
- Complete blood count (CBC): This test measures your platelet count and the number of other blood cells in your blood.
- Blood smear: For this test, some of your blood is put on a slide. ...
- Bone marrow tests: These tests check whether your bone marrow is healthy.
What s the best treatment to get rid of ITP?
- Oral: Oral medications have been proven effective, but they take time to work. ...
- Topical: Topical treatments (like amorolfine and ciclopirox) can help with minor toenail fungus. ...
- Natural/Homeopathic: Natural preventative measures can be effective, but once fungus sets in, your best bet is a research-backed and FDA approved oral antifungal. ...
What is the optimal treatment of ITP?
Which treatments are available for ITP?
- Corticosteroids. Corticosteroids have been used as a first-line treatment for ITP for more than 30 years, according to available research from 2016.
- Thrombopoietin receptor antagonists. ...
- Antibody therapy. ...
- Immunoglobulin infusions. ...
- Avoiding certain medications and supplements. ...
- Splenectomy. ...
- Antibiotics. ...
- Lifestyle changes. ...
Is ITP considered cancer?
Immune thrombocytopenia (ITP) is not cancer, although some confuse it with blood cancer (leukemia). Learn about symptoms, causes, and treatment. Read more: Is ITP Considered Cancer? Article Some blood disorders are forms of cancer. Others are benign.
How serious is ITP?
While ITP may sound worrying to parents, the risk of any serious complication from ITP is very low. In most children the condition will settle down quite quickly – often without needing any treatment. The platelet count is often up to safe levels within a week or two, but it may take longer to fully return to normal.
Does ITP show up in blood tests?
Diagnostic Procedures for ITP Includes a special blood test called an "anti-platelet antibody test." Careful review of medications. Bone marrow aspiration: This test examines the platelet production and can rule out any abnormal cells the marrow may be producing that could lower platelet counts.
What can ITP be mistaken for?
Hepatitis C+ Of the liver diseases, hepatitis C is most often associated with low platelets and mistaken for ITP.
At what platelet count do you treat ITP?
Treatment is considered for patients who have: A platelet count less than 30,000. An upcoming operation or procedure that requires them to have a higher platelet count. Active bleeding with a known diagnosis of ITP.
Is ITP a terminal illness?
Yes, ITP can potentially be fatal. However, that could be said for virtually every disease, including many which are usually not very serious. Extremely rare but fatal complications can occur from strep throats, the common cold (which may lead to pneumonia), chickenpox, or what seems to be a mild case of indigestion.
What cancers cause ITP?
Immune Thrombocytopenic Purpura (ITP) is in rare cases secondary to solid tumors, particularly breast cancer. In these cases, the clinical course of the ITP may follow the clinical course of the primary tumor, and remission of the ITP may be induced by treatment of the primary tumor.
Can ITP resolve itself?
Acute ITP in children often goes away on its own within a few weeks or months and does not return. For a small number of children, ITP does not go away on its own, and the child may need treatment. Chronic ITP varies from person to person and can last for many years.
What are 3 causes of thrombocytopenia?
Factors that can decrease platelet production include:Leukemia and other cancers.Some types of anemia.Viral infections, such as hepatitis C or HIV.Chemotherapy drugs and radiation therapy.Heavy alcohol consumption.
What is the first line treatment for ITP?
The standard initial treatment for ITP is oral corticosteroids to increase platelet counts. Intravenous immunoglobulin or anti-D immunoglobulin can also increase platelet counts and are particularly useful for stimulating rapid platelet increases before planned procedures.
What are 3 causes of thrombocytopenia?
Factors that can decrease platelet production include:Leukemia and other cancers.Some types of anemia.Viral infections, such as hepatitis C or HIV.Chemotherapy drugs and radiation therapy.Heavy alcohol consumption.
What is the most common cause of low platelet count?
Autoimmune diseases: Autoimmune diseases, like immune thrombocytopenia (ITP), lupus and rheumatoid arthritis, that attack your immune system may destroy platelets. Blood cancers: Leukemia and lymphoma may damage your bone marrow and affect its ability to make enough blood cells, including platelets.
What cancers cause low platelets?
Certain cancers such as leukemia or lymphoma can lower your platelet count. The abnormal cells in these cancers can crowd out healthy cells in the bone marrow, where platelets are made.
