When monitoring a patient’s airway, assess his or her respiratory status by simply observing for the following factors:
- Mental status
- Skin color, temperature, and dryness
- Breathing rate and quality of respirations
- Work of breathing and accessory muscle use
- Chest expansion symmetry and depth
- Obvious signs of chest trauma or wounds
Why is the assessment of the patient's airway important?
The assessment of the patient's airway is an integral part of the pre-operative workup. Its purpose is to predict potential problems, allowing a management plan to be developed ahead of time and avoid an unanticipated difficult airway.
How easy is basic airway assessment?
Basic Airway Assessment: It’s as easy as… 1-2-3? In medical school, many multiple-choice questions in the setting of an acutely ill patient have an option of “managing the ABC’s” and it is always the correct answer.
What is patency in Airway assessment?
Patency is our primary concern in airway assessment, but the patient who can talk does not necessarily have a PATENT airway. Think about a patient with bad airway edema from a laryngeal fracture, or a patient with an inhalational injury.
What is included in a preoprative Airway assessment?
Like any kind of patient evaluation preoprative airway assessment can be divided into history and examination, supported by clinical tests. The Australian VORTEX appraoch website has a fantastic page on preoperative airway assessment and planning.

When assessing the airway of the patient we have to check for?
A thorough, but brief, airway assessment is essential to manage patients requiring advanced airway management. Indications for the use of airway management are: (1) failure to oxygenate; (2) failure to ventilate; (3) failure to maintain a patent airway.
What does the nurse look for when assessing airway?
Respiratory deterioration The aim of airway assessment is to establish patency and assess the risk of deterioration in patients' ability to protect their airway with an effective cough and gag reflex. The airway can be clear, partially obstructed, or completely obstructed (Coombs et al, 2013).
How do you assess airway on ABC?
0:003:22Checking airway, breathing and circulation (ABC) - YouTubeYouTubeStart of suggested clipEnd of suggested clipWe need to make sure that we manage somebody's airway quite quickly but quite effectively as well soMoreWe need to make sure that we manage somebody's airway quite quickly but quite effectively as well so the first thing we need to do is make sure that the tongue hasn't fallen back into the throat.
How do you assess a difficult airway?
There are several patient characteristics that have been associated with difficult airway intubation: obesity, head and neck movement, jaw movement, receding mandible, long upper incisors, Mallampatti score, maxillary incisor characteristics, male sex, age 40-59, decreased mouth opening, shortened thyromental distance, ...
Why is the airway The most important assessment when caring for patient?
Its main function is to carry air into the body. The aim of airway assessment is to ensure this anatomical function is achieved and any obstruction (full or partial) of the airway is identified (Table 1). An indication of a patent airway is the patient's ability to speak with a usual voice in full sentences.
What is a simple question you could ask your patient to immediately assess their airway?
Read on for an approach to basic airway assessment....A suggested approach to basic airway assessmentStep 1: Is there evidence of airway OBSTRUCTION now – is it complete or partial?Step 2: Is there a risk of ANTICIPATED airway obstruction?Step 3: Is there a risk of Aspiration from failure to PROTECT their airway?
Why is airway the first priority?
The airway is the most important priority in the management of the severely injured patient. It is essential to open and clear the airway to allow free access of air to the distal endobronchial tree. Manual methods of opening the airway are described.
What is an airway test?
The assessment of the patient's airway is an integral part of the pre-operative workup. Its purpose is to predict potential problems, allowing a management plan to be developed ahead of time and avoid an unanticipated difficult airway.
What is the difference between airway and breathing in ABCs?
A is for airway assessment, observing for airway obstruction which can be seen with a changed sound of voice, “see-saw” respirations, and stridor. B is for breathing assessment, observing for an abnormal respiratory rate, the use of accessory muscles for respiration, and cyanosis.
What should you look for when breathing assessed?
look to see if their chest is rising and falling. listen over their mouth and nose for breathing sounds. feel their breath against your cheek for 10 seconds.
What 7 things are you looking at when you assess a patient respiratory function?
Observe the patient for important respiratory clues:Check the rate of respiration.Look for abnormalities in the shape of the patient's chest.Ask about shortness of breath and watch for signs of labored breathing.Check the patient's pulse and blood pressure.Assess oxygen saturation.
What is the first step in assessing a patient's airway?
All health care professionals, regardless of the setting, can assess the airway as described and use a head-tilt and chin-lift maneuver to open the airway (Figure 2). With the proper equipment, suction of the airways to remove obstructions, for example, blood or vomit, is recommended.
