Why do viruses become resistant to antivirals?
Drug resistance in viruses Antiviral drug resistance is an increasing concern in immunocompromised patient populations, where ongoing viral replication and prolonged drug exposure lead to the selection of resistant strains. Resistance has developed to most antivirals including antiretroviral (ARV) drugs.
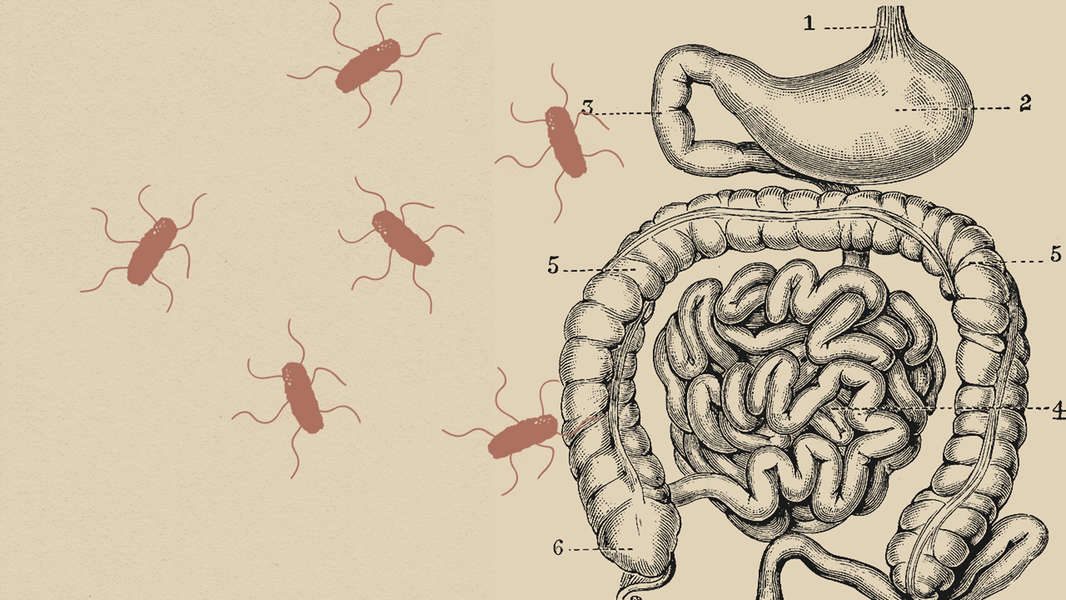
How do bacteria become resistant to drugs?
Bacteria multiply by the billions. Bacteria that have drug-resistant DNA may transfer a copy of these genes to other bacteria. Non-resistant bacteria receive the new DNA and become resistant to drugs. In the presence of drugs, only drug-resistant bacteria survive. The drug-resistant bacteria multiply and thrive.
What is antiretroviral drug resistance?
Antiviral drug resistance is an increasing concern in immunocompromised patient populations, where ongoing viral replication and prolonged drug exposure lead to the selection of resistant strains. Resistance has developed to most antivirals including antiretroviral (ARV) drugs.
What causes HIV drug resistance?
HIV drug resistance is caused by changes in the genetic structure of HIV that affect the ability of medicines to block the replication of the virus. All antiretroviral drugs, including those from newer drug classes, are at risk of becoming partially or fully inactive due to the emergence of drug-resistant virus.

Can viruses be resistant to drugs?
Reduced susceptibility detected using laboratory tests can be a sign of potential antiviral drug resistance in clinical settings. Typically, flu virus is called resistant after sufficient evidence was gathered to prove a lack of antiviral effect of a particular antiviral medication in patients infected with such virus.
What causes resistance to drugs?
Microbes also may get genes from each other, including genes that make the microbe drug resistant. Bacteria multiply by the billions. Bacteria that have drug-resistant DNA may transfer a copy of these genes to other bacteria. Non-resistant bacteria receive the new DNA and become resistant to drugs.
