The approach to treatment of cervical facet joint syndrome is typically conservative, and includes:
- Resting to allow the facet joints to relax and reduce inflammation.
- Applying ice to the affected area in 10 to 15 minute intervals to help reduce inflammation.
- Stretching and strengthening exercises (Physical Therapy). [3] [6]
- Core exercises to help achieve good spine alignment and posture. [6]
Can stem cell therapy help facet joint syndrome?
Facet Joint Syndrome/Osteoarthritis ... A pioneering new treatment using your body’s own stem cells to treat pain and inflammation. The minimally invasive procedure is a possible alternative to having an operation or can be used after surgery to help healing. It harnesses natural repair cells removed from your body fat to target problems ...
What is the best exercise for facet joint pain?
With facet joint impingement, the best modes of aerobic exercise are:
- slow walking
- stationary cycling
- Elliptical machine
What are some treatment options for facet joint pain?
- Nonprescription medications like over-the-counter acetaminophen. ...
- Diagnostic facet injections. ...
- Yoga, or other low-impact stretching exercises. ...
- Strength training for muscle tone. ...
- Water therapy, such as swimming. ...
- Chiropractic or osteopathic manipulations. ...
- Posture corrections. ...
- Activity modification. ...
What is the treatment for cervical facet syndrome?
- Pain medications. Over-the-counter pain relievers like acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can help patients manage the symptoms of facet syndrome. ...
- Physical therapy. ...
- Application of heat or ice. ...
- Wearing a neck brace. ...
- Facet joint injections. ...

How long does it take for facet syndrome to heal?
How long does it take to heal a facet joint? As with any injuries healing times can change depending on numerous factors, such as age, weight, work and ability to avoid/manage aggravating activities. But typically, an acute sprain can take anywhere from 2-4 weeks if managed and treated correctly.
How do you treat facet syndrome?
Your doctor may recommend any of the following pain management treatment options:Heat and Cold Therapy. Heat and cold therapy can help ease pain caused by facet joint syndrome. ... Medications. ... Physical Therapy and Exercise. ... Proper Posture. ... Back Brace. ... Epidural Steroid Facet Injections. ... Medial Branch Injections.
Can damaged facet joints be repaired?
It involves the removal of your damaged facet joints via the posterior approach (from the back) and replacing them with a set of artificial facet joints, designed to restore your vertebra to the safe and correct position, while removing pain and retaining healthy movement.
Is facet joint disease permanent?
Facet joint syndrome is a widespread form of arthritis in older adults. It usually results from normal wear and tear, but injuries can worsen it. This condition can also affect younger people due to injury or overuse. Once the facet joint is damaged, it can cause long-lasting or permanent disability.
What aggravates facet joint?
What aggravates facet joint pain? Facet pain is usually heightened with activities that cause excess movement of the spine such as rotating or bending the spine backward, twisting, and lifting. Conversely, bending forward may relieve the pain.
Can chiropractor help facet syndrome?
Chiropractic is a proven, reliable treatment for relieving the pain and discomfort of facet syndrome. It helps restore mobility and flexibility while providing pain relief.
What kind of doctor treats facet joint syndrome?
Physiatrists: These rehabilitation physicians specialize in treating injuries or illnesses that affect movement. They manage non-surgical approaches to back pain, including the pain of facet joint syndrome.
Is facet syndrome a form of arthritis?
Facet joint syndrome is an arthritis-like condition of the spine that can be a significant source of back and neck pain. It is caused by degenerative changes to the joints between the spine bones. The cartilage inside the facet joint can break down and become inflamed, triggering pain signals in nearby nerve endings.
Do facet joint problems show on MRI?
Facet joint disorders have a wide range of causes and, because of the potential for chronic back pain and disability, an accurate diagnosis is essential. The most frequent cause of pain in facet joints is osteoarthritis, which can be assessed at radiography, CT, or MRI.
Is walking good for facet disease?
With facet joint impingement, the best modes of aerobic exercise are: slow walking. stationary cycling.