How do you assess airway patency in nursing?
“Once the cuff is completely deflated, airway patency can be determined by assessing voicing on exhalation, listening for exhalation though the upper airway using a stethoscope, or by reading the peak inspiratory pressure (PIP) and/or exhaled volumes via the ventilator.
What are some interventions to help with obstruction of the airway?
(These simple interventions being: suction, jaw thrust, oral-pharyngeal airway, supplemental O 2).
How is PATENCY assessed?
PATENCY is assessed through the presence/absence of obstructive symptoms (stridor, secretions, snoring, etc.), or findings suggesting an airway that may become obstructed (singed nasal/facial hair, carbonaceous sputum, stab to neck with risk of expanding hematoma).
Can a patient talk but their airway is closed?
They can talk, but their airway may be closing nonetheless. The ability to talk usually implies a PROTECTED airway, not a patent airway. Lack of airway protection is a less urgent matter than patency.
Do you need to intubate an airway?
The next issue is that the indications for definitive airway management involve both airway and breathing, so just because the airway is patent and protected, it doesn’t mean the patient won’t need to be intubated.
Does apneic oxygenation help with hypoxemia?
You would want to use apneic oxygenation as part of your RSI to mitigate the risk of hypoxemia, and choose a sedative agent that will maintain their blood pressure.
Can you intubate with a GCS of 8?
The level of consciousness can always change and along with it the ability to protect the airway from aspiration, however aspiration is not an immediate event the second your GCS hits 8 or less. GCS < 8 is not an absolute indication for intubation. Many intoxicated patients and post-ictal patients live with a GCS or 5 or 6 and wake up a few hours later. They don’t usually aspirate, and can be managed without definitive airway protection. Alternatively the head-injured trauma patient with a GCS of 12 at presentation that is a 10 now probably needs definitive airway management.
How to tell if a patient has a patency in their airway?
The best sign of airway patency in responsive patients is the ability to hold a conversation without changes in the voice or feeling of breathlessness. However, a patient's airway may still be at risk even when they are conversational. Foreign bodies or substances in the mouth may impair the airway at a later time and must be removed.
What is the only absolute indicator of airway status in unresponsive patients?
AIRWAY STATUS: The only absolute indicator of airway status in unresponsive patients is the movement of air. Seeing condensation in oxygen masks, feeling air movement, and using end-tidal CO2 monitors are all good ways of ensuring ventilation is occurring.
How to treat apnea?
APNEA: An absence of breathing should be treated with a re-assessment of the airway followed by rapid initiation of mechanical ventilation, generally via bag valve mask. Patients that are gasping occasionally should be treated as apneic until proven otherwise.
What is an ABC assessment?
Basic Airway Assessment. The basic assessment of any patient, the "ABC's" begins with the airway, a compromised airway is one of the quickest killers in all of medicine, making accurate assessment a priority. This section will review the assessment of the unresponsive patient, the responsive patient, and several special situations ...
What is the respiratory rate of an ABC?
The normal adult resting respiratory rate is 12 to 20 breaths per minute (BPM). Breathing too slow ( bradypnea ), too fast ( tachypnea ), or not at ( apnea) all are commonly encountered conditions in the field.
What are the signs of compromised airways?
DANGER SIGNS: Snoring, gurgling, choking, and coughing are all potential indicators of compromised airways in unconscious patients. If these are occurring it would be wise to reposition the patient or consider airway-related interventions.
Should unresponsive patients have their airway opened and maintained manually?
Unresponsive patients should have their airway opened and maintained manually. Non-Traumatic mechanisms of injury should lead to the usage of the head-tilt and chin-lift technique. While patients with Traumatic injuries that may compromise the C-spine are limited to the jaw-thrust technique.
What is the purpose of an airway assessment?
Its purpose is to predict potential problems, allowing a management plan to be developed ahead of time and avoid an unanticipated difficult airway.
How to find problems with airway management?
Look at old anesthetic records, if they are available, to see if problems with airway management were documented. In practice this means finding comments on ease or difficulty of bag-mask ventilation, laryngoscopy view, and any special airway techniques or equipment used previously. You might even consider requesting records from a different hospital if airway management is expected to be particularly challenging and time allows.
Why is preoperative airway assessment important?
There are some easily overlooked aspects of preoperative airway assessment because they go beyond the more familiar medical history and examination discussed above and have more to do with logistics. They are nevertheless crucial to the development of your airway management plan, just as the assessments described above are.
How to measure IIG?