What infections cause low platelets?
Infections with protozoa, bacteria and viruses can cause thrombocytopenia with or without disseminated intravascular coagulation. Commonly dengue, malaria, scrub typhus and other rickettsial infections, meningococci, leptospira and certain viral infections present as fever with thrombocytopenia.
What is the blood test for ITP?
There are a variety of tests that may be ordered by the healthcare provider when evaluating ITP or its cause. These include: Complete blood count (CBC): A CBC is a blood test that measures the number of white blood cells, red blood cells, and platelets in the blood. This test also measures the size of the blood cell types.
What is the physical exam for ITP?
Physical Examination. When being evaluated by a medical professional for ITP, exams may include: 2. A skin check, looking for any evidence of bleeding, such as bruises or petechiae. Inspection of the mouth and gums, looking for bleeding or blood blisters.
What is ITP in labs?
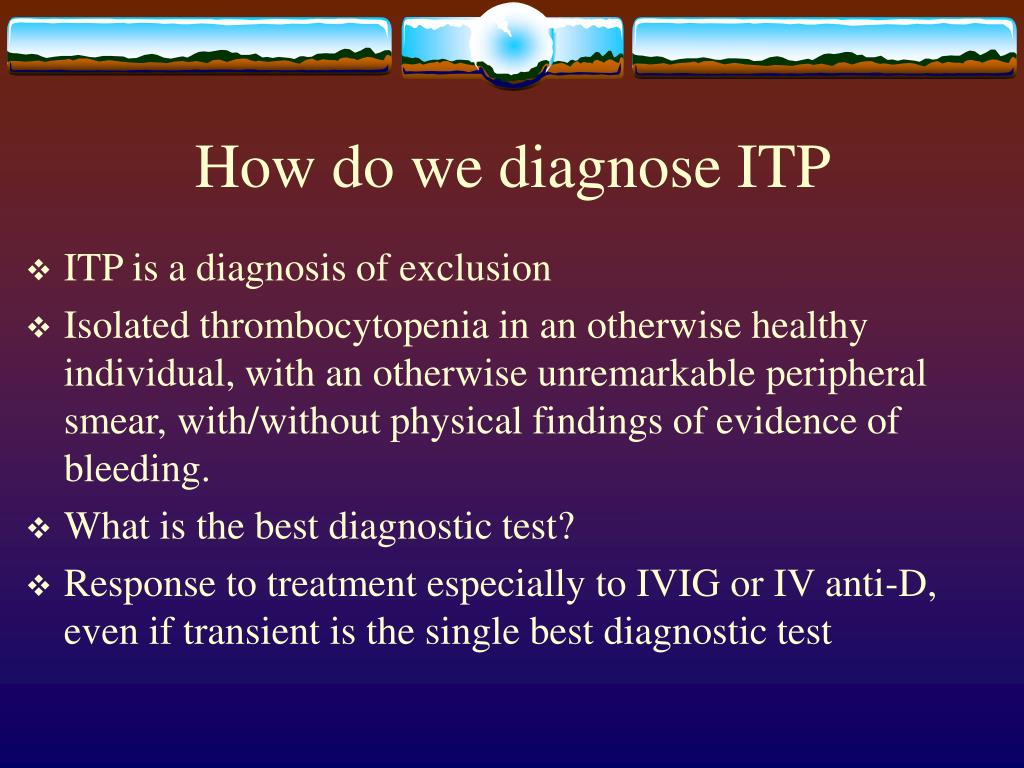
Labs and Tests. Imaging. Differential Diagnosis. Immune thrombocytopenia (ITP) is a diagnosis made when the immune system destroys platelets inappropriately, resulting in low platelet counts in the blood. It is often considered a diagnosis of exclusion—when other testing to determine the cause of the low platelets has not shown any specific cause. ...
What is the diagnosis of low platelet count?
Immune thrombocytopenia (ITP) is a diagnosis made when the immune system destroys platelets inappropria tely, resulting in low platelet counts in the blood. There are various methods of diagnosis for ITP.
How to determine platelet size?
Blood smear: In a blood smear, a sample of blood is taken and placed on a slide. This slide is then evaluated under the microscope. The platelets can be evaluated for the proper size and appearance. This visualization also ensures there is no platelet clumping. With platelet clumping, the platelets stick to each other, making them appear low in the blood circulation when they are actually normal in number. 3
What is the drug that causes thrombocytopenia?
