When should I use an insulin sliding scale?
Using Your Sliding Scale. A sliding scale is what you will use to determine how much insulin you need to give to correct an elevated blood sugar and/or for food. There are two parts. Correction factor and insulin to carb ratio. In our example, the correction factor is half a unit will lower the blood sugar 25 points, and the insulin to carb ratio is half a unit will cover 10 grams of carbs.
Which insulins are used for sliding scale?
common sliding scale regimens: long-acting insulin (glargine/detemir or nph), once or twice a day with short acting insulin (aspart, glulisine, lispro, regular) before meals and at bedtime long-acting insulin (glargine/detemir or nph), given once a day regular and nph, given twice a day pre-mixed, or short-acting insulin analogs or regular and …
What is an insulin sliding scale andHow does it work?
- Sliding scale insulin therapy uses your pre-meal blood sugar level to determine insulin dosage.
- Research indicates sliding scale insulin therapy is ineffective at managing blood sugar levels.
- Therefore, try an alternative method like insulin pumps or once-weekly injections.
- Visit Insider's Health Reference library for more advice.
How to calculate a sliding scale?
A sliding scale is a term in economics used to describe a scale where prices, taxes or wages change based on another factor such as gross sales, a cost-of-living index or income level. Under a sliding scale, you can manually calculate the prices, taxes or wages paid or received based on information about the sliding ...
See more
What is a typical sliding scale for insulin?
70-139 mg/dL - 0 units 140-180 mg/dL - 4 units subcut 181-240 mg/dL - 6 units subcut 241-300 mg/dL - 8 units subcut 301-350 mg/dL - 10 units subcut 351-400 mg/dL - 12 units subcut If blood glucose is greater than 400 mg/dL, administer 14 units subcut, notify provider, and repeat POC blood sugar check in 1 hour.
How do I calculate how much insulin to take?
For short-acting insulin, use the “1800 rule.” This tells you how much your blood sugar will drop for each unit of short-acting insulin. For example, if you take 30 units of short-acting insulin daily, divide 1800 by 30.
How much insulin should I take if my blood sugar is 200?
Your Insulin TherapyBlood sugar levelSupplemental insulin doseHigher than 200 mg per dLAdd 2 units of insulin150 to 200 mg per dLAdd 1 unit of insulin100 to 149 mg per dlNo change70 to 100 mg per dLSubtract 1 unit of insulin1 more row•Aug 1, 2004
How much insulin should I take if my blood sugar is 400?
Theoretically, to reduce 400 mg/dL blood sugar to about 100 mg/dL, you would need at least 10 units of insulin. However, depending on your weight and other factors, a higher dose of insulin is almost always required.
What is sliding scale therapy?
Sliding scale therapy approximates daily insulin requirements. The term "sliding scale" refers to the progressive increase in pre-meal or nighttime insulin doses. The term “sliding scale” refers to the progressive increase in the pre-meal or nighttime insulin dose , based on pre-defined blood glucose ranges.
Why is sliding scale not effective?
Sliding scales are less effective in covering a pre-meal high blood sugar, because the high blood glucose correction and food bolus cannot be split.
Does insulin change at bedtime?
The amount of carbohydrate to be eaten at each meal is pre-set. The basal (background) insulin dose doesn’t change. You take the same long-acting insulin dose no matter what the blood glucose level. The bolus insulin is based on the blood sugar level before the meal or at bedtime.
Is sliding scale easier than a sliding scale?
The sliding scale method may seem easier, because there are fewer calculations. However, to be successful, it requires a strict adherence to a consistent schedule of meals and activity, and following your prescribed diet. Eat the pre-assigned amount of carbohydrate for each meal, and at a similar time of the day.
Can you use a sliding scale for a bedtime snack?
Points To Remember! Sliding scale regimens may include a bedtime high blood sugar correction. As the nighttime scale only considers the amount of insulin required to drop your blood sugar level back into the target range, it should not be used to cover a bedtime snack.