How do you get facet syndrome?
What Causes Facet Syndrome?Being overweight or obese.Fractures of the spine.Poor posture.Repetitive bending or twisting.Sedentary lifestyle.Sudden, vigorous stretching.Torn ligaments.Trauma, such as an accident, fall, or sports injury.
Is facet syndrome considered a disability?
Have you been diagnosed with facet joint syndrome or facet disease? Disability benefits may be available to you if your condition has made it impossible for you to earn a living. Below is an overview of this potentially debilitating disease and what is necessary to apply for disability benefits in such circumstances.
What kind of doctor treats facet joint syndrome?
Physiatrists: These rehabilitation physicians specialize in treating injuries or illnesses that affect movement. They manage non-surgical approaches to back pain, including the pain of facet joint syndrome.
Is facet syndrome considered a disability?
Have you been diagnosed with facet joint syndrome or facet disease? Disability benefits may be available to you if your condition has made it impossible for you to earn a living. Below is an overview of this potentially debilitating disease and what is necessary to apply for disability benefits in such circumstances.
Does facet joint pain require surgery?
Although most facet joint arthritis cases do not require surgery, if symptoms do not respond to other forms of treatment, a laminectomy or spinal fusion may be the next option. In addition to laminectomy surgery, spinal fusion is commonly performed to treat facet joint arthritis.
Does facet arthritis go away?
While there is no cure for facet arthropathy, there are ways to effectively manage the pain. Your orthopaedic specialist will work with you to find the least invasive treatment plan to manage your pain. Nonsurgical treatment options include: NSAIDs to fight pain and reduce inflammation.
How are Facet Joint Syndrome Symptoms Treated?
A conservative nonoperative approach is often the starting course of action, and this may include physical therapy and anti-inflammatory medication. Core strengthening exercises (eg, abdominals) and low back stretching are key to alleviate and prevent facet syndrome.
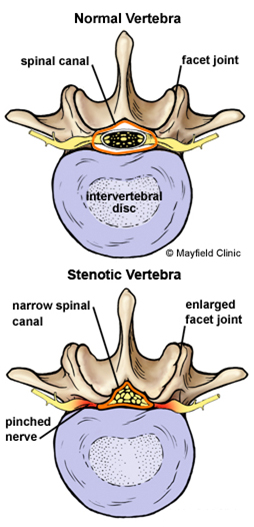
What is the role of the intervertebral disc in the facet joints?
Like any other joint in your body, each facet joints’ job is to promote healthy movement and—along with the intervertebral disc—provide stability for each motion segment. The disc functions as a spacer and to support motion between the vertebral bodies.
Why do my facet joints hurt?
Trauma—like whiplash from a car accident—is a common cause of facet joint syndrome in the neck. While aging is the leading cause of facet joint pain in the lumbar spine, trauma from a sports injury or auto accident can cause chronic low back joint pain too. Rarely do spinal tumors affect the facet joints and cause pain.
Why does my facet hurt?
The cause of facet joint syndrome is largely dependent on the region of the spine affected. For example, facet pain in the low back is typically caused by the degenerative effects of aging. Like the knee or hip joints, the facet joints are true synovial joints (fluid filled).
What is the most common site of facet joint pain in the lumbar spine?
The most common site of facet joint pain in the lumbar spine is at the L4-L5 level followed by L5-S1. Some researchers estimate that facet joint syndrome accounts anywhere from 15% of all low back pain complaints to 59.6% in men and 66.7% in women. 1. While facet joint syndrome most often affects the lumbar spine, ...
What is the name of the joint that connects two or more bones in your body and functions to promote motion?
Facet Joint Syndrome. A joint connects two or more bones in your body and functions to promote motion. In your spine, the joints connecting each of your vertebrae are known as facet joints. Other names for facet joints include zygapophyseal or apophyseal joints, or your doctor may refer to them as simply facets.
How does RFA work?
RFA blocks the nerve’s pain signals by heating the nerves with radiofrequency waves. RFA may be an appropriate treatment if your spinal joint pain isn’t responding well to injection therapy. RFA provides extended pain relief—possibly up to a year.
