- Grab a 20-mL (or 30-mL) syringe.
- Draw up the adenosine AND the normal saline in the same 20-mL syringe.
- Administer via fast IV push (can be through a running IV line).
How do you administer adenosine IV?
How to Administer Adenosine. So the best way to give Adenosine is in a large bore IV located at or above the antecubital but not below the wrist. If possible, you will want to push the medication with a stopcock attached to the hub of the catheter rather than through a J-loop or any other extended IV tubing.
What is the best way to give adenosine?
So the best way to give Adenosine is in a large bore IV located at or above the antecubital but not below the wrist. If possible, you will want to push the medication with a stopcock attached to the hub of the catheter rather than through a J-loop or any other extended IV tubing.
How is adenosine administered for SVT?
Administration Adenosine is administered intravenously in specific clinical cases. For the management of SVT, adenosine is ideally given through a peripheral intravenous (IV) access initially as a 6 mg dose followed by a 20 mL saline flush for rapid infusion. Subsequent doses start at 12 mg, also followed by 20-mL of saline for rapid infusion.[6]
How do you administer adenosine with a saline flush?
Draw up 6 mg of adenosine in a 2 – 5ml syringe. Draw up a 20 ml Normal Saline flush. Connect the adenosine syringe to the top port of the cannula and the Saline flush to the back port. Administer the adenosne syringe first and as fast as possible. Immediately follow the adenosine with the NS Flush. Observe the rhythm.
See more

How fast do you push IV adenosine?
The first dose of adenosine should be 6 mg administered rapidly over 1-3 seconds followed by a 20 ml NS bolus. If the patient's rhythm does not convert out of SVT within 1 to 2 minutes, a second 12 mg dose may be given in a similar fashion. All efforts should be made to administer adenosine as quickly as possible.
Do you give adenosine fast or slow?
For the management of SVT, adenosine is ideally given through a peripheral intravenous (IV) access initially as a 6 mg dose followed by a 20 mL saline flush for rapid infusion. Subsequent doses start at 12 mg, also followed by 20-mL of saline for rapid infusion.
How is adenosine pushed?
There are a variety of methods to administer adenosine. Some will push it through a running IV line, followed by two 10-mL saline flushes. Others will utilize a stopcock, where the adenosine is hooked up to one port and a 10-mL saline flush is hooked up to the other.
Do you dilute adenosine?
There has been provider concern that diluting adenosine prior to administration could reduce the drug's efficacy. Our results counter this argument and show that the SS method is highly effective with a 73% chance of successful NSR conversion with first dose of adenosine and 100% chance with repeat doses.
What is the first line treatment for SVT?
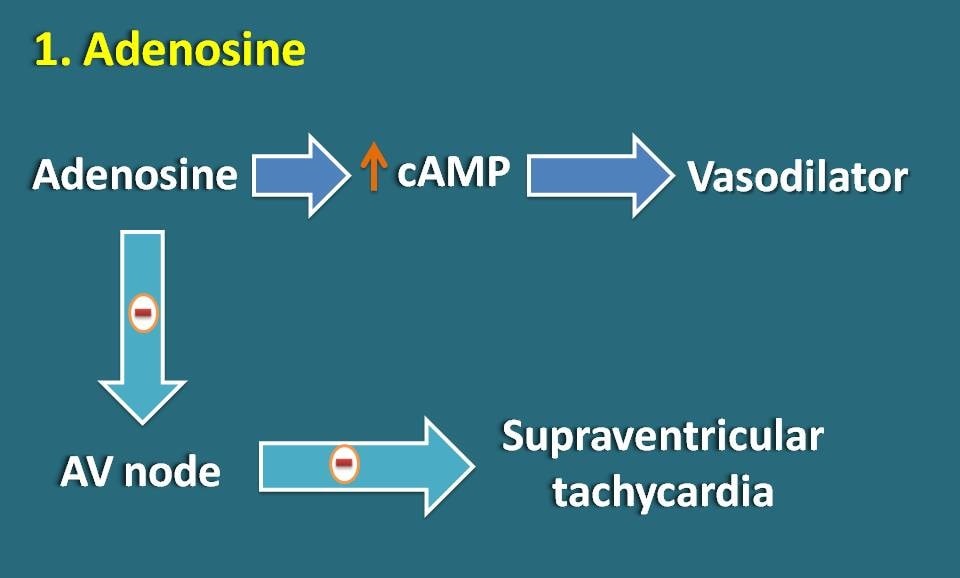
Adenosine (Adenocard) Adenosine is the first-line medical treatment for the termination of paroxysmal SVT. It is a short-acting agent that alters potassium conductance into cells and results in hyperpolarization of nodal cells.
What are the key nursing considerations when administering adenosine?
Nursing considerationsContinuous ECG printout during and immediately after administration IS ESSENTIAL. ... Where practical record blood pressure prior to first dose.Continuous cardio-respiratory monitoring. ... Monitor and assess patient response to therapy.Observe for signs of adverse effects and arrhythmias.More items...•
Why do you flush adenosine?
Adenosine is frequently used to convert supraventricular tachycardia (SVT) to sinus rhythm. Because it has a half-life of <10 seconds, administration is typically followed by a saline flush to deliver the medication bolus to the heart quickly.
Which arm is adenosine?
For two groups of treatment methods, the standard method (control group) was defined as intravenous adenosine through a right cubital vein or as proximal as heart by T-connector or stopcock.
When do you give adenosine for SVT?
Adenosine should be used for regular tachycardias only! It can be dangerous in the setting of atrial fibrillation and Wolff-Parkinson-White Syndrome. Record a 12-lead ECG whenever possible prior to treating a narrow complex tachycardia with adenosine.
