
Causes
Causes
- If a heart problem causes the pulmonary edema, it's called cardiogenic pulmonary edema. Most often, the fluid buildup in the lungs is due to a heart condition.
- If pulmonary edema is not heart related, it's called noncardiogenic pulmonary edema.
- Sometimes, pulmonary edema can be caused by both a heart problem and a non-heart problem.
Symptoms
The clinical presentation of pulmonary edema includes:
- acute breathlessness
- orthopnea
- paroxysmal nocturnal dyspnea (PND)
- foaming at the mouth
- distress
Prevention
Treatment
- Medication. Medications such as corticosteroids and NSAIDS treat edema in a way that it reduces the swelling and inflammation however it doesn’t treat the underlying condition.
- Antihistamines. For edema caused by allergic reactions, antihistamines would treat the swelling. ...
- Diuretics. ...
Complications
Pulmonary edema is a serious medical condition that happens when excess fluid begins to fill the lungs' air sacs (the alveoli). When the alveoli are filled with fluid, they cannot adequately add oxygen to, or remove carbon dioxide from, the blood.
What is the most common cause of pulmonary edema?
What are the signs of a pulmonary edema?
What is the best treatment for pulmonary edema?
Why is pulmonary edema a serious problem?

What causes pulmonary flash edema?
Flash pulmonary edema is caused by abrupt physiologic derangement such as a sudden increase in blood pressure, acute myocardial ischemia, acute myocarditis, acute valve dysfunction (e.g., mitral regurgitation), or arrhythmia.
What drug causes flash pulmonary edema?
Additional drugs that can cause noncardiogenic pulmonary edema include carbamazepine, cytarabine, erythromycin, hydrochlorothiazide, IV radiographic contrast agents, methotrexate, protamine, tamoxifen, and tumor necrosis factor.
How do you fix flash pulmonary edema?
The first treatment for acute pulmonary edema is oxygen. Oxygen flows through a face mask or a flexible plastic tube with two openings (nasal cannula) that deliver oxygen to each nostril. This should ease some symptoms....TreatmentDiuretics. ... Blood pressure drugs. ... Inotropes. ... Morphine (MS Contin, Infumorph, others).
Is flash pulmonary edema heart failure?
Flash pulmonary edema (FPE) is a general clinical term used to describe a particularly dramatic form of acute decompensated heart failure.
When does flash pulmonary edema occur?
Green's signs and symptoms, you suspect flash pulmonary edema, a life-threatening condition that occurs when fluid suddenly shifts from the pulmonary vasculature into the lung interstitium and alveoli. Pulmonary edema can be caused by pneumonia, MI, trauma, or inhalation of toxic chemicals.
What is the most common cause of pulmonary edema?
Pulmonary edema is often caused by congestive heart failure. When the heart is not able to pump efficiently, blood can back up into the veins that take blood through the lungs. As the pressure in these blood vessels increases, fluid is pushed into the air spaces (alveoli) in the lungs.
How long does it take to recover from flash pulmonary edema?
With treatment, most people with this type of pulmonary edema recover in about 24 hours.
What stage of heart failure is pulmonary edema?
Pulmonary edema is acute, severe left ventricular failure with pulmonary venous hypertension and alveolar flooding. Findings are severe dyspnea, diaphoresis, wheezing, and sometimes blood-tinged frothy sputum. Diagnosis is clinical and by chest x-ray.
What stage of heart failure is edema?
Patients in the end stages of heart failure want to know what to expect. The symptoms of end-stage congestive heart failure include dyspnea, chronic cough or wheezing, edema, nausea or lack of appetite, a high heart rate, and confusion or impaired thinking.
How long can you survive with pulmonary edema?
Pulmonary edema is life-threatening, but your prognosis depends on what caused it. One year after discharge from a hospital, about 50% survive cardiac edema. Heart failure, a common cause of cardiogenic pulmonary edema, is a chronic disease that can get better with treatment.
Can pulmonary edema cause sudden death?
Pulmonary edema that develops suddenly (acute pulmonary edema) is a medical emergency that needs immediate care. Pulmonary edema can sometimes cause death. Prompt treatment might help. Treatment for pulmonary edema depends on the cause but generally includes additional oxygen and medications.
How do you know if you have fluid in your lungs?