Do viruses build resistance?
Like all microorganisms, viruses can develop resistance to the drugs meant to treat them, and not only in clinical situations.
What is antibiotic and antiviral drug resistance How does it happen?
Antimicrobial resistance occurs when microorganisms such as bacteria, viruses, fungi and parasites change in ways that render the medications used to cure the infections they cause ineffective. When the microorganisms become resistant to most antimicrobials they are often referred to as “superbugs”.
What are the 5 mechanisms of drug resistance?
The main mechanisms of resistance are: limiting uptake of a drug, modification of a drug target, inactivation of a drug, and active efflux of a drug. These mechanisms may be native to the microorganisms, or acquired from other microorganisms.
How is drug resistance acquired?
Acquired antimicrobial resistance is the result of an evolutionary process by which microorganisms adapt to antibiotics through several mechanisms including alteration of drug target by mutations and horizontal transfer of novel/foreign genes, referred to as resistance genes.
Can viruses become immune to antibiotics?
Antibiotic resistance occurs when bacteria develop defenses against the antibiotics designed to kill them. Antimicrobial resistance is a broader term that applies not only to bacteria but also to other germs, such as viruses or fungi, that may develop such defenses.
Are viruses immune to antibiotics?
Antibiotics DO NOT work on viruses, such as those that cause colds, flu, or COVID-19. Antibiotics also are not needed for many sinus infections and some ear infections. When antibiotics aren't needed, they won't help you, and the side effects could still cause harm.
How does antibiotic resistance happen?
Antibiotic resistance occurs when bacteria change in response to the use of these medicines. Bacteria, not humans or animals, become antibiotic-resistant. These bacteria may infect humans and animals, and the infections they cause are harder to treat than those caused by non-resistant bacteria.
What is meant by drug resistance?
Listen to pronunciation. (... reh-ZIH-stunts) When cancer cells or microorganisms, such as bacteria or viruses, don't respond to a drug that is usually able to kill or weaken them.
How do you know if you are antibiotic-resistant?
Your healthcare provider may take a sample of your infected tissue and send it to a lab. There, the type of infection can be figured out. Tests can also show which antibiotics will kill the germs. You may have an antibiotic-resistant infection if you don't get better after treatment with standard antibiotics.
What are examples of antibiotic resistance?
Important examples are:methicillin-resistant Staphylococcus aureus (MRSA)vancomycin-resistant Enterococcus (VRE)multi-drug-resistant Mycobacterium tuberculosis (MDR-TB)carbapenem-resistant Enterobacteriaceae (CRE) gut bacteria.
What does it mean to be resistant to a drug?
reh-ZIH-stunts) When cancer cells or microorganisms, such as bacteria or viruses, don't respond to a drug that is usually able to kill or weaken them. Drug resistance may be present before treatment is given or may occur during or after treatment with the drug.
What is the cause of tolerance?
A tolerance develops when a person has been regularly taking a drug and their body begins to adapt itself to the presence of the chemicals in the drug. It is a gradual process but using larger quantities of a substance can drastically decrease the amount of time it takes to begin.
What is the main cause of antibiotic resistance?
The main cause of antibiotic resistance is antibiotic use. When we use antibiotics, some bacteria die but resistant bacteria can survive and even multiply. The overuse of antibiotics makes resistant bacteria more common. The more we use antibiotics, the more chances bacteria have to become resistant to them.
What is an example of drug resistance?
Some bacteria have developed resistance to antibiotics that were once commonly used to treat them. For example, Staphylococcus aureus ('golden staph' or MRSA) and Neisseria gonorrhoeae (the cause of gonorrhoea) are now almost always resistant to benzyl penicillin.
How does antibiotic resistance happen?
How Antibiotic Resistance Happens. Antibiotics save lives but any time antibiotics are used, they can cause side effects and lead to antibiotic resistance. Since the 1940s, antibiotics have greatly reduced illness and death from infectious diseases. However, as we use the drugs, germs develop defense strategies against them.