This can happen with a variety of medications, most commonly a medication called heparin. Other medications with this risk include penicillin, nonsteroidal anti-inflammatory medications, quinine, sulfa medications, and statin medications. 7
What is the best way to see the abdomen?
Imaging of the abdomen with a computed tomography (CT) scan, magnetic resonance imaging (MRI), or ultrasound can evaluate the abdominal organs of the liver and spleen.
Diagnosing ITP
We begin the diagnosis by taking your complete medical history and performing a physical examination. Make sure to tell us about all of you (or your child's) symptoms.
ITP Treatment
Once we confirm a diagnosis, we will discuss the treatment plan with you. Learn about ITP treatment options at Stanford.
Why is it difficult to diagnose ITP?
The difficulty in establishing an accurate diagnosis of ITP has implications for the management of ITP because patients can be exposed to treatment-related toxicities without achieving a platelet count response and because of the generalizability of results from clinical trials.
What is the most common method used to detect platelet autoantibodies in ITP?
Moore, D.M.A., J.G.K., I. Nazy, manuscript submitted, August 2018). We found that the MAIPA and ELISA are the most common methods used to detect platelet GPIIb/IIIa and/or GPIb/IX-specific autoantibodies in ITP among various laboratories. Our systematic review included the results from glycoprotein-specific platelet autoantibody testing in 1170 ITP patients, and 225 non-immune thrombocytopenic controls. We found that the pooled estimates for the sensitivity of glycoprotein-specific autoantibody detection assays were low (<50%), whereas the specificity estimates were higher (>90%). The specificity estimates did not include the results from healthy controls. We also found that direct assays have a better sensitivity than indirect assays. Together, these results suggest that serological investigations for ITP have a high specificity but low sensitivity, meaning that these assays are useful for ruling in, but not for ruling out ITP. This is in contrast to the results found in patients with suspected AIHA, in which the sensitivity and specificity are both high. Our interpretation for the low sensitivity yet high specificity in ITP is that either: (1) a proportion of ITP patients have autoantibodies against other non-platelet target antigens such as thrombopoietin or its receptor c-Mpl, 47 (2) the autoantibodies are undetectable in some patients (because of low titer or sequestration), or (3) other pathological immune mechanisms exist that are independent of platelet autoantibodies, such as cytotoxic T cells. 48 These results suggest that ITP is a heterogenous group of disorders caused by multiple mechanisms including, but not limited to, anti-platelet autoantibodies.
How to detect autoantibodies in plasma?
The MAIPA assay can detect autoantibodies directly on the platelet surface or indirectly in the plasma. In the first step of MAIPA, a plate is coated with anti-murine antibody. In the direct assay, a patient’s platelet lysate containing the glycoprotein bound by the suspected autoantibody is mixed with an anti-platelet monoclonal antibody. For indirect MAIPA, normal platelets are mixed with patient test plasma to allow the autoantibody to bind. In the third step, the presence of an autoantibody is detected with a labeled anti-human antibody. The ELISA is an indirect assay in which a plate is coated with platelet glycoprotein followed by the patient test plasma sample. As in the MAIPA, the presence of an autoantibody is detected with a labeled anti-human antibody. The Immunobead assay can be indirect or direct, and it is a type of antigen capture assay similar to the MAIPA; the difference is that the glycoprotein is captured on the well by an anti-platelet monoclonal antibody conjugated to a bead.
What is the diagnosis of AIHA?
Today, these laboratory tests are essential in making the diagnosis of AIHA. 2. AIHA is characterized by a reduction in the red cell number (anemia) and evidence of increased red cell destruction, including an elevated bilirubin, and elevated red cell lactate dehydrogenase.
Is ITP a diagnosis of exclusion?