The symptoms of pleural effusion can range from none to shortness of breath to coughing, among others. The greater the build-up of fluid, the more likely symptoms will be noticeable. In addition to excess fluid, the tissue around the lung may become inflamed, which can cause chest pain.
How do beta blockers cause pulmonary edema?
Beta-blockers may cause cardiogenic pulmonary edema secondary to their negative inotropic and negative chronotropic effects. The drug's lipid solubility or a deficiency in the enzyme responsible for its metabolism may have allowed the drug to accumulate to a critical concentration over the 6-week period of use.
What medications cause pulmonary embolism?
Certain medications (eg, birth control pills, hormone replacement therapy, tamoxifen, thalidomide, erythropoietin, cancer chemotherapy medications). The risk of a blood clot is further increased in people who use one of these medications and also have other risk factors.
What toxins can cause pulmonary edema?
Agents with low water solubility, such as nitrogen dioxide or phosgene, can penetrate into the lower respiratory tract and pulmonary parenchyma, causing pulmonary edema following a latent period of several hours.
What medications can cause pleural effusion?
Eosinophilic pleural effusion is usually seen with drugs like nitrofurantoin, dantrolene, bromocriptine, valproic acid, isotretionin, prophythiouracil and angiotensin-converting enzyme inhibitors.
Why is pulmonary edema so hard to breathe?
Overview. Pulmonary edema is a condition caused by excess fluid in the lungs. This fluid collects in the numerous air sacs in the lungs, making it difficult to breathe. In most cases, heart problems cause pulmonary edema. But fluid can collect in the lungs for other reasons, including pneumonia, exposure to certain toxins and medications, ...
What are the symptoms of pulmonary edema?
Sudden (acute) pulmonary edema signs and symptoms. Difficulty breathing (dyspnea) or extreme shortness of breath that worsens with activity or when lying down. A feeling of suffocating or drowning that worsens when lying down. A cough that produces frothy sputum that may be tinged with blood.
What is cardiogenic pulmonary edema?
Cardiogenic pulmonary edema is caused by increased pressures in the heart.
How long does it take for pulmonary edema to heal?
With treatment, most people with this type of pulmonary edema recover in about 24 hours.
Why does fluid build up in the lungs?
Most often, the fluid buildup in the lungs is due to a heart condition. If pulmonary edema is not heart related, it's called noncardiogenic pulmonary edema. Sometimes, pulmonary edema can be caused by both a heart problem and a non-heart problem.
What causes fluid to leak from the blood vessels to the lung tissues?
High-altitude pulmonary edema. In normal lungs, air sacs (alveoli) take in oxygen and release carbon dioxide. In high-altitude pulmonary edema (HAPE), it's theorized that vessels in the lungs constrict, causing increased pressure. This causes fluid to leak from the blood vessels to the lung tissues and eventually into the air sacs.
How high can you travel to get pulmonary edema?
People who travel to high-altitude locations above 8,000 feet (about 2,400 meters) are more likely to develop high-altitude pulmonary edema (HAPE). It usually affects those who do not first become acclimated to the elevation (which can take from a few days to a week or so).
How to prevent pulmonary edema?
The best way to try and prevent pulmonary edema is by taking good care of your health: Get a pneumonia vaccine. Get the flu vaccine, especially if you have heart problems or if you are an older adult. Remain on diuretics after an episode of pulmonary edema to prevent a reoccurrence.
What is the first line of treatment for pulmonary edema?
Pulmonary edema is a serious condition that requires quick treatment. Oxygen is always the first line of treatment for this condition. Your healthcare team may prop you up and deliver 100 percent oxygen through an oxygen mask, nasal cannula, or positive pressure mask.
What is pulmonary edema?
Overview. Pulmonary edema is a condition in which the lungs fill with fluid. It’s also known as lung congestion, lung water, and pulmonary congestion. When pulmonary edema occurs, the body struggles to get enough oxygen and you start to have shortness of breath. But timely treatment for pulmonary edema and its underlying cause can improve possible ...
Why does pulmonary edema make you lose oxygen?
This is due to the amount of increasing fluid in the lungs preventing oxygen moving into the bloodstream. Symptoms may continue to worsen until you get treatment.
Why do you need to stay on diuretics after pulmonary edema?
Remain on diuretics after an episode of pulmonary edema to prevent a reoccurrence.
What tests are used to check for pulmonary edema?