How do antibiotics fight germs?
Antibiotics fight germs (bacteria and fungi). But germs fight back and find new ways to survive. Their defense strategies are called resistance mechanisms . Bacteria develop resistance mechanisms by using instructions provided by their DNA. Often, resistance genes are found within plasmids, small pieces of DNA that carry genetic instructions from one germ to another. This means that some bacteria can share their DNA and make other germs become resistant.
What bacteria break down antibiotics?
Germs change or destroy the antibiotics with enzymes, proteins that break down the drug. Example: Klebsiella pneumoniae bacteria produce enzymes called carbapenemases, which break down carbapenem drugs and most other beta-lactam drugs. Bypass the effects of the antibiotic.
How did antibiotics help the world?
However, as we use the drugs, germs develop defense strategies against them. This makes the drugs less effective.
What is the name of the drug that treats infections?
Antimicrobials Treat Infections Caused by Microbes. Microbes are very small living organisms, like bacteria. Most microbes are harmless and even helpful to humans, but some can cause infections and disease. Drugs used to treat these infections are called antimicrobials .
Can Staphylococcus aureus be bypassed?
Example: Some Staphylococcus aureus bacteria can bypass the drug effects of trimethoprim . Change the targets for the antibiotic. Many antibiotic drugs are designed to single out and destroy specific parts (or targets) of a bacterium. Germs change the antibiotic’s target so the drug can no longer fit and do its job.
Can germs resist antibiotics?
Germs can use defense strategies to resist the effects of antibiotics. Here are a few examples.
How do bacteria become drug resistant?
Gene Transfer. Microbes also may get genes from each other, including genes that make the microbe drug resistant. Bacteria multiply by the billions. Bacteria that have drug-resistant DNA may transfer a copy of these genes to other bacteria. Non-resistant bacteria receive the new DNA and become resistant to drugs.
What are the causes of antibiotic resistance?
Causes of Antimicrobial (Drug) Resistance. Microbes, such as bacteria, viruses, fungi, and parasites, are living organisms that evolve over time. Their primary function is to reproduce, thrive, and spread quickly and efficiently. Therefore, microbes adapt to their environments and change in ways that ensure their survival.
Why do we add antibiotics to food?
Scientists also believe that the practice of adding antibiotics to agricultural feed promotes drug resistance. More than half of the antibiotics produced in the United States are used for agricultural purposes. 1, 2 However, there is still much debate about whether drug-resistant microbes in animals pose a significant public health burden.
How do microbes reproduce?
Most microbes reproduce by dividing every few hours, allowing them to evolve rapidly and adapt quickly to new environmental conditions . During replication, mutations arise and some of these mutations may help an individual microbe survive exposure to an antimicrobial.
How do microbes adapt to their environment?
Therefore, microbes adapt to their environments and change in ways that ensure their survival. If something stops their ability to grow, such as an antimicrobial, genetic changes can occur that enable the microbe to survive. There are several ways this happens.
Do antimicrobials increase resistance?
However, there are additional societal pressures that act to accelerate the increase of antimicrobial resistance.
Do microbes survive in the presence of antimicrobials?
In the presence of an antimicrobial, microbes are either killed or, if they carry resistance genes, survive. These survivors will replicate, and their progeny will quickly become the dominant type throughout the microbial population.
How do viruses become resistant to drugs?
Viruses, and bacteria, usually become resistant to drugs through genetic changes that allow them to thrive in the presence of a drug that would ordinarily kill them.
What trick often works in ovrercoming bacterial resitance to antibiotics?
Dr. Hirsch said that another trick that often works in ovrercoming bacterial resitance to antibiotics is to give two different drugs alternately.
Is the resistance to viral drugs a new phenomenon?