What is a sliding scale?
The sliding scale is one way of working out how much insulin to take before each meal. Doctors developed it several decades ago as a guide to insulin dosage, but few healthcare professionals now use it. warn that using only sliding scale insulin for treatment is ineffective for most people.
How to calculate insulin dose?
To calculate the dose, the person should divide the number of grams of carb in the meal by the grams of carbs that one unit of insulin breaks down. Correctional insulin: To form a complete mealtime dose, the person will need to combine a correctional insulin value with the nutritional insulin value.
Why do people need to eat the same number of carbs on a sliding scale?
Carbohydrates: The person must consume the same number of carbs with each meal because the chart’s calculations depend on a single carb value. This number should not change from day to day.
What is intensive insulin therapy?
Intensive insulin therapy involves three types of insulin dose. Another name for this method is basal-bolus therapy, or tight control. The person must make daily calculations to keep their glucose levels as close to their target level as they can.
How does insulin travel?
The person will wear the pump on their body. The insulin travels from the pump, through a small tube and needle, into the body. The individual will need to work with their doctor to program the pump and to work out which doses they need. They may still need to inject insulin at mealtimes or after exercising.
Where is the insulin on the chart?
Insulin dosage will vary, depending on two factors: Pre-meal blood glucose level: This usually appears on the left-hand side on the chart, from low to high, with higher doses of insulin toward the bottom of the chart. The more blood sugar a person has, the more insulin they will need to deal with it.
Can sliding scales cause low blood sugar?
Low blood sugar. The doses that a sliding scale chart requires might also be excessive if a person skips meals or is more sensitive to insulin on a given day. As these doses build up throughout the day, they could lead to a dangerous drop in blood glucose levels.
What does sliding scale insulin do?
Sliding scale doses are typically taken just prior to meal time, and sometimes at bedtime, to correct for elevated blood sugar. The type of insulin used on a sliding scale is often regular or fast-acting, but there are different sliding scale regimens - using a variety of insulin - to address different diabetic needs.
Does sliding scale therapy work?
It is easy to see why sliding scale therapy can only work well when the user has a generally predictable lifestyle. Although there are many variations of sliding scale regimen, each one needs to be followed consistently. Source: Dibetes Teaching Center, Washington DSHS. Photo: Pexels.
Does sliding scale include bedtime correction?
Sliding scale users must keep the following in mind. A sliding scale prescription may include a bedtime correction dose. This amount is only what is required to get the blood sugar back to target level and does not cover any additional carbs from a non-prescribed bedtime snack.
Should you eat the same amount of carbs on a sliding scale?
When using a sliding scale it is important to eat the same amount of carbohydrate at every meal. Although the foods can change, the time and carb count of the meal should always be constant. The timing, type, and duration of your physical activity or exercise should be, as much as possible, the same each day.
What is sliding scale therapy?
Sliding scale therapy approximates daily insulin requirements. The term "sliding scale" refers to the progressive increase in pre-meal or nighttime insulin doses. The term “sliding scale” refers to the progressive increase in the pre-meal or nighttime insulin dose , based on pre-defined blood glucose ranges.
What is the transition from IV to SQ insulin?
This review article suggests a stepwise approach to the transition in order to promote safety and euglycemia. Important components of the transition include evaluating the patient and clinical situation for appropriateness, recognizing factors that influence a safe transition, calculation of proper SQ insulin doses, and deciding the appropriate type of SQ insulin. This article addresses other clinical situations including the management of patients previously on insulin pumps and recommendations for patients requiring glucocorticoids and enteral tube feedings. The use of institutional and computerized protocols is discussed. Further research is needed regarding the transition management of subgroups of patients such as those with type 1 diabetes and end-stage renal disease. Introduction Intravenous (IV) insulin is used in the hospitalized patient to control blood sugars for patients with and without diabetes who may exhibit uncontrolled hyperglycemia or for those who need close glycemic attention. Common hospital uses for IV insulin include the perioperative setting, during the use of high-risk medications (such as corticosteroids), or during crises such as diabetic ketoacidosis (DKA) [1,2]. Other conditions such as hyperglycemic hyperosmolar state (HHS) and trauma frequently require IV insulin, as well as specific hospital units such as the cardiothoracic intensive care unit [3,4]. The correlation between hyperglycemia and poor inpatient outcomes has been well described in the literature [5,6]. The treatment of hyperglycemia using an IV Continue reading >>
What is insulin shock therapy?
