
How to Recognize and Assess Pain
- Understanding Pain There are several different categories of pain. 1 Pain can be acute (of recent onset) or chronic. ...
- Severity of Pain The first step in assessing pain is to find out how bad it is at the present moment. ...
- Acceptable Level of Pain ...
- Location of Pain ...
- Palliation and Provocation ...
- Assessing Non-Verbal Signs ...
- Psychosocial Factors ...
- Keep a Record ...
- P = Provocation/Palliation. What were you doing when the pain started? ...
- Q = Quality/Quantity. What does it feel like? ...
- R = Region/Radiation. Where is the pain located? ...
- S = Severity Scale. ...
- T = Timing. ...
- Documentation.
What elements are included in pain assessment?
- P (Provocation/Palliation)- What were you doing when the pain started? What caused it? ...
- Q (Quality)-what does the pain feel like? Is it sharp, dull, tingling? ...
- S (Severe)- on a pain scale from 0-10 with 0 being no pain, where would you rate the pain? How long does the pain last?
- T (Timing)- How often does it occur? ...
How to relieve pain using pressure points?
Pressure points that may offer relief when stimulated include:
- Inner court, the web between one's second and third toes on top of your foot
- On the back of one's shoulder, around a thumb's width above the end of one's armpit.
- Cross your arms, then there will be a vertical grove formed on front of your shoulder, then you can press the center of the groove to relieve shoulder pain
What are the different types of pain assessment tools?
Three ways of measuring pain:
- Self report - what the child says ( the gold standard)
- Behavioural –how the child behaves
- Physiological –clinical observations
How to document pain assessment?
- O nset: When did the pain start? ...
- L ocation: Where is the pain?
- D uration: How long has the pain been going on? ...
- C haracteristics: What does the pain feel like? ...
- A ggravating factors: What brings on the pain? ...
- R adiating: Does the pain travel to another area or the body, or does it stay in one place?
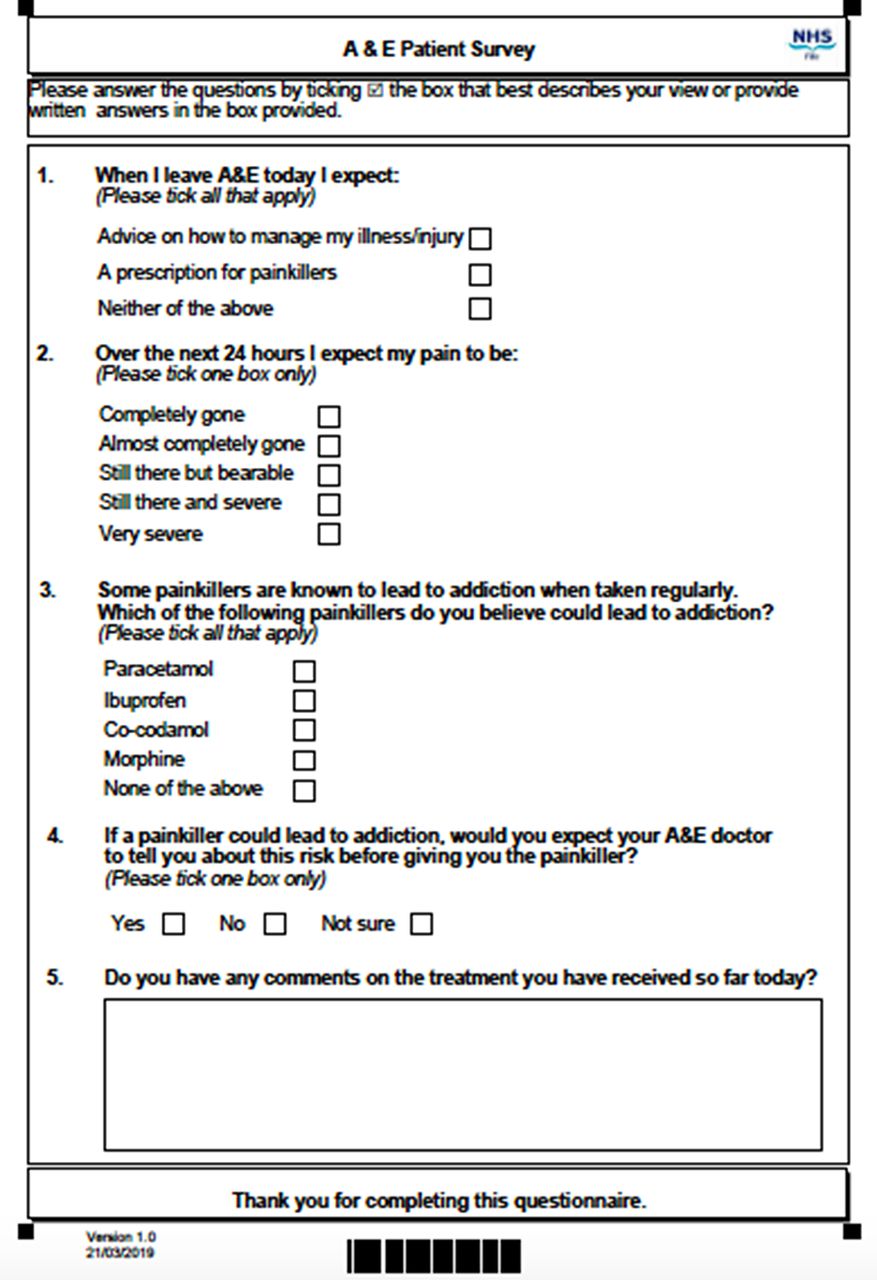
How does a nurse assess for pain?
Measuring pain Pain should be measured using an assessment tool that identifies the quantity and/or quality of one or more of the dimensions of the patients' experience of pain. This includes the: intensity of pain; intensity and associated anxiety and behaviour.
What is the most reliable way to assess a patient's pain?