What is the best radiographic assessment for lumbar pain?
The initial radiographic assessment of patients presenting with lumbar facet-mediated pain includes AP, lateral, and oblique views [18]. Oblique radiographs are the best projections for assessing FJs of the lumbar spine because of their oblique position (“Scottie dog”). Lateral films, however, may provide useful information from the isthmus profile such as the pars interarticularis defect. Because of its ability to provide cross-sectional images and to provide a higher contrast between bony structures, CT improves anatomic evaluation of the FJs and is the preferred method for imaging FJ osteoarthritis [46]. However, standard radiographs can also show pathological changes especially in severe disease. Degeneration is characterized by joint space narrowing, sclerosis, subchondral sclerosis and erosions, cartilage thinning, calcification of the joint capsule, hypertrophy of articular processes and of the ligamentum flavum causing impingement of the foramina and osteophytes. Secondary signs include vacuum joint phenomenon (intra-articular gas), joint effusion and associated degenerative spondylolisthesis. Synovial and subchondral cysts can extend posterior to the FJ but also anterior in the spinal cord or neuroforamen. Kalichman et al. showed 24% of X-rays FJOA before 40 years and 89% in the 60–69 years population, but once again with no correlation between abnormal morphology on radiologic findings and back pain [4].
What are the classifications of FJ degeneration?
Two classifications of FJ degeneration are recommended for clinical use. Radiographically, Pathria’s classification classifies FJ arthropathy as well: Facets with joint space narrowing are classified as grade 1, facets with narrowing and sclerosis or hypertrophy as grade 2, and facets with severe degenerative disease encompassing narrowing, sclerosis, and osteophytes as grade 3 [57]. Standard radiographs (Meyerding or Taillard classification) [33] also evaluate motion-related abnormalities in flexion or extension, and assess instability in cases of spondylolisthesis, thanks to dynamic studies. In the setting of degenerative spondylolisthesis, a weight-bearing lateral flexion-extension radiograph is most effective for grading spondylolisthesis and may be needed in addition to MRI and CT imaging. Anteroposterior translation of more than a few millimetres is suggestive of lumbar spine instability in the sagittal plane, which in the appropriate clinical setting may require surgical arthrodesis. In addition to Pathria’s classification, Weishaupt’s grading scheme, based on the agreement between MRI and CT imaging, has been proposed. Facets were again graded from 0 to 3 depending on the degree of joint space narrowing, hypertrophy, sclerosis, and osteophyte formation. The authors recommended against the routine use of CT imaging in the presence of an adequate MRI scan [49]. Fujiwara et al. is credited with developing the standard MRI-based classification system for lumbar FJ osteoarthritis. An additional grading system for foramen stenosis, caused by disc and FJ degeneration can be used as well, based on the depiction of the foraminal components: nerve, vessels and fat [58]. First stage, the non stenotic stage: no modifications depicted. Second stage corresponds to stenosis without evidence of root compression. Third stage, compression of the spinal nerve in the intervertebral foramen caused by either intervertebral disc, flaval ligament or osseous stenosis. In this stage, the content of the foramen is not well identified. A grading scale has also been proposed for lumbar canal stenosis as follows [59]: A) cerebro-spinal fluid (CSF) is clearly visible inside the thecal sac, but its distribution is inhomogeneous. B) Some CSF is still present, giving a grainy appearance to the thecal sac. The rootlets occupy the whole of the dural sac, but they can still be individualized. C) the dural sac demonstrates a homogeneous grey signal with no CSF. No rootlets can be recognized. D) In addition to no rootlets being recognizable, there is no epidural fat posteriorly.
What is degenerative spondylolisthesis?