The resistance to the viral drugs ''is a new phenomenon,'' said Dr. Martin S. Hirsch of the Massachusetts General Hospital in Boston. ''It is something we have feared,'' he said, but since it was not observed in the eight years since the first antiviral drug was developed, ''we had become a little bit sanguine.''
Is azidothymidine resistant to AIDS?
Dr. Hirsch said he is concerned that other antiviral drugs, including AZT, or azidothymidine, the only drug approved for the treatment of the AIDS virus, may also be thwarted by resistant viruses. The AIDS virus has become resistant to AZT in laboratory experiments, Dr. Hirsch said, and ''it stands to reason that sooner or later there will be resistant variants in patients.''
Why is antimicrobial resistance a global concern?
The emergence and spread of drug-resistant pathogens that have acquired new resistance mechanisms, leading to antimicrobial resistance, continues to threaten our ability to treat common infections. Especially alarming is the rapid global spread of multi- and pan-resistant bacteria (also known as “superbugs”) that cause infections that are not treatable with existing antimicrobial medicines such as antibiotics.
What are the high rates of resistance against antibiotics?
For example, the rate of resistance to ciprofloxacin, an antibiotic commonly used to treat urinary tract infections, varied from 8.4% to 92.9% for Escherichia coli and from 4.1% to 79.4% for Klebsiella pneumoniae in countries reporting to the Global Antimicrobial Resistance and Use Surveillance System (GLASS).
What is the term for the change in the way bacteria, viruses, fungi, and parasites respond to?
Antimicrobial Resistance (AMR) occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines making infections harder to treat and increasing the risk of disease spread, severe illness and death.
Why are antibiotics so ineffective?
Antibiotics are becoming increasingly ineffective as drug-resistance spreads globally leading to more difficult to treat infections and death.
What drugs have gonorrhoea resistance?
Resistance has rapidly emerged to sulphonamides, penicillins, tetracyclines, macrolides, fluoroquinolones, and early generation cephalosporins. Currently, in most countries, the injectable extended-spectrum cephalosporin (ESC) ceftriaxone is the only remaining empiric monotherapy for gonorrhoea.
Why are ARV drugs inactive?
All antiretroviral (ARV) drugs, including newer classes, are at risk of becoming partly or fully inactive because of the emergence of drug-resistant HIV (HIVDR). People receiving antiretroviral therapy can acquire HIVDR, and people can also be infected with HIV that is already drug resistant. Levels of pretreatment HIVDR (PDR) to non-nucleoside reverse-transcriptase inhibitors (NNRTIs) among adults initiating first-line therapy exceeded 10% in the majority of the monitored countries in Africa, Asia and Latin America. The prevalence of PDR among infants is alarmingly high. In sub-Saharan Africa, over 50% of the infants newly diagnosed with HIV carry a virus that is resistant to NNRTI. Informed by these findings, latest WHO ARV guidelines now recommend the adoption of a new drug, dolutegravir, as the preferred first-line treatment for adults and children. The use of this drug is particularly urgent in averting the negative effects of resistance to NNRTIs.
Is artemisinin resistance in Rwanda?
In Africa, evidence has recently been published showing emergence of mutations linked to partial artemi sinin resistance in Rwanda. So far, ACTs that have been tested remain highly efficacious. However, further spread of resistance to artemisinin and ACT partner drugs could pose a major public health challenge and jeopardize important gains in malaria control.
What is drug resistance?
