be used. Using Antibiotics. To control or prevent infection, your doctor may prescribe antibiotics.
Overview
- Bedsores — also called pressure ulcers and decubitus ulcers — are injuries to skin and underlying tissue resulting from prolonged pressure on the skin. Bedsores most often develop on skin that covers bony areas of the body, such as the heels, ankles, hips and tailbone. People most at risk of bedsores have medical conditions that limit their ability...
Symptoms
- Warning signs of bedsores or pressure ulcers are: 1. Unusual changes in skin color or texture 2. Swelling 3. Pus-like draining 4. An area of skin that feels cooler or warmer to the touch than other areas 5. Tender areas Bedsores fall into one of several stages based on their depth, severity and other characteristics. The degree of skin and tissue damage ranges from changes in skin color t…
Causes
- Bedsores are caused by pressure against the skin that limits blood flow to the skin. Limited movement can make skin vulnerable to damage and lead to development of bedsores. Three primary contributing factors for bedsores are: 1. Pressure. Constant pressure on any part of your body can lessen the blood flow to tissues. Blood flow is essential for delivering oxygen and othe…
Risk Factors
- Your risk of developing bedsores is higher if you have difficulty moving and can't change position easily while seated or in bed. Risk factors include: 1. Immobility.This might be due to poor health, spinal cord injury and other causes. 2. Incontinence.Skin becomes more vulnerable with extended exposure to urine and stool. 3. Lack of sensory perception.Spinal cord injuries, neurological diso…
Complications
- Complications of pressure ulcers, some life-threatening, include: 1. Cellulitis.Cellulitis is an infection of the skin and connected soft tissues. It can cause warmth, inflammation and swelling of the affected area. People with nerve damage often do not feel pain in the area affected by cellulitis. 2. Bone and joint infections.An infection from a pressure sore can burrow into joints an…
Prevention
- You can help prevent bedsores by frequently repositioning yourself to avoid stress on the skin. Other strategies include taking good care of your skin, maintaining good nutrition and fluid intake, quitting smoking, managing stress, and exercising daily.