Degenerative spondylolisthesis is the displacement of one vertebra to another in the sagittal plane , which is related in the majority of cases to FJ osteoarthritis and failure of the motion segment. It occurs as a result of subluxation of the FJs, related to an important and progressive loss of cartilage and articular remodelling, with segmental instability causing capsule tension [22]. Spondylolisthesis most often occurs at the L4–5 level, which is predominantly affected by osteoarthritis [33]. In younger populations (30–40 years old), spondylolisthesis can be due to congenital abnormalities, acute or stress-related fractures or isthmic spondylolisthesis. As opposed to its degenerative counterpart, L5–1 is the most affected level, and related instability seems to be more frequent [34].
What is the most common form of back pain?
Lumbar facet joints (FJ) constitute a common source of pain, accounting for 15–45% of LBP. Facet joint degenerative osteoarthritis is the most frequent form of facet joint pain. History and physical examination may suggest but not confirm facet joint syndrome. Although imaging (radiographs, MRI, CT, SPECT) for back pain syndrome is very commonly performed, there are no effective correlations between clinical symptoms and degenerative spinal changes. Diagnostic positive facet joint block can indicate facet joints as the source of chronic spinal pain. These patients may benefit from specific interventions to eliminate facet joint pain such as neurolysis, by radiofrequency or cryoablation. The purpose of this review is to describe the anatomy, epidemiology, clinical presentation, and radiologic findings of facet joint syndrome. Specific interventional facet joint management will also be described in detail.
Which spondyloarthropathies are seronegative?
Rheumatoid arthritis and ankylosing spondylitis, which are seronegative spondyloarthropathies, may also involve the lumbar FJs, as FJs are synovial joints [18].
Is MRI good for FJ?
MRI is a noninvasive and nonionizing modality that provides excellent soft tissue resolution. The role of MRI in the evaluation of FJ degeneration is not proven. Osteoarthritis may be present in both symptomatic and asymptomatic patients (from 8 to 14%) [47, 48]. Superior sensitivity of MRI compared to CT imaging is controversial [8]. CT and MRI are equally useful in demonstrating morphological changes in FJ. One of the two examinations is thus sufficient for assessing degenerative changes [49]. MRI, however, clearly presents advantages of better assessing the immediate consequences of FJ degeneration, such as surrounding neural structure impingement [50]. Chronic degenerative osteoarthritis processes in these structures involve active synovial inflammation or adjacent bone edema, which can be detected using MRI with a fat saturation technique [51]. Exaggerated fluid in the facets and FJ synovial cysts seen on axial MRI seems to be significantly suggestive of spondylolisthesis and its instability, but is not specific of FJ origin of pain [52]. Recent studies using fat-suppressed MRI sequences have demonstrated that subchondral bone edema is present in the lumbar FJ articular processes in 14 to 41% of patients with back pain [53, 54]. Enhancement of the FJ rim after gadolinium administration will establish a diagnosis of synovitis. Fujiwara et al. proposed a four-grade classification from 1 to 4 [55]: grade 1, normal; grade 2, joint space narrowing or mild osteophyte; grade 3, sclerosis or moderate osteophyte; and grade 4, marked osteophyte. They additionally described the wraparound bumper osteophyte formations which provides an additional stabilizing effect in segmental degenerative disease. An important observation from the Fujiwara study is that MRI tends to underestimate the severity of osteoarthritis of the FJs as compared to CT. The fluid-sensitive sequences on MRI are generally preferred over CT for imaging FJ effusions and juxta-facet cysts; however, they are less sensitive in depicting the joints’ bony cortices and are less accurate in quantifying the amount of sclerosis present. An additional limitation of MRI is that it cannot accurately measure cartilage thinning secondary to the partial volume effect and chemical-shift artefact inherent in this type of imaging. CT is better able to demonstrate the degenerative changes of the FJs because of the high contrast between bony structures and the surrounding soft tissues [18]. However, some authors suggest that TSE T2 fat saturation sequences and, when indicated, gadolinium administration with T1 fat saturation sequences enhance the sensitivity and diagnostic specificity of MR scans. In particular, gadolinium will disclose the active inflammatory stage of a degenerative process thereby identifying new therapeutic targets for percutaneous treatment [51].
Is chronic pain a health problem?