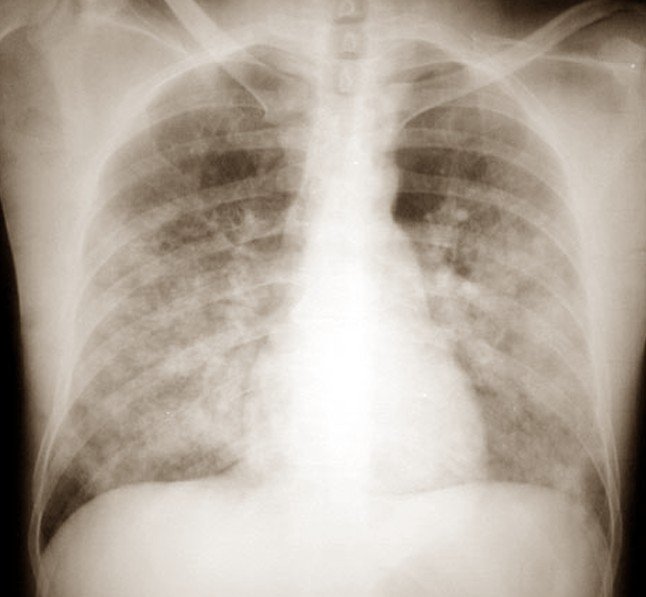
Examples of tests used in diagnosing pulmonary edema include: complete blood count. echocardiogram, or an ultrasound, to check for abnormal heart activity. chest X-ray to see fluid. blood tests to check oxygen levels.
What are the risk factors for pulmonary edema?
Risk factors of pulmonary edema. People with heart problems or heart failure are the most at risk for pulmonary edema. Other factors that may put a person at risk include: history of pulmonary edema. history of lung disease, such as tuberculosis or chronic obstructive pulmonary disorder (COPD) vascular (blood) disorders.
What is flash pulmonary edema?
Flash pulmonary edema is largely a diagnosis of exclusion, which is usually made after exclusion of other more common causes of pulmonary edema such as left ventricular systolic impairment or reversible myocardial ischemia.
What is the best way to evaluate pulmonary edema?
Evaluation of the patient with pulmonary edema should focus on the severity of the respiratory distress and required respiratory support then shift to an assessment of etiology. Chest radiography and 12-lead electrocardiography are cornerstones of management, and laboratory evaluation should include cardiac troponins, complete blood count (CBC), complete metabolic panel (CMP), and brain natriuretic peptide level. Transthoracic echocardiography may be considered for better definition of cardiac structure and function.
What causes a transudative edema fluid to enter the interstitium and the alve?
Elevated filling pressures in the left heart cause an increase in pulmonary venous pressures and increased hydrostatic pressure in the pulmonary capillary bed. These changes force a transudative edema fluid into the interstitium and the alveoli when the left atrial pressure increases above 18 mm Hg.
Is balloon angioplasty a good treatment for FMD?
14-12 ). Balloon angioplasty remains the treatment of choice for FMD and is an accepted treatment for selected patients with RAS causing renovascular hypertension and/or renal insufficiency. However, atherosclerotic aorto-ostial renal artery lesions are particularly difficult to treat with balloon angioplasty alone because they are prone to significant vascular recoil, leading to a restenosis rate of approximately 50% over 6 months. Balloon angioplasty alone may have negligible long-term benefit for controlling blood pressure, probably because of a high restenosis rate. The current long-term patency rates for renal stenting are excellent, with restenosis rates approaching 10%. Stent placement is favored over balloon angioplasty and carries ACC/AHA class I recommendation for treatment of atherosclerotic RAS.
Can pulmonary edema be recurrent?
IRD may present as recurrent episodes of flash pulmonary edema. These episodes can be unpredictable, sudden, and life-threatening and may be associated with low, normal, or very high BP at the time of presentation. Renal revascularization can reverse the cyclical flash pulmonary edema and improve pulmonary function even in those patients with poor preoperative cardiopulmonary status.28 In one series, 41% of subjects with bilateral renal artery stenosis had a history of pulmonary edema compared with 12% with unilateral renovascular disease. Seventy-seven percent of the patients with bilateral renal artery stenosis had no further pulmonary edema after renal artery stent placement in one or both arteries. The patients who did have recurrent pulmonary edema all had evidence of stent thrombosis or restenosis. 29 The mechanisms of pulmonary edema reflect combinations of diastolic or systolic ventricular dysfunction occurring in association with chronic reduction in GFR and sodium retention. These may coincide with superimposed episodes of severe hypertension or further increases in sodium retention. There are no prospective clinical studies specifically examining the effect of optimal medical therapy for BP and volume status on the frequency of events in these patients. Initial reports from prospective, randomized clinical studies, such as the Angioplasty and Stenting for Renal Artery Lesions (ASTRAL) study, demonstrated no differences in hospitalizations or episodes of congestive heart failure (CHF) in intensively treated subjects with or without renal artery stenting. 30
Can a stent cause pulmonary edema?