How much do you flush adenosine with?
Typically, adenosine is administered as an initial 6mg rapid IV bolus over 1 – 2 seconds followed by a rapid 10 – 20mL saline flush.
Does adenosine drop BP?
Adenosine lowers blood pressure (top), heart rate (middle), and renal sympathetic nerve activity (RSNA) (bot- tom) in this model These effects are similar to those obtained with excitatory amino acid glutamate.
How do you bear down for SVT?
Vagal maneuvers that you can try to slow your fast heart rate include:Bearing down. Bearing down means that you try to breathe out with your stomach muscles but you don't let air out of your nose or mouth.Putting an ice-cold, wet towel on your face.Coughing or gagging.
How to administer adenosine?
Adenosine should be administered by rapid intravenous (IV) bolus injection into a vein or into an IV line. If given into an IV line it should be injected through as proximally as possible, and followed by a rapid saline flush.
How long does adenosine infusion take?
1. Adenosine Infusion should be administered undiluted as a continuous peripheral intravenous infusion at a dose of 140 µg/kg/min for six minutes using an infusion pump. Separate venous sites for Adenosine Infusion and radionuclide administration are recommended to avoid an adenosine bolus effect. 2.
Does adenosine slow cardiac conduction?
When given as a rapid IV bolus, adenosine slows cardiac conduction particularly affecting conduction through the AV node. In light of this adenosine should be administered by RAPID intravenous bolus so that a significant bolus of adenosine reaches the heart before it is metabolized.
Can you use adenosine for atrial fibrillation?
Patients with irregular heart rates, especially atrial fibrillation, patients with PSVT mimics such as atrial flutter with 2:1 conduction or sinus tachycardia in a dehydrated or stressed patient should never receive adenosine. Adenosine should never be used in wide irregular tachycardias.
Usual Adult Dose for Radionuclide Myocardial Perfusion Study
0.14 mg/kg/min infused over 6 minutes (total dose of 0.84 mg/kg) Comments: -Administer only as a continuous peripheral IV infusion. -Inject thallium 201 at the infusion midpoint; may inject directly into the adenosine infusion set as close to venous access as possible to prevent inadvertent increase in the adenosine dose (the contents of the intravenous tubing). Use: Adjunct to thallium 201 myocardial perfusion scintigraphy in patients unable to exercise adequately..
Usual Adult Dose for Supraventricular Tachycardia
Initial dose: 6 mg IV bolus over 1 to 2 seconds Repeat dose: If initial dose fails to eliminate supraventricular tachycardia within 1 to 2 minutes: 12 mg IV bolus over 1 to 2 seconds; may repeat a second time if required Maximum dose: 12 mg Comments: -For rapid IV bolus only; should be given peripherally. -Administer directly into a vein or, if given into an IV line, as close to the patient as possible followed by a rapid saline flush. -This drug does not convert atrial flutter, atrial fibrillation, or ventricular tachycardia to normal sinus rhythm; when atrial flutter or fibrillation is present, a transient modest slowing of ventricular response may occur immediately after administrating this drug. Use: Conversion to sinus rhythm of paroxysmal supraventricular tachycardia (PSVT), including that associated with accessory bypass tracts (Wolff-Parkinson-White Syndrome).
Usual Adult Dose for Wolff-Parkinson-White Syndrome
Initial dose: 6 mg IV bolus over 1 to 2 seconds Repeat dose: If initial dose fails to eliminate supraventricular tachycardia within 1 to 2 minutes: 12 mg IV bolus over 1 to 2 seconds; may repeat a second time if required Maximum dose: 12 mg Comments: -For rapid IV bolus only; should be given peripherally. -Administer directly into a vein or, if given into an IV line, as close to the patient as possible followed by a rapid saline flush. -This drug does not convert atrial flutter, atrial fibrillation, or ventricular tachycardia to normal sinus rhythm; when atrial flutter or fibrillation is present, a transient modest slowing of ventricular response may occur immediately after administrating this drug. Use: Conversion to sinus rhythm of paroxysmal supraventricular tachycardia (PSVT), including that associated with accessory bypass tracts (Wolff-Parkinson-White Syndrome).
Usual Pediatric Dose for Supraventricular Tachycardia
LESS THAN 50 KG: Initial dose: 0.05 to 0.1 mg/kg IV bolus over 1 to 2 seconds Repeat dose: If initial dose fails to eliminate supraventricular tachycardia within 1 to 2 minutes, repeat at incrementally higher doses, increasing by 0.05 to 0.1 mg/kg, until sinus rhythm or maximum single dose attained 50 KG OR MORE: Initial dose: 6 mg IV bolus over 1 to 2 seconds Repeat dose: If initial dose fails to eliminate supraventricular tachycardia within 1 to 2 minutes: 12 mg IV bolus over 1 to 2 seconds; may repeat a second time if required Maximum dose: 0.3 mg/kg; 12 mg Comments: -For rapid IV bolus only; may be given centrally or peripherally. -Administer directly into a vein or, if given into an IV line, as close to the patient as possible followed by a rapid saline flush. -Follow each bolus with a saline flush. -This drug does not convert atrial flutter, atrial fibrillation, or ventricular tachycardia to normal sinus rhythm; when atrial flutter or fibrillation is present, a transient modest slowing of ventricular response may occur immediately after administrating this drug. Use: Conversion to sinus rhythm of paroxysmal supraventricular tachycardia (PSVT).
Precautions
Adenoscan (R) safety and efficacy have not been established in patients younger than 18 years. Consult WARNINGS section for additional precautions.
Other Comments
General: -Overdose: In clinical trials, theophylline 50 to 125 mg slow IV injection was used to treat delayed or persistent adverse reactions.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.