Chronic and recurrent pain has been defined as a specific health care problem and is considered a disease in its own right [10]. A recent survey showed a high prevalence of chronic pain of moderate to severe intensity in adult Europeans, affecting the quality of their social and working lives and is therefore a major health care problem in Europe [1]. Low back pain (LBP) is one of the most common pain syndromes and is an enormous burden and cost generator for society. The high health care costs may be attributed to multiple factors, including lack of an accurate diagnosis [2], imaging overuse, unwarranted surgery and working stoppages. LBP is responsible for functional limitations and causes difficulty in performing common daily life tasks, especially among the elderly [11]. Therefore, LBP is the most expensive disease in industrialized countries, as has been reported in Germany at a total cost of 48.960 billion euros per year [12]. In the USA, the prevalence of LBP is reportedly between 15 and 45% according to cross-sectional studies [13]. Most spinal structures may be source of LBP, including intervertebral discs, FJs, sacroiliac joints and nerve roots, and may be accessible to diagnostic tests including imaging. Some disorders, particularly disc-related impairments, are reasonably easily diagnosed and lead to definitive treatments. However, discogenic LBP without disc herniation, lumbar FJ, and sacroiliac joint pain are difficult to diagnose with imaging only [2]. The literature focuses on intervertebral discs as the source of LBP; however, FJ pain also seems to play a major role in generating LBP [8]. Among LBP patients, there are wide discrepancies in the reported prevalence of FJ pain. Reviews implicate FJs as the primary pain generator in 10–15% of young adult patients with chronic LBP and higher in older populations (15% among injured workers, 40% in older population without pre-existing trauma, 45% in a more heterogeneous population) [14]. Controlled diagnostic studies have shown a prevalence of lumbar FJ pain of 27–40% in patients with chronic LBP [15].
Why do you need a facet injection?
A facet joint injection may be done to help diagnose the facet joints as the source of pain, as well as to provide pain relief. Watch: Facet Joint Injections Procedure Video. For pain and dysfunction that does not respond to nonsurgical care, or for severe conditions, such as complex fractures, significant dislocations, or spinal cord involvement, ...
What is the treatment for facet joint pain?
Treatment injections contain numbing medications that work on the nerves around the facet joint, reducing their ability to carry pain signals to the brain. Injections also contain steroids, which decrease the inflammatory reactions in the facet joint, reducing the pain.
What is the best treatment for a facet joint?
Nonsurgical treatments are usually the first line of treatment and have a favorable success rate in terms of reducing pain that originates from a facet joint. A full range of treatments are available, and typically several are done at the same time.
How to treat lumbar facet pain?
Treatments that may be performed at home to relieve lumbar facet pain include: Applying heat therapy. Heat therapy can help relax the muscles and open up blood vessels to allow blood flow and oxygen to reach the painful tissues, providing nourishment.
Why is it important to maintain the natural spinal alignment by using correct sitting, standing, and/or lying down posture?
It is important to maintain the natural spinal alignment by using correct sitting, standing, and/or lying down posture. A good posture helps keep stresses off the facet joints and foster a better healing environment.
How to help lumbar pain?
Staying active. While avoiding certain activities is recommended, it is also necessary to stay active in moderation and avoid complete bed rest, which may decondition the lumbar tissues and increase the pain.
What is cold therapy?
Cold therapy may be used when the pain is acute or during a pain flare-up, such as after strenuous physical activity. A cold pack constricts the blood vessels, reducing blood flow to the region and numbing the pain. See Ice Packs for Back Pain Relief. Supporting the lumbar curve.
What causes a twisting spine?
Any twisting of the spine has the potential for injury. A few of the known culprits are: golf. over-extending. leaning backward. Another option is to explore several pain management treatments. The key is to work your way up, starting with the less aggressive treatments first.
What is the best treatment for facet joint syndrome?
When a more permanent solution is needed, surgery can help. There are two different surgical options to consider: Spinal Fusion, and something called Facet Debridement.
Where are facet joints located?