Hematologists quickly discovered that there was no parallel DAT test for platelets; therefore, ITP became a diagnosis of exclusion. 7 But the weakness of such a tautological approach for the diagnosis of ITP is the challenge of confirming a negative. Consequently, over the past decades, several working groups have attempted to further refine the diagnosis. The designation of “ITP” continues to be used, although the previous designation of “idiopathic” has been replaced by immune, and “purpura” is no longer used, recognizing that many patients do not have any bleeding symptoms. 8-10 ITP can be defined as a platelet count <100 × 10 9 /L with other causes of thrombocytopenia excluded. ITP is further differentiated into primary ITP or secondary ITP, which indicates immune-mediated thrombocytopenia associated with a variety of disorders such as chronic viral infections or autoimmune rheumatological disorders such as systemic lupus erythematosus. That differentiation is important because many of the treatments of secondary ITP target the underlying disorder. Primary ITP is separated into newly diagnosed (<3 months from diagnosis), persistent (3-12 months from diagnosis), or chronic (>12 months since diagnosis). 8
Is thrombocytopenia a hematological presentation?
Thrombocytopenia is a common hematological presentation with a variety of potential causes. Establishing the diagnosis can be difficult, and the correct identification of the underlying cause is important to make appropriate management decisions for thrombocytopenic patients. 11, 12 In a recent study based on data from the McMaster ITP Registry, 1 in 7 patients diagnosed with primary ITP at presentation or on follow-up were reclassified as additional investigations were performed ( Table 1 ). These patients were usually male, with a milder thrombocytopenia and a fewer number of severe bleeding episodes. 13
Is ITP a clinical expression?
This suggests several possibilities: (1) the ideal test for ITP has yet to be developed, (2) current test methods need to be improved, or (3) ITP is the clinical expression of a variety of thro mbocytopenic disorders with different underlying mechanisms.
Why is ITP also called ITP?
The body recognizes any cells with antibodies as foreign cells and destroys them. That is why ITP is also referred to as immune thrombocytopenic purpura.
What is idiopathic thrombocytopenic purpura (ITP)?
Idiopathic thrombocytopenic purpura is a blood disorder characterized by an abnormal decrease in the number of platelets in the blood. Platelets are cells in the blood that help stop bleeding. A decrease in platelets can result in easy bruising, bleeding gums and internal bleeding.
How long do ITP platelets live?
ITP platelets usually survive only a few hours, in comparison to normal platelets which have a lifespan of 7 to 10 days. Platelets are essential for the formation of a blood clot. Blood clots consist of a mass of fibers and blood cells.
How long does it take for an ITP to heal?
Many children with ITP are able to spontaneously recover in about 2 to 4 days.
How many children have ITP?
ITP affects approximately four to eight per 100,000 children under the age of 15 each year in the U.S. There are two forms of ITP: Acute thrombocytopenic purpura — This is most commonly seen in young children (2 to 6 years old). The symptoms may follow a viral illness, such as chickenpox.
What is the normal platelet count for a child with ITP?
Normal platelet count is in the range of 150,000 to 450,000. In a child with ITP, the platelet count is generally less than 100,000. By the time significant bleeding occurs, the child may have a platelet count of less than 10,000. The lower the platelet count, the greater the risk of bleeding.
What is the red spot on my head?
Petechia - tiny red dots under the skin that are a result of very small bleeds. Nosebleeds. Bleeding in the mouth and/or in and around the gums. Blood in the vomit, urine or stool. Bleeding in the head - this is the most dangerous symptom of ITP.
What is ITP in blood?
What is ITP? Idiopathic thrombocytopenic purpura is an immune disorder in which the blood doesn’t clot normally. This condition is now more commonly referred to as immune thrombocytopenia (ITP). ITP can cause excessive bruising and bleeding. An unusually low level of platelets, or thrombocytes, in the blood results in ITP.
Why is ITP called idiopathic?
The term “idiopathic,” used in the former name of the condition, means “of unknown cause.” In the past, it was used because the cause of ITP wasn’t well understood . However, it’s now clear that the immune system plays an important role in the development of ITP, thus its newer name, immune thrombocytopenia.
How long does it take for ITP to heal?
In some cases, treatment isn’t needed. For example, children that develop the acute form of ITP usually recover within six months or less without any treatment. Adults with less severe cases of ITP may also not require treatment.
How long does ITP last?
Acute ITP is the most common form of the disorder in children. It usually lasts less than six months. Chronic ITP lasts six months or longer. It’s most commonly seen in adults, although teenagers and younger children can also be affected.
Can Petechiae be a rash?
Petechiae often look like a rash. ITP can occur in both children and adults. There appears to be differences at certain ages between women and men and the development of ITP. At younger ages, ITP may be more common in women. At older ages, it may be more common in men.