Similarly to the measurement of thyromental distance (TMD) (see below), measurement of IIG is usually done by finger breadths in clinical practice rather than a tape measure. Ask the patient if they can insert 2 and then 3 fingers between their upper and lower incisiors.
What is STOP BANG assessment?
You are likely to come across patients who have not definitiely been diagnosed with OSA but in whom you strongly suspect it. A screening score such as the STOP-BANG assessment, developed by the University Health Network in Toronto, CA, is helpful in identifying likely OSA cases and guide overall risk stratification.
What is the red flag for radiotherapy to the neck?
Find out if the patient has had head/ neck surgery before such as laryngeal surgery, neck dissection, facial reconstruction, tracheotomy or c-spine surgery. A particular large red flag is the history of radiotherapy to the neck!
Why is aspiration risk increased?
Certain patients are at an increased risk of regurgitation and aspiration of stomach contents such as food particles or gastric acid because of conditions such as GERD, hiatal hernia, obesity, autonomic neuropathy, non-npo status, etc.
What is the assessment of ventilation?
Assessment of Ventilation. Ventilation is the movement of air in and out of the lungs through a patent airway. The majority of observations regarding ventilations focus on the movements of the chest.
How to know if you have adequate ventilation?
SIGNS OF ADEQUATE VENTILATION: In most patients, your assessment of ventilation will be based on observing their respiratory rate (normal 12 to 20) and listening for clear breathing sounds in the left and right chest. Auditor y confirmation of breathing sounds is the strongest sign of adequate ventilation. In patients on ventilators or bag-valve-mask, this does not change.
How to treat apnea?
APNEA: An absence of breathing should be treated with a re-assessment of the airway followed by rapid initiation of mechanical ventilation, generally via bag valve mask. Patients that are gasping occasionally should be treated as apneic until proven otherwise.
What is the strongest sign of inadequate ventilation?
Auditory confirmation of breathing sounds is the strongest sign of adequate ventilation. In patients on ventilators or bag-valve-mask, this does not change. SIGNS OF INADEQUATE VENTILATION: The signs of inadequate ventilation are best broken down into what you can see and what you can hear.
What is the work of breathing?
"Work of breathing" refers to the difficulty of taking a breath, patients at rest should have no difficulty carrying on a conversation without stopping to catch their breath.
How to find the amount of air a person breathes per minute?
MINUTE VENTILATION: the amount of air that a person breathes per minute, it is found by multiplying respiratory rate and tidal volume. (RR x TV = Minute Ventilation).
Can you breathe with a rib?
They should not be using the muscles in their neck or ribs to take a breath, and they should not be sweating or bending over to breathe. *This is not specific to ventilation, patients with poor oxygenation or poor respiration may also have these same signs.
A Systematic Approach Is Key
In the world of emergency medicine, surprise is the name of the game. Take a systematic approach to everything. If you focus solely on the airway, you may miss a more critical symptom. For example, a patient who seems to be choking may actually be in a state of anaphylaxis. Or consider the patient who suffers a traumatic pneumothorax incident.
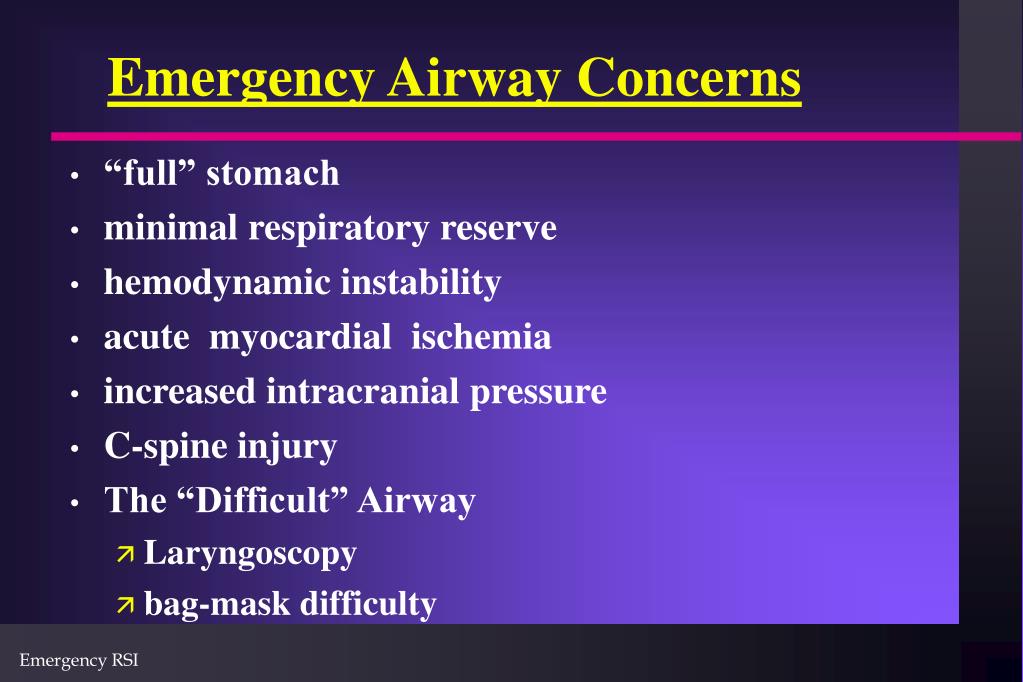
You Must Assess for a Difficult Airway
Before intubating the patient, assessing for a difficult airway is critical. Many first responders fear difficult airways, and especially worry about the dreaded “can’t intubate, can’t oxygenate” (CICO) crisis. Assessments save lives and time because a slight change in strategy can overcome the challenges of a difficult airway.