Self-report is the most reliable way to assess pain intensity. When the patient is able to report pain, the patient's behavior or vital signs should never be used in lieu of self-report.
What is the most important part of a pain assessment?
The most important factor in pain assessment is the self-report of the patient. However, some patients may be reluctant to trigger the assessment so it is vital for nurses to prompt discussion of pain with patients.
What are 3 questions you can ask your patient to assess their pain?
How long have I been in pain? What am I currently doing to manage my pain? Is there anything I'm doing that's reducing my pain? What pain medications have I taken in the past, and how did they work for me?
What are the five key components of pain assessment?
The WILDA approach to pain assessment—focusing on words to describe pain, intensity, location, duration, and aggravating or alleviating factors—offers a concise template for assessment in patients with acute and chronic pain.
What tools can you use in assessing pain?
The most commonly used pain assessment tools for acute pain in clinical and research settings are the Numerical Rating Scales (NRS), Verbal Rating Scales (VRS), Visual Analog Scales (VAS), and the Faces Pain Scale-Revised (FPS-R) [9,10].
What are the nursing interventions for pain?
Nursing Interventions for Acute PainProvide measures to relieve pain before it becomes severe. ... Acknowledge and accept the client's pain. ... Provide nonpharmacologic pain management. ... Provide pharmacologic pain management as ordered. ... Manage acute pain using a multimodal approach.More items...•
Which standard method of assessing pain is the most widely used?
The most widely used tool, the NRS, asks a person to rate their pain by assigning a numerical value with zero indicating no pain and 10 representing the worst pain imaginable.
Can a nursing assistant assess pain?
Background: Nursing assistants provide most of the direct care to residents and represent the major taskforce in nursing homes. They may develop specialized knowledge of residents' pain experience that enables them to play both a pivotal role in pain assessment and possibly a supporting role in pain treatment.
Why is pain assessment important in nursing?
Accurate and reliable pain assessment is not only crucial to advocate for the patient but pain assessment also aids in determining the subsequent management and treatment strategies for the patient8.
What questions do you ask patient about pain?