Does the immune system affect platelets?
The immune system also appears to interfere with cells responsible for normal platelet production, which can further lower the number of platelets in the blood stream. In children, ITP often develops acutely following a virus. In adults, ITP usually develops over time.
What are the symptoms of ITP?
ping. pong. Also, if you ride a bike, a helmet is a necessity when you have ITP. ITP may cause bruises (purpura) and small, scattered rash-like bruising (petechiae) to spontaneously appear on your skin. You might see these symptoms even if you don’t participate in contact sports.
What to do after ITP diagnosis?
After an ITP diagnosis, talk to your doctor if you drink alcohol. They will likely recommend you stop drinking — at least until your platelet counts normalize.
What to do if ITP is severe?
If your ITP is severe and your platelet count is extremely low, your doctor may recommend that you do make some changes. You might even find the changes helpful in symptom management. Read on to learn more about some of the lifestyle changes you might need to make following an ITP diagnosis. Be sure to talk with your doctor about any lifestyle ...
What is the best diet for ITP?
Your diet can play a role in your ITP treatment plan. A healthy, balanced diet is important for all adults. But when you have ITP, eating the right foods can help you feel better and more energetic. Certain nutrients, such as vitamin K and calcium, have natural components important to blood clotting.
How to boost immune system in ITP?
Vitamin D supplementation may also have a role in boosting the immune system in ITP, especially if vitamin D levels are low. You may also consider other dietary measures: Eat organic foods when possible. Swap saturated (animal) and trans (man-made) fats for plant-based versions, such as avocados. Limit red meats.
Can ITP be a long term health condition?
An ITP diagnosis doesn’t mean you can’t exercise or stay active. Regular exercise is beneficial for long-term health for everyone. However, you may need to adjust the types of activities you participate in.
What is an ITP?
Immune thrombocytopenic purpura (ITP) is an autoimmune pathology characterized by a low platelet count, purpura, and hemorrhagic episodes caused by antiplatelet autoantibodies.
What is the ITP of a spleen?
Immune thrombocytopenic purpura ( ITP) is an autoimmune pathology characterized by a low platelet count, purpura, and hemorrhagic episodes caused by antiplatelet autoantibodies. The diagnosis is typically made by the exclusion of the known causes of thrombocytopenia. IgG autoantibodies sensitize the circulating platelets. It leads to accelerated removal of these cells by antigen-presenting cells (macrophages) of the spleen, and sometimes the liver or other components of the monocyte-macrophage system. Bone marrow compensates the platelet destruction by increasing platelet production. ITP most often occurs in healthy children and young adults within a few weeks following a viral infection. Certain drugs can also cause immune thrombocytopenia indistinguishable from ITP. Most children have spontaneous remission within a few weeks or months, and splenectomy is rarely needed. However, young adults rarely have spontaneous remissions necessitating splenectomy within the first few months after diagnosis. According to current evidence, this activity will review the most common causes of ITP and outline an interprofessional treatment approach.
How long does it take for ITP to go away?
ITP most often occurs in healthy children and young adults within a few weeks following a viral infection. Certain drugs can also cause immune thrombocytopenia indistinguishable from ITP. Most children have spontaneous remission within a few weeks or months, and splenectomy is rarely needed.
What is the difference between acute and chronic ITP?
Immune thrombocytopenic purpura can be divided into two classifications; acute and chronic. The acute form presents in childhood, affects both sexes, and may be prefaced by a viral infection. Most children (85%) have a benign course and do not require treatment. They can spontaneously recover within three months. The chronic form affects individuals between ages 20-50 years; there is a female/male ratio of 3 to 1, and It is usually not preceded by a viral infection. It may present with bleeding episodes for months or years; during that time, the platelet counts are close to normal. Fewer than 10% of children develop chronic ITP.
How long does it take for a child to get thrombocytopenic purpura?
Childhood immune thrombocytopenic purpura often occurs within a few weeks following a viral infection, suggesting a possible cross-immunization between viral and platelet antigens, the absorption of immune complexes, or a hapten mechanism.
What is purpura in children?
Acute immune thrombocytopenic purpura can be characterized by generalized purpura in a previously healthy child or, less commonly in an adult, bruises following minor trauma, the presence of oral hemorrhagic bullae, epistaxis, gastrointestinal bleeding, conjunctival hemorrhage, and hematuria.