Choose the Right Equipment
The right equipment is a key ingredient in the recipe for successfully treating all airways, but especially difficult ones. Quality equipment also matters in challenging scenarios, such as when a patient is vomiting while aspirating.
How to check airway?
1. Position the victim. Before you can check the airway, the victim needs to be in the right position. If there is any exudate (vomit, blood, etc.) in or around the person's mouth, put on a glove and remove it to clear the airway before you roll her. Roll the person onto her back.
How to open the airway when laying on the ground?
To open the airway when he is laying on the ground, his head and breathing passages need to be aligned correctly. Place one hand behind his head and one hand under his chin. Tilt his head backward toward the sky. The chin should end in a slightly lifted position, as if he were sniffing the air. [5]
How to open the airway in a sailor?
To open the airway when he is laying on the ground, his head and breathing passages need to be aligned correctly. Place one hand behind his head and one hand under his chin. Tilt his head backward toward the sky.
How to remove foreign objects from the airway?
This may be from a foreign object, by the victim's tongue, or by vomit or other bodily fluids. If the airway is obviously obstructed by vomit or any removable matter, get it out of the mouth with a quick swipes with two or three fingers in her mouth. You can quickly turn the victim’s head to one side to assist in the removal.
How to get airway out of mouth?
This may be from a foreign object, by the victim's tongue, or by vomit or other bodily fluids. If the airway is obviously obstructed by vomit or any removable matter, get it out of the mouth with a quick swipes with two or three fingers in her mouth.
What to do if chest is not rising?
If there is not a rise of the chest, try to re-position the airway a little in either direction. You may have gone too far or not far enough to open the airway. If the patient is gasping for breath or breathing poorly, treat this as not breathing and check for circulation.
How to help a victim breathe?
Opening the airway may be enough to start the victim breathing again. If this happens, roll the victim onto his side so there is less pressure on his chest. This will help him breathe better.
What is the airway?
The airway includes the nose, mouth, larynx, pharynx, trachea, bronchi and bronchioles (Cathala and Costa, 2019). Its main function is to carry air into the body. The aim of airway assessment is to ensure this anatomical function is achieved and any obstruction (full or partial) of the airway is identified (Table 1). An indication of a patent airway is the patient’s ability to speak with a usual voice in full sentences.
What do nurses need to do to perform an A-G assessment?
Nurses performing the assessment need to explain to the patient what they are going to do and seek their informed consent. Before approaching the patient, they need to undertake a risk assessment of the environment to determine whether it is safe to undertake the A-G assessment.
What is the A-G method?
The A-G method is a systematic and structured approach of assessing patients, useful both in routine and emergency situations. It is based on the ABCDE approach used when resuscitation may be needed, extended by two additional steps.
What is the importance of blood glucose in disability assessment?
Clinical judgement should be used if the patient is not diabetic; blood glucose levels may not need to be checked but if there are signs of altered levels of consciousness (Box 3) then the blood glucose level should be measured. Measuring arterial or venous blood gas can be helpful in such situations. In diabetic patients with high blood sugar levels, it is important to look for signs of ketoacidosis (Box 3).
What is the oxygen saturation of a patient?
Looking for any respiratory distress signs (Box 1), assessing the depth and pattern of the respiratory cycle for 15 seconds and counting the respiratory rate for a full minute is recommended The acceptable oxygen saturation is >96% for patients without hypercapnic respiratory failure or chronic obstructive pulmonary disease (COPD) and 88-92% for patients with those conditions or at risk of worsening hypercapnia (Williams, 2019; National Guideline Centre, 2010; National Institute for Health and Care Excellence, 2018; O’Driscoll et al, 2008). The patient’s ability to talk in full sentences is a good indicator of their breathing status.