Start your assessments by asking patients to rate their pain on a scale from 0 to 10, with 10 being the worst possible pain and 0 being no pain. Where are you feeling pain? When did the pain start? How long have you been in pain?
What is the Abbey Pain Scale tool?
The Abbey Pain Scale is best used as part of an overall pain management plan. The Pain Scale is an instrument designed to assist in the assessment of pain in patients who are unable to clearly articulate their needs.
What is the VAS pain scale?
The visual analog scale (VAS) is a validated, subjective measure for acute and chronic pain. Scores are recorded by making a handwritten mark on a 10-cm line that represents a continuum between “no pain” and “worst pain.”
What is Flacc pain assessment?
Abstract. Purpose: To test the validity of the Faces, Legs, Activity, Cry and Consolability (FLACC) pain assessment tool by measuring changes in scores in response to analgesics.
Is pain scale objective or subjective?
Pain is defined as a subjective experience,1 which means that it cannot be directly observed by those who are not experiencing it. Yet, clinicians and researchers rely upon observations and measures to assess and infer the pain experienced by other people.
How does pain assessment help?
This means listening empathically, believing and legitimizing the patient's pain, and understanding, to the best of his or her capability, what the patient may be experiencing. A health care professional's empathic understanding of the patient's pain experience and accompanying symptoms confirms that there is genuine interest in the patient as a person. This can influence a positive pain management outcome. After the assessment, quality pain management depends on clinicians' earnest efforts to ensure that patients have access to the best level of pain relief that can be safely provided. Clinicians most successful at this task are those who are knowledgeable, experienced, empathic, and available to respond to patient needs quickly.
Why is pain assessment important?
Pain assessment is critical to optimal pain management interventions. While pain is a highly subjective experience, its management necessitates objective standards of care. The WILDA approach to pain assessment—focusing on words to describe pain, intensity, location, duration, and aggravating or alleviating factors—offers a concise template for assessment in patients with acute and chronic pain.
What is breakthrough pain?
Breakthrough pain refers to a transitory exacerbation or flare of pain occurring in an individual who is on a regimen of analgesics for continuous stable pain (20). Patients need to be asked, “Is your pain always there, or does it come and go?” or “Do you have both chronic and breakthrough pain?” Pain descriptors, intensity, and location are important to obtain not only on breakthrough pain but on stable (continuous) pain as well.
What are some interventions that can help relieve pain?
A typical question might be, “What makes the pain better or worse?” Analgesics, nonpharmacologic approaches (massage, relaxation, music or visualization therapy, biofeedback, heat or cold), and nerve blocks are some interventions that may relieve the pain. Other factors (movement, physical therapy, activity, intravenous sticks or blood draws, mental anguish, depression, sadness, bad news) may intensify the pain.
What is the difference between chronic pain and acute pain?
According to the International Association for the Study of Pain, pain is an unpleasant sensory and emotional experience arising from actual or potential tissue damage (1). Clinically, pain is whatever the person says he or she is experiencing whenever he or she says it occurs (2). Pain is commonly categorized along a continuum of duration. Acute pain usually lasts hours, days, or weeks and is associated with tissue damage, inflammation, a surgical procedure, or a brief disease process. Acute pain serves as a warning that something is wrong. Chronic pain, in contrast, worsens and intensifies over time and persists for months, years, or a lifetime. It accompanies disease processes such as cancer, HIV/AIDS, arthritis, fibromyalgia, and diabetes. Chronic pain can also accompany an injury that has not resolved over time, such as reflex sympathetic dystrophy, low back pain, or phantom limb pain.
What are the side effects of pain assessment?
These include nausea, vomiting, constipation, sleepiness, confusion, urinary retention, and weakness. Some patients may tolerate these symptoms without aggressive treatment; others may choose to stop taking analgesics or adjuvant medications because of side effect intolerance. Adjustments, alterations, or titration may be all that is necessary.
What is visceral pain?
Visceral pain. Pain described as squeezing, pressure, cramping, distention, dull, deep, and stretching is visceral in origin . Visceral pain is manifested in patients after abdominal or thoracic surgery. It also occurs secondary to liver metastases or bowel or venous obstruction. Opioids are the treatment of choice. However, caution should be taken when using this class of drugs with patients who have bowel obstructions.