Drug resistance is defined as a reduced susceptibility to a drug in a laboratory culture system and is expressed as an altered IC50or IC90(drug concentration required to inhibit viral growth by 50% or 90% respectively). This is termed the phenotype. This phenotype is determined by specific mutations in the viral genome (the genotype), which leads to alterations in the viral target protein (for example, HIV reverse transcriptase) or the viral drug activator (for example, herpes simplex thymidine kinase). The high rate of replication of some viruses determines that many of these genetic variants will already exist in untreated infected people. This is consequent on an inherent error rate of viral polymerases, especially for RNA viruses such as HIV1and influenza, which replicate the viral genome. A wide range of viral variants, including those with mutations associated with drug resistance, will therefore be present. This collection of variants in one person is termed the viral quasispecies, with the “fittest” virus representing the majority population. The use of an antiviral drug will provide a selective pressure for the preferential growth of variants with a reduced susceptibility to drugs in accordance with Darwinian evolutionary principles. The emergent drug resistant virus will be the fittest in the presence of drug. Some drug resistant viruses, however, seem not to replicate as well as wild type virus (in the absence of drug).2In some cases, multiple mutations are required for the development of high level resistance, and insufficient suppression of viral replication by antiviral drugs will predispose to their sequential acquisition.
When does resistance develop?
Resistance develops rapidly when viral replication is not maximally suppressed
What is the best treatment for herpes simplex?
Drugs such as aciclovir, valaciclovir, and famciclovir are widely used to treat infections with herpes simplex and varicella zoster. In general, drug resistance is limited to patients who are immunocompromised; the estimated prevalence of herpes simplex resistant to aciclovir is 5-10% in patients with AIDS and recipients of bone marrow transplants.17,18Long term ganciclovir treatment of cytomegalovirus infections in this group of patients can also lead to resistance.19Second line treatments are of proved efficacy,20,21and drug susceptibility assays should be performed in immunocompromised patients with unresponsive herpes simplex infections to distinguish true antiviral resistance from other causes of clinical non-responsiveness such as poor drug absorption. Although drug resistance of herpes simplex is exceedingly rare in patients whose immune system is not compromised (estimated prevalence is 0.5% in genitourinary medicine clinics in the United States),17vigilance is required as the use of these drugs increases in primary care and over the counter preparations become available. Only one case of transmission of aciclovir resistant herpes has been documented to date.22Current understanding of the latent state of herpes simplex suggests that resistant virus shed at epithelial surfaces will revert to the wild type on subsequent reactivations, and this may limit the spread of resistant virus to others.
Why do drug treatments fail?
The primary reasons whytreatment fails are many and include poor drug compliance, pharmacological factors, and drug resistance, but in many cases failure occurs withresistant virus. Adherence to treatment regimens that may entail 30 or more tablets daily is less than ideal, and simplified strategies, such as once daily dosing and reducing the number of pills, are required. The drug resistant viruses present when treatment fails may have reduced susceptibilities to other drugs in the same class, or even multidrug resistance,8and this limits the success of second line salvage treatment. The clinical usefulness of drug resistance assays in guiding effective salvage treatments requires urgent investigation.9
Who receives funding for antiviral research?
Conflict of interest: The Public Health Laboratory Service obtains funding for antiviral research from GlaxoWellcome and Roche Pharmaceuticals.
Is viral resistance inevitable?
The emergence of viral resistance against any specific and potent drug is virtually inevitable. Drug resistance is costly to the health service, to the patient who fails to gain maximum therapeutic benefit, and for the community in which resistant viruses may be spread. For persistent infections, resistance will develop more rapidly in the face of suboptimal virus suppression, and every attempt must be made to implement appropriate therapeutic regimens. Clear diagnostic and therapeutic guidelines are required on using antiviral agents in primary care against, for example, shingles and influenza. Finally, there is an urgent need to clarify the most effective use of antiviral resistance assays in clinical practice.
Is virally encoded drug resistance genetic?
Against this exciting background comes the news of drug resistance. Virally encoded drug resistance has been document ed against nearly all compounds with antiviral activity, and the genetic basis of resistance is now known.
Why is HIV drug resistant?
HIV drug resistance is caused by changes in the genetic structure of HIV that affect the ability of drugs to block the replication of the virus. All current antiretroviral drugs, including newer classes, are at risk of becoming partly or fully inactive because of the emergence of drug-resistant virus strains.