Unlike spinal conditions caused by acute injury, facet joint syndrome develops with age. Facet joints are located in the spine, and help with normal range of motion like twisting from side to side. Each joint is lined with a nerve-rich substance called “ synovial tissue “.
How long does a rfa last?
Next, you might consider prescription drugs (cortisone, novocaine, etc.) Finally, RFA (or radiofrequency ablation) can also be used to manage pain for up to 12 months.
Why does my lower back hurt?
Specifically, suffers will experience pain in the lower back region. The sensation of pain is caused by tiny nerves and tissues that get compressed . Other symptoms occur at the anatomical level, and are less likely to be “felt”. These symptoms include: less water volume in the joints.
Can facet joint syndrome be treated without surgery?
However, the vast majority of people are able to manage their symptoms without surgery for many years. One option is to avoid activities that are known to aggravate the facet joins. Any twisting of the spine has the potential for injury.
Is spinal fusion surgery risky?
Spinal fusion is the more dramatic and risky of the two surgical options. Because of the invasiveness of this approach, recovery time is quite long and complications are not uncommon. Studies show that the success-rate of this surgery is only 66%.
What is facet joint pain?
These small bones are stacked one above the other. Each vertebra consists of three parts – a large disc and two projections behind it which are called facets. These three structures form a tripod that gives the spine stability and flexibility. 1 It allows us to bend and twist while keeping the spinal bones linked together.
What causes numbness in buttocks and legs?
Bone spurs irritate the nerves, causing symptoms such as pain, numbness, and weakness in the buttocks and legs. 5. Facet joint arthropathy is often associated with another condition called degenerative disk disease (DDD). DDD occurs with age where the vertebral disks become worn out.
What causes facet joints to wear down?
Common causes of worn down facet joints. Osteoarthritis. This is an age-related breakdown of cartilage in the joints. It is most often seen in large joints like the knee and hip but can affect any joint in the body, including the spinal facet joints.>. Injuries.
Why does my facet hurt?
The main symptom of facet joint pain is significant back and neck pain. 1 The pain is caused by degenerative changes in the facet joints. In other words, the cartilage in the facet joints breaks down and becomes inflamed. The damage to the cartilage causes the bones in the joint to rub together, leading to symptoms such as pain, swelling, ...
What are the facets of the vertebrae?
The facets of the vertebrae are linked to one another at the facet joints. Each joint is lined with cartilage and has a lubricating synovial fluid inside a joint capsule. When the facet joints are healthy, they glide easily and allow us to move our back and neck without pain.
What is the best test for facet joint pain?
Imaging tests such as X-ray, CT scan, and MRI can help confirm the diagnosis of facet joint pain by demonstrating abnormal changes in the facets. A facet joint block is an injection of local anesthetic and steroid medication into a suspicious facet joint. This is sometimes performed to make a diagnosis.
What is facet joint syndrome?
Facet joint syndrome is a frustrating condition. It causes unpredictable back and neck pain that can reduce your quality of life and keep you from doing the things you love.
What is the best way to treat back pain from facet joint?
A minimally invasive facet fusion is the most recommended surgical option for eliminating back pain from conditions like facet arthritis and facet joint syndrome. This outpatient procedure is performed through a tiny incision and with no sutures needed.
How to treat spondylosis?
Spondylosis is usually well addressed with a combination of medication and physical therapy. For more serious cases, decompression surgery may be warranted. Two of the most popular types of minimally invasive decompression surgeries used today to treat this condition are: 1 Foraminotomy —Minimally invasive foraminotomy is performed through a very small incision in the back. We place a small tube between the muscle fibers to preserve the muscles, tendons, and ligaments, significantly reducing post-operative pain, recovery time, and the potential for any reinjury. Specialized instruments and microscopes are then used to remove a small piece of bone and soft tissue, taking pressure off of the nerve. This outpatient procedure involves very minimal blood loss and is sutureless. 2 Laminectomy —Minimally invasive laminectomy is a type of decompression surgery we perform through a small incision—typically just one-half-inch long—and with great care to preserve muscles, tendons, and soft tissue. The procedure takes about 45 minutes and patients are usually up and walking soon after it’s over. Since it’s an outpatient procedure, they’re able to return home within about an hour. Minimally invasive laminectomy may also be a viable option if more conservative treatments have not relieved the pain of facet hypertrophy.