"Insulin therapy" redirects here. For the psychiatric treatment, see Insulin shock therapy. Insulin is used as a medication to treat high blood sugar. [3] This includes in diabetes mellitus type 1, diabetes mellitus type 2, gestational diabetes, and complications of diabetes such as diabetic ketoacidosis and hyperosmolar hyperglycemic states. [3] It is also used along with glucose to treat high blood potassium levels. [4] Typically it is given by injection under the skin, but some forms may also be used by injection into a vein or muscle. [3] The common side effect is low blood sugar. [3] Other side effects may include pain or skin changes at the sites of injection, low blood potassium, and allergic reactions. [3] Use during pregnancy is relatively safe for the baby. [3] Insulin can be made from the pancreas of pigs or cows. [5] Human versions can be made either by modifying pig versions or recombinant technology. [5] It comes in three main types short–acting (such as regular insulin), intermediate–acting (such as NPH insulin), and longer-acting (such as insulin glargine). [5] Insulin was first used as a medication in Canada by Charles Best and Frederick Banting in 1922. [6] It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system. [7] The wholesale cost in the developing world is about US$2.39 to $10.61 per 1,000 iu of regular insulin and $2.23 to $10.35 per 1,000 iu of NPH insulin. [8] [9] In the United Kingdom 1,000 iu of regular or NPH insulin costs the NHS 7.48 pounds, while this amount of insulin glargine costs 30.68 pounds. [5] Medical uses Giving insulin with an insulin pen. Insulin is used to treat a number of diseases including diabetes and its acute complications such as diabetic ketoacid Continue reading >>
What is bolus insulin?
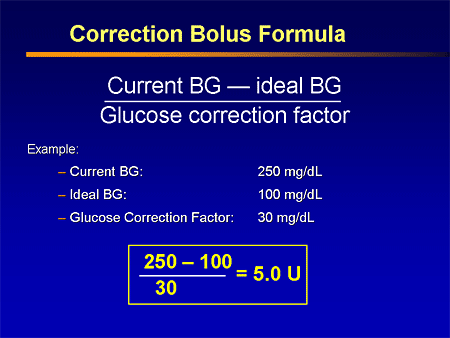
Bolus – High blood sugar correction (also known as insulin sensitivity factor) The bolus dose for high blood sugar correction is defined as how much one unit of rapid-acting insulin will drop the blood sugar. Generally, to correct a high blood Continue reading >>. Calculating Insulin Dose.
What is the background insulin called?
This is called background or basal insulin replacement . The basal or background insulin dose usually is constant from day to day. The other 50-60% of the total daily insulin dose is for carbohydrate coverage (food) and high blood sugar correction. This is called the bolus insulin replacement.
Why does insulin increase as you go from top to bottom?
As one slides from top to bottom, insulin dosage increases. This is because more insulin is needed to manage greater amounts of blood glucose. Mealtime This is usually plotted along the chart's top row. As one moves from breakfast to lunch to dinner within the same blood glucose level, dosage may vary.
Can you take insulin before or after a meal?
For people who have type 1 diabetes or insulin-deficient type 2 diabetes, these bursts must be recreated through insulin injections either before or after a meal. The sliding scale is one way of working out how much insulin to take before each meal. Most doctors advise against the sliding scale approach.