Why is stopping HIV drug resistance important?
Stopping HIV drug resistance is important to ensure the long-term efficacy and durability of available medicines to treat HIV.
Why is it important to have a continuous supply of antiretroviral drugs?
A continuous supply of antiretroviral drugs is essential to avoid treatment interruption and prevent the emergence and spread of HIV drug resistance. Limited access to health centres can result in treatment interruption among individuals on antiretroviral therapy.
What happens if you don't prevent HIV?
If not prevented, HIV drug resistance can jeopardize the efficacy of antiretroviral drugs, resulting in increased numbers of HIV infections and HIV-associated morbidity and mortality.
What is the WHO report on HIV 2021?
WHO’s Report on HIV drug resistance 2021 shows substantial progress in the development of national action plans to prevent, monitor and respond to HIV drug resistance and the implementation of nationally representative surveys in low- and middle-income countries. As of 2021, 64% of countries with a high burden of HIV have developed national action plans. Between 2004 and 2021, 66 countries implemented surveys of HIV drug resistance using WHO-recommended standard methods, and 34 countries plan to conduct HIV drug resistance surveys within the next two years.
What is the purpose of HIV drug resistance surveillance?
Surveillance of HIV drug resistance provides countries with evidence that can be used to optimize patient and population-level treatment outcomes. WHO recommends that countries routinely implement nationally representative HIV drug resistance surveys among different populations, including adults, children and adolescents.
How old is HIV resistant?
HIV drug resistance is also alarmingly high in children under 18 months of age that are newly diagnosed with HIV. Surveys conducted in 9 countries in sub-Saharan Africa between 2012 and 2018 found that over half of the infants newly diagnosed with HIV carry a virus that is resistant to the standard NNRTI class of drugs.
How to prevent antibiotic resistance?
To help fight antibiotic resistance and protect yourself against infection: 1 Don't take antibiotics unless you're certain you need them. An estimated 30% of the millions of prescriptions written each year are not needed. Always ask your doctor if antibiotics will really help. For illnesses caused by viruses -- common colds, bronchitis, and many ear and sinus infections -- they won't. 2 Finish your pills. Take your entire prescription exactly as directed. Do it even if you start feeling better. If you stop before the infection is completely wiped out, those bacteria are more likely to become drug-resistant. 3 Get vaccinated. Immunizations can protect you against some diseases that are treated with antibiotics. They include tetanus and whooping cough. 4 Stay safe in the hospital. Antibiotic-resistant bacteria are commonly found in hospitals. Make sure your caregivers wash their hands properly. Also, ask how to keep surgical wounds free of infection.
Why do some bacteria resist antibiotics?
Others can become resistant if their genes change or they get drug-resistant genes from other bacteria. The longer and more often antibiotics are used, the less effective they are against those bacteria.
What should scientists do to help prevent antibiotic resistance?
Scientists should step up the development of new antibiotics and vaccines as well as diagnostic tests to identify drug-resistant bacteria. Public health officials should monitor antibiotic resistance and track its spread. Doctors should help stop unnecessary antibiotic use and develop safer practices in hospitals and clinics.
What is the purpose of antibiotics?
The discovery of antibiotics changed medicine in the 20th century. Today, they're widely used to treat infections caused by bacteria.
How to stay safe in a hospital?
Stay safe in the hospital. Antibiotic-resistant bacteria are commonly found in hospitals. Make sure your caregivers wash their hands properly. Also, ask how to keep surgical wounds free of infection.
Can resistance cause death?
In some cases, these infections result in death. Resistance also makes it more difficult to care for people with chronic diseases. Some people need medical treatments like chemotherapy, surgery, or dialysis, and they sometimes take antibiotics to help reduce the risk of infection.
Should doctors stop antibiotics?
Doctors should help stop unnecessary antibiotic use and develop safer practices in hospitals and clinics. Farmers should stop giving animals antibiotics needed to treat diseases in people.