How do you know if you have a facet joint problem?
However, there are some telltale signs you’ll want to be aware of. Common symptoms of facet joint problems include: Pain that is worse first thing in the morning or at the end of the day. Pain that changes or worsens because of the weather. Pain that improves or worsens when you sit or stand.
Why do my facet joints hurt?
Facet joint syndrome is one of the most common conditions related to these joints. The facet joints swell up due to spinal arthritis or injury , causing painful symptoms. If the facet joint issue is cervical, symptoms may include bad headaches and neck stiffness. If the affected joint is located in the lower back, there may be extreme pain in the back that extends down into the buttocks and thighs. Facet joint syndrome can make it hard to do simple movements like turning your head, standing up straight, or walking without being hunched over, depending on where the affected joint is located.
How is foraminotomy performed?
Foraminotomy —Minimally invasive foraminotomy is performed through a very small incision in the back. We place a small tube between the muscle fibers to preserve the muscles, tendons, and ligaments, significantly reducing post-operative pain, recovery time, and the potential for any reinjury.
What causes a pinched nerve in the facet?
This occurs when a swollen facet joint blocks a nerve pathway, leading to a pinched nerve. Spondylosis is also common with facet joint issues. Spondylosis is arthritis of the spine but is also used as ...
How to treat a facet joint?
Initially, your treatment plan may include a combination of anti-inflammatory medication and physical therapy, which will typically involve stretching and core strengthening exercises. Many patients with facet joint pain see significant improvement from this type of program and don’t need further treatment. However, if the facet joint pain has ...
Why does my facet hurt?
Causes of Lumbar Facet Joint Pain. Facet joint degenerative osteoarthritis is the most common form of Facet joint pain. [1] . It is the result of degenerative changes to the joints that are located between the bones of the spine, known as the facet joints. This condition is often (not always) tied to the degenerative changes ...
What causes lumbar facet joint pain?
These conditions include: Overuse Injuries (i.e. traumatic fall, sporting injury, etc). [6]
How to treat cervical facet joint?
The approach to treatment of cervical facet joint syndrome is typically conservative, and includes: 1 Resting to allow the facet joints to relax and reduce inflammation. 2 Applying ice to the affected area in 10 to 15 minute intervals to help reduce inflammation. 3 Stretching and strengthening exercises (Physical Therapy). [3] [6] 4 Core exercises to help achieve good spine alignment and posture. [6] 5 Posture/Ergonomics education to keep the facet joints in alignment and reduce unnecessary pressure on the affected facet joints. [6] 6 Medications, such as non-steroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants, to ease muscle spasm in the muscles surrounding the affected facet joints. [1] [2] [6] 7 Behavioral therapy [3]
What is the purpose of posture education?
Posture/Ergonomics education to keep the facet joints in alignment and reduce unnecessary pressure on the affected facet joints. [6]
How to get rid of a swollen facet joint?
Resting to allow the facet joints to relax and reduce inflammation. Applying ice to the affected area in 10 to 15 minute intervals to help reduce inflammation. Stretching and strengthening exercises (Physical Therapy). [3] [6] Core exercises to help achieve good spine alignment and posture. [6]
What is facet joint pain?
Symptoms of Facet Joint Pain Syndrome. Widespread, achy back pain (affecting one/both sides of body) that radiates to one or both buttocks, sides of the groin, and thighs, and stops above the knee. [1] Pain may be chronic or come and go.
How to do a plank on your stomach?
How to do it: – Begin lying on your stomach with your forearms against the mat. – Engage your core and lift your body so that you are resting on your forearms and toes. – Hold the plank position for 30-60 seconds. – Aim for 2 to 5 repetitions of this exercise.