Why is pain assessment important?
An important aspect of the pain assessment is in the acknowledgment of the influence of various comorbidities and psychosocial determinants of health that impact pain . Comorbid mood disorders lead to worsening pain, and the treatment of said mood disorder improves a patient's pain. Prior history of opioid dependence, IV drug use, sexual abuse, trauma, old age, chronic diseases, and economic disparity all contribute to a patient's pain. Cultural influences on pain also play a role. [6][7][8]
How do we treat pain?
Some types of pain respond to modulating neurotransmitters or ion channels, while others are more receptive to opioid neuroreceptors.
What is a PEG score?
A chronic pain patient who experiences daily 7/10 pain is treated with both pharmacological and nonpharmacological therapies. Following treatment, their pain is 5/10. A few points might not seem like a significant difference, but if their enjoyment and quality of life, as well as function, are improving, treatment may have had a profound impact on the patient's life. The PEG tool is scored 0 to 10 for each category . The higher the score, the worse the function and uncontrolled pain.
How long does pain stay centralized?
As pain becomes chronic, over three to six months of acute pain, pain can become centralized. Centralized pain requires a lower threshold to experience pain. Decreased thresholds are problematic. Pain is an adaptive response to a painful stimulus. A lower threshold for pain subjectively means pain can be experienced from non-painful stimuli (allodynia), or mildly painful stimuli experienced can be experienced as severe pain (hyperalgesia). Centralized pain is a maladaptive form of pain.
Why do we need a fibromyalgia survey?
A fibromyalgia survey can be used to help distinguish a new pain complaint from a patient's comorbid fibromyalgia as well.
How long does pain last?
Part of the pain assessment is defining whether a patient's pain is either acute or chronic. When severe pain lasts longer than three months, it is generally considered to be chronic. Determining if the pain is acute or chronic pain is an important distinction because as pain transitions from acute to chronic, pain becomes centralized, or a function of the central nervous system rather than peripheral. Pain becomes maladaptive with hyperalgesia, and allodynia becoming more prevalent. The texture of the tissues becomes hypertonic, ropy, and cold. Pain is often more dull and achy rather than sharp.
What is the difference between 10/10 and 1/10 pain?
Often, it is necessary to prompt a patient to explain the numerical scale of pain. A 1/10 pain being a minor bump or bruise, while 10/10 pain being the worst pain they have ever experienced on par with giving birth or passing a kidney stone.[18] If a patient complains of 9/10 pain, this does not mean they automatically warrant opioid analgesia.[19] They may very well benefit from less potent analgesics tailored to treating the underlying cause.
How to find the source of pain?
Step 1: Take Extra Time. For chronic pain patients, finding the sources of their pain (locations, intensity, duration, etc.) takes considerable time. Clinicians must do the detective work necessary for these patients, despite the inclination to move difficult patients along. Step 2: Focus on the Patient, Not the Pain.
How does pain affect the patient's life?
The collateral damage caused by chronic pain can take the forms of nausea, depression, fatigue, anxiety, and other problems. Learning these aspects of patients' lives will help clinicians understand the "true dimensions" of their patients' pain (Fishman, 2007).
What is the goal of chronic pain management?
The goal of chronic pain management is to safely and effectively reduce pain and improve function and quality of life. Complete eradication of chronic pain is an unrealistic expectation and should not be a goal for the patient or the medical provider.
How long does chronic pain last?
Chronic pain refers to a pain state which is persistent, typically 3 months or more , and exists beyond an expected time for healing. The cause of the pain may not be removable or otherwise treated. It may persist despite generally accepted medical treatments.
What is chronic pain?
Chronic pain refers to a wide spectrum of diseases and conditions with causes that are multifactorial in nature. Chronic pain may include physical, psychological, social, and spiritual components, while physical pain may be further classified as either somatic, visceral, or neuropathic. Chronic pain refers to a pain state which is persistent, ...