What is disability assessment?
Disability assessment focuses on the main causes of reduced consciousness such as fainting (falls and mobility), drugs (polypharmacy and side effects), alcohol, poisons and hypoglycaemia. The patient’s ACVPU status should be assessed. ACPVU stands for alert, confusion (new), response to voice, painful stimuli, and unconscious (Smith et al, 2017).
What is the process by which air moves in and out of the lungs, allowing gaseous exchange?
Breathing is the process by which air moves in and out of the lungs, allowing gaseous exchange. It should be:
What is the airway of a burn patient?
The airway of the burn patient presents ongoing challenges and special considerations during the period of initial burn injury and throughout the patient’s hospital course. As a consequence of their injuries, some burn patients have airway difficulties throughout the remainder of their lives.
What is failure to secure an airway?
Failure to secure an airway was one of the most common complications occurring during patient transport. The fact that airway obstruction can develop very quickly in burn patients and that the experience and equipment of EMS are often limited supports intubation in the field before transport in the patient with a potential for respiratory compromise.
What is the diagnosis of inhalational trauma?
In the unintubated patient, the presence of soot in the sputum, dyspnea, tachypnea, hoarseness, and stridor are signs of impending airway obstruction. Fiberoptic endoscopy is the gold standard for the diagnosis of inhalational trauma.10–17In the awake patient, a nasal fiberoptic examination under local anesthesia can be performed to evaluate the larynx and confirm the presence or absence of edema and soot. Patients with altered mental status, dyspnea, hoarseness, or stridor require immediate intubation.
What is the procedure for a burn to the chest and neck?
Figure 44-3Extensive burns to the chest and neck can require immediate escharotomy to facilitate ventilation.
Can an airway obstruction develop quickly in burn patients?
The fact that airway obstruction can develop very quickly in burn patients and that the experience and equipment of EMS are often limited supports intubation in the field before transport in the patient with a potential for respiratory compromise.
Do you need to intubate if you have a fire in your neck?
Patients with a flame injury from a barbecue or fire in an open space may have burns to the neck and face but no airway involvement and therefore do not require early intubation.
Can a large burn cause an airway burn?
Patients with large body surface area burns frequently have airway burns as well (Fig. 44-3). Edema after resuscitative efforts can make intubation impossible. After massive burns, patients develop a hypermetabolic state leading to increased CO2production requiring ventilator support. Some physicians suggest prophylactic intubation for total body surface area burns greater than 30%.10,12,17,22

History
Examination & Clinical Tests
- Always assess the S’s of the Airway. If they are all normal, you can be confident that you are NOT dealing with an immediate or impending airway issue of patency or protection. If there are abnormalities in the S’s, simple airway interventions will temporize the situation until more experienced providers can assist with definitive airway interventi...
Predicting Difficult Intubation and Ventilation- The Value of Testing
Situational Awareness
Assessment of Ventilation
- Like any diagnostic tool, an ideal method of preoperative airway assessment should have high sensitivity and specificity, while maintaining a high predicitve value.Disappointingly, no single test for airway assessment meets these requirements! More on predicting risk below ... This is not an exhaustive list of tests. Others not mentioned here have ...
Respiratory Patterns
- Assessing the airway before surgery using some combination of the tests described above is standard clinical practice. But how good are these tests on their own or in combination to predict which patients will be truly difficult to ventilate and/ or intubate and which ones won't? Unfortunately there is no way to talk about tests and the value of testing without some basic sta…
Assessment of Respiration
- There are some easily overlooked aspects of preoperative airway assessment because they go beyond the more familiar medical history and examination discussed above and have more to do with logistics. They are nevertheless crucial to the development of your airway management plan, just as the assessments described above are. 1. Where are you going to do your airway intervent…
Assessment of Oxygenation
Additional Important Concepts
- PATTERNS OF BREATHING Regular pattern: 1. Normal breathing. /¯\__/¯\__/¯\__/¯\__/¯\__/¯\__ 2. Kussmaul breathing: deep, slow, and labored breathing--sometimes increased in rate--in response to metabolic acidosis. Deep inspirations attempt to blow off CO2 to raise pH. (E.g., DKA.) __|¯¯¯¯|__|¯¯¯¯|__|¯¯¯¯|__|¯¯¯¯|__|¯¯¯¯|__ Irregular pattern: 1. Cheyne-Stokes: "Periodic Breathing." …