Recurrent CHF and “flash” pulmonary edema not related to ischemic heart disease can result from bilateral RAS (or unilateral RAS to a single functioning kidney). In a renal artery stent series, 39 patients (19% of all patients undergoing renal artery stent implantation from 1991 to 1997) had recurrent episodes of CHF or “flash” pulmonary edema as the primary indication for renal artery stenting. 20 Nineteen of 39 patients had moderate-to-severe left ventricular systolic function. Although not completely understood, the mechanism of CHF may be related in part to the inability to use ACE inhibitors or angiotensin receptor blockers (ARBs), to the direct adverse effects of angiotensin II on myocardial function, or to the inability to control volume adequately. If coronary ischemia has been excluded as a cause of CHF, renal revascularization (surgical or percutaneous stenting) is a very effective method of treatment in these individuals. 20–22
Is ARAS a cause of HTN?
ARAS has been implicated as a cause of HTN, deterioration of renal function, and cardiac disturbance syndromes (recurrent unexplained congestive heart failure, refractory angina, and “flash” pulmonary edema). HTN related to underlying RAS should be suspected in individuals who either are young, suggesting a nonatherosclerotic etiology, or are older than 55 years at the time of onset of HTN. Resistant HTN—defined as the inability to achieve goal blood pressure of 140/90 mm Hg or lower despite the use of three antihypertensive medications at maximum tolerable doses and in appropriate combinations—is another important clinical clue for underlying RAS. 7 Other significant clinical clues, which should prompt an investigation for ARAS, are listed in Box 37-1.
How to treat pulmonary edema?
The first treatment for acute pulmonary edema is supplemental oxygen. You usually receive oxygen through a face mask or nasal cannula — a flexible plastic tube with two openings that deliver oxygen to each nostril. This should ease some of your symptoms.
What is the first treatment for pulmonary edema?
Treating high-altitude pulmonary edema (HAPE) As with other forms of pulmonary edema, oxygen is the usually the first treatment. If supplemental oxygen isn't available, you may use portable hyperbaric chambers, which imitate a descent for several hours until you are able to move to a lower elevation.
What test is used to diagnose pulmonary edema?
Blood tests to diagnose pulmonary edema and its causes also usually include a complete blood count, metabolic panel to check kidney function and thyroid function test. Electrocardiogram (ECG or EKG). This painless test detects and records the timing and strength of your heart's signals using small sensors ...
How high can you climb to get pulmonary edema?
If you're climbing or traveling at high altitudes and have mild symptoms of HAPE, descend 1,000 to 3,000 feet (about 300 to 1,000 meters) as quickly as you can, within reason.
What test is done to determine if you have fluid in your lungs?
Tests that may be done to diagnose pulmonary edema or to determine why you developed fluid in your lungs include: Chest X-ray. A chest X-ray can confirm the diagnosis of pulmonary edema and exclude other possible causes of your shortness of breath. It's usually the first test done when someone has signs or symptoms of pulmonary edema. Chest CT.
What blood test is used to check for oxygen and carbon dioxide?
Arterial blood gas test. Blood is taken, usually from an artery in your wrist, and checked for the amount of oxygen and carbon dioxide it contains (arterial blood gas concentrations). B-type natriuretic peptide (BNP) blood test. Increased levels of BNP may signal a heart condition. Other blood tests.
Does morphine cause pulmonary edema?
But some doctors believe that the risks of morphine may outweigh the benefits and are more likely to use other drugs. Blood pressure drugs. If you have high or low blood pressure when you develop pulmonary edema, you'll be given medications to help manage the condition.
How to prevent pulmonary edema?
Some lifestyle changes can prevent pulmonary edema or help keep the condition in check. Keep your heart healthy by: Eating plenty of vegetables, fruits, and whole grains. Eating less salt.
What Is Pulmonary Edema?