What is the pain associated with end of life?
This type of pain may be associated with end-of-life pathology involving cancer or organ failure. Pain is a very personal and subjective experience in which a multitude of factors such as past pain experiences, expectations, social or environmental factors, and personal beliefs and values can affect perceptions of pain.
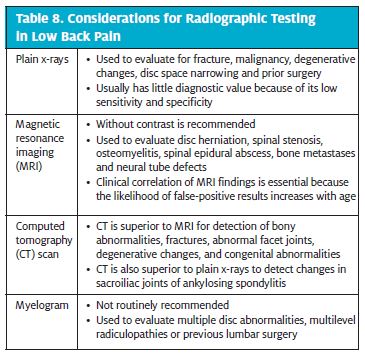
Can opium be used for back pain?
Opioids are not clinically indicated for treatment of back pain without radiculopathy, migraines, inflammatory disorders (rheumatoid arthritis or osteoarthritis), or neuropathic pain syndromes (peripheral neuropathy or fibromyalgia) and should not be prescribed for these conditions.
How to interview a patient about pain?
While interviewing a patient about pain, use open-ended questions to allow the patient to elaborate on information that further improves your understanding of their concerns. If their answers do not seem to align, continue to ask focused questions to clarify information. For example, if a patient states that “the pain is tolerable” ...
What to do if pain score exceeds comfort function goal?
If a patient’s pain score exceeds their comfort-function goal, nurses must implement an intervention and follow up within 1 hour to ensure that the intervention was successful. Using the previous example, if a patient had established a comfort-function goal of 3 to ambulate and the current pain rating was 6, the nurse would provide appropriate interventions, such as medication, application of cold packs, or relaxation measures. Documentation of the comfort-function goal, pain level, interventions, and follow-up are key to effective, individualized pain management. [10]
How to use the Faces scale?
The FACES scale is a visual tool for assessing pain with children and others who cannot quantify the severity of their pain on a scale of 0 to 10. See Figure 11.5 [2] for the FACES Pain Rating Scale. To use this scale, use the following evidence-based instructions. Explain to the patient that each face represents a person who has no pain (hurt), some pain, or a lot of pain. “Face 0 doesn’t hurt at all. Face 2 hurts just a little. Face 4 hurts a little more. Face 6 hurts even more. Face 8 hurts a whole lot. Face 10 hurts as much as you can imagine, although you don’t have to be crying to have this worst pain.” Ask the person to choose the face that best represents the pain they are feeling. [3]
What are some pain characteristics?
Note: You can provide suggestions for pain characteristics such as “aching,” “stabbing,” or “burning.”
What is the pain scale?
Asking a patient to rate the severity of their pain on a scale from 0 to 10, with “0” being no pain and “10” being the worst pain imaginable is a common question used to screen patients for pain. However, according to The Joint Commission requirements described earlier, this question can be used to initially screen a patient for pain, but a thorough pain assessment is required. Additionally, the patient’s comfort-function goal must be assessed. The comfort-function goal provides the basis for the patient’s individualized pain treatment plan and is used to evaluate the effectiveness of interventions.
What is an alternative mnemonic to use when assessing pain?
An alternative mnemonic to use when assessing pain is “OLDCARTES.”
What is comfort scale?
The COMFORT Behavioral Scale is a behavioral-observation tool validated for use in children of all ages who are receiving mechanical ventilation. Eight physiological and behavioral indicators are scored on a scale of 1 to 5 to assess pain and sedation. [6]
Why is pain assessment important?
Pain assessment is crucial if pain management is to be effective. Nurses are in a unique position to assess pain as they have the most contact with the child and their family in hospital. Pain is the most common symptom children experience in hospital. Acute pain (noiciception) is associated with tissue damage and an inflammatory response, ...
What is pain measurement?
Pain measurement quantifies pain intensity and enables the nurse to determine the efficacy of interventions aimed at reducing pain.
How often should pain and sedation be documented?
Children on complex analgesia such as intravenous opioid and/ or ketamine, epidurals or regional analgesia should have hourly pain and sedation scores documented.