What age group is most likely to have thrombocytopenic purpura?
HIV-associated disease is now the most common cause of thrombocytopenic purpura, especially in males between 20 and 50 years of age . Testing for HIV antibodies is a critical part of the assessment of ITP. [4][5]
How long does it take for ITP to go away?
There are two forms of ITP: Acute thrombocytopenic purpura. This usually affects young children, ages 2 to 6 years old. The symptoms may follow a viral illness, such as chickenpox. Acute ITP usually starts suddenly and the symptoms usually disappear in less than 6 months, often within a few weeks.
How is idiopathic thrombocytopenic purpura treated?
Specific treatment for idiopathic thrombocytopenic purpura will be determined by your health care provider based on:
What is immune thrombocytopenic purpura?
Immune thrombocytopenic purpura (ITP) is a blood disorder characterized by a decrease in the number of platelets in the blood. Platelets are cells in the blood that help stop bleeding. A decrease in platelets can cause easy bruising, bleeding gums, and internal bleeding. This disease is caused by an immune reaction against one's own platelets. It has also been called autoimmune thrombocytopenic purpura.
What causes idiopathic thrombocytopenic purpura?
In ITP, the immune system is stimulated to attack your body's own platelets. Most often this is a result of antibody production against platelets. In a small number of cases, a type of white blood cell called T-cells will directly attack platelets. This immune system error may be a result of any of the following:
What is the difference between purpura and thrombocytopenia?
Thrombocytopenia means a decreased number of platelets in the blood. Purpura refers to the purple discoloring of the skin, as with a bruise. ITP is a fairly common blood disorder that both children and adults can develop. There are two forms of ITP: Acute thrombocytopenic purpura.
What is the normal platelet count for thrombocytopenic purpura?
What are the symptoms of idiopathic thrombocytopenic purpura? Normal platelet count is in the range of 150,000 to 450,000. With ITP, the platelet count is less than 100,000. By the time significant bleeding occurs, you may have a platelet count of less than 10,000.
How long does thrombocytopenic purpura last?
Chronic thrombocytopenic purpura. The onset of the disorder can happen at any age, and the symptoms can last a minimum of 6 months, several years , or a lifetime. Adults have this form more often than children do, but it does affect adolescents. Females have it more often than males.
Self-Checks/At-Home Testing
Physical Examination
- When being evaluated by a medical professional for ITP, exams may include:2 1. A skin check, looking for any evidence of bleeding, such as bruises or petechiae 2. Inspection of the mouth and gums, looking for bleeding or blood blisters 3. Examination of the abdomen to feel for the size of the spleen, as sometimes the spleen is enlarged in ITP
Labs and Tests
- There are a variety of tests that may be ordered by the healthcare provider when evaluating ITP or its cause. These include: 1. Complete blood count (CBC): A CBC is a blood test that measures the number of white blood cells, red blood cells, and platelets in the blood. This test also measures the size of the blood cell types. Thrombocytopenia is diagnosed when the platelet levels are low…
Imaging
- Imaging of the abdomen with a computed tomography (CT) scan, magnetic resonance imaging (MRI), or ultrasound can evaluate the abdominal organs of the liver and spleen. Sometimes dysfunction in these organs can lead to the development of low platelets. If there is any abnormality of the liver or spleen, this likely is causing the low platelets, not ITP.5
Differential Diagnosis
- A finding of low platelets may be caused by other illnesses or conditions other than ITP, including: 1. TTP (thrombotic thrombocytopenic purpura):Low platelets can be found in TTP, but for a different reason than ITP. In TTP, there is not enough activity by a protein called ADAMTS13. This leads to too many clots forming in the blood, and the circulating platelets are low because they …
Summary
- Immune thrombocytopenia (ITP) is a diagnosis made when the immune system destroys plateletsinappropriately, resulting in low platelet counts in the blood. There are various methods of diagnosis for ITP.
A Word from Verywell
- Be sure to speak to your healthcare team if you are concerned about the development of ITP, or if you are concerned that you may have low platelets. Testing may be done that can help determine the cause of the low platelets as well as a treatment plan. Also be sure to seek medical care emergently if you have ITP or any other platelet disorder and you are experiencing bleeding.