Pulmonary edema is a buildup of fluid in your lungs. That can make it hard for you to breathe.
What causes a swollen leg and feet?
Have swollen legs and feet. Have trouble breathing when lying down. Wake up at night with a breathless feeling that gets better if you sit up. Wheeze. Pulmonary Edema Causes. There are two main kinds of pulmonary edema : cardiogenic and noncardiogenic. Cardiogenic pulmonary edema.
Why does my left ventricle have a buildup of fluid?
In many cases, your left ventricle (one of the chambers of your heart) isn’t able to pump out blood that enters through blood vessels from your lung. This creates a buildup of pressure and fluid.
What happens when you take a breath?
When you take a breath, your lungs should fill with air. If you have pulmonary edema, they fill with fluid instead. When that happens, oxygen from the air can’t get from your lungs into your blood, where it’s needed.
What causes a dry cough?
Symptoms include chest pain, shortness of breath, and a dry cough. It can be caused by problems like heart failure, blood clots, pneumonia, kidney disease, and tuberculosis. Pneumonia also leads to fluid buildup in the tiny air sacs in your lungs, but it’s caused by an infection with a virus, bacteria, or fungus.
How to get oxygen right away?
Pulmonary Edema Treatment. If you’re having trouble breathing and your oxygen level is low , you’ll get oxygen right away.
What is pulmonary edema?
Pulmonary edema can be defined as an abnormal accumulation of extravascular fluid in the lung parenchyma. This process leads to diminished gas exchange at the alveolar level, progressing to potentially causing respiratory failure. Its etiology is either due to a cardiogenic process with the inability to remove sufficient blood away from the pulmonary circulation or non-cardiogenic precipitated by injury to the lung parenchyma. It is an important pathologic feature in many disease processes, and hence learning the underlying disease process is crucial to guide its management. Clinical features include progressive worsening dyspnea, rales on lung auscultation, and worsening hypoxia. [1]
What is volume overload pulmonary edema?
Cardiogenic or volume-overload pulmonary edema arises due to a rapid elevation in the hydrostatic pressure of the pulmonary capillaries. This is typically seen in disorders involving left ventricular systolic and diastolic function (acute myocarditis including other etiologies of non-ischemic cardiomyopathy, acute myocardial infarction), valvular function (aortic/mitral regurgitation and stenosis in the moderate to the severe range), rhythm (atrial fibrillation with a rapid ventricular response, ventricular tachycardia, high degree, and third-degree heart block). [2]
What is noncardiogenic pulmonary edema?
Noncardiogenic pulmonary edema is caused by lung injury with a resultant increase in pulmonary vascular permeability leading to the movement of fluid, rich in proteins , to the alveolar and interstitial compartments. Acute lung injury with severe hypoxemia is referred to as acute respiratory distress syndrome (ARDS) and is seen in various conditions directly affecting the lungs, such as pneumonia, inhalational injury, or indirectly, such as sepsis, acute pancreatitis, severe trauma with shock, multiple blood transfusions. [3]
How many people are diagnosed with pulmonary edema each year?
More than 1 million patients are admitted each year with a diagnosis of pulmonary edema secondary to cardiac causes (heart failure).[4] An estimated 190,000 patients are diagnosed with acute lung injury each year.[5] About 1.5 to 3.5 cases/100,000 population are diagnosed with ARDS.
Why does my sputum have pink froth?
Cough with pink frothy sputum noted due to hypoxemia from alveolar flooding and auscultation of an S3 gallop could suggest cardiogenic edema. Similarly, the presence of murmurs, elevated jugular venous pressure, peripheral edema may point towards a cardiac etiology.
Can pulmonary edema cause fever?
In patients with non-cardiogenic pulmonary edema , the symptoms of infections such as fever, cough with expectoration, dyspnea pointing to likely pneumonia, recent trauma, blood transfusions should be carefully assessed as these patients may progress to acute respiratory distress syndrome.
Is pulmonary edema a noncardiogenic etiology?
In noncardiogenic etiologies, the edema pattern is typically patchy and peripheral that can demonstrate the presence of ground-glass opacities and consolidations with air bronchograms.[10] Pleural effusions are more commonly seen in the cardiogenic type. [1]
Overview
Symptoms
Causes
Risk Factors
Complications
Prevention
- Pulmonary edema signs and symptoms may appear suddenly or develop over time. The signs and symptoms you have depends on the type of pulmonary edema.