What are the challenges of assessing paediatric pain?
There are challenges in assessing paediatric pain, none more so than in the pre-verbal and developmentally disabled child. Therefore physiological and behavioural tools are used in place of the self-report of pain.
Can blood pressure be measured in isolation?
blood pressure may increase. oxygen saturation may decrease. Physiological indicators in isolation cannot be used as a measurement for pain. A tool that incorporates physical, behavioural and self report is preferred when possible.
When to assess pain?
It is crucial to assess pain when at rest as well as when the patient is mobile. You also need to evaluate pain when the patient is on pain relievers to know how pain is reacting and responding to the medications. Consult the caregiver and parents in situations where you are dealing with children and cognitively impaired patients.
What is pain assessment?
Herein, pain assessment is the process of objectively understanding the state and condition of pain by observing the patient and measuring the intensity of the pain. The assessment is a broad concept that involves clinical judgment which is grounded in observation, uniqueness, and context of the individual experience with the pain.
What is pain measurement tool?
Pain measurement tools are the equipment used to aid nurses in carrying out their pain assessment process.
Why is pain assessment important?
Accurate pain assessment is vital for the development of effective pain management. Pain is a nervous system triggered feeling usually associated with the physical disorder such as illness or injuries. Pain is a common symptom that children and older people experience. Nurses are in a position to assess pain in patients mostly children ...
What is pain in nursing?
Pain is a common symptom that children and older people experience. Nurses are in a position to assess pain in patients mostly children and older people exclusively owing to their relationship and interaction with the patients. Pain is multi-dimensional and subjective making its assessment challenging at times.
What is the term for pain caused by the central nervous system?
2. Neuropathic pain. Neuropathic Pain arises when the reporting system (nervous system), central or peripheral is damaged either from diseases, injury, etc. Multiple sclerosis, chemotherapy, and phantom pain are some of the conditions that may damage neurons leading to neuropathic pain.
What are the two types of pain?
Types of pain. There are two basic pain types. Nociceptive Pain. Nociceptive Pain arises from a wide range of tissue related trouble that is reported to the brain by the nervous system. This pain typically changes with movement, load, and position.
Assessment
Diagnosis
- The first step in assessing pain is to find out how bad it is at the present moment. There are tools that can help someone who is able to communicate describe the severity of their pain. For adults, this is usually done with a numeric scale of 0-10. Zero would describe the absence of pain and ten would symbolize the worst pain imaginable. In genera...
Components
- There are a number of different pain rating scales which can be used to make this process easier. For example, one scale referred to as the FLACC scale uses a description of several signs the person may be demonstrating, in order to estimate a number between one and ten. These include facial appearance, legs (whether relaxed, tense, or kicking), activity (whether lying quietly, squir…
Results
- Everyone will have their own acceptable level of pain. For some it may be no pain and others will tolerate a pain level of 3 on a scale of 0-10. It is important to find out what the acceptable level is for the individual you are caring for. If your loved one is happy at a pain level of 3, you wouldnt want to medicate them to the point of sedation to get them at a zero level of pain. On the other h…
Symptoms
- As mentioned earlier, it can be difficult to assess someones pain if they are unable to verbalize it and/or unable to point to the FACES scale. There are some signs and symptoms that a person may exhibit if they are in pain that can clue you in: The more symptoms a person has, and the more intense they appear to be, the more you will get a grasp of the degree of pain they are expe…
Treatment
- One of the most important things you can do for the person you are caring for is to keep an accurate record of their pain and their pain treatments. Once you assess their pain, record the severity and location and any medications or treatments that you give them. Take note whether the medications or treatments were effective. Also, write down anything new they may have tol…
Quotes
- As a final note, caring for a loved one with a life-threatening illness is perhaps the greatest thing you can do for another human being, but it is also very draining. As much as you can, remember to care for your own needs. Ask for help and be willing to receive it. Pamper yourself, if only for a few minutes here and there. You may feel guilty trying to meet your own needs. But remember that y…