When a patient is in PEA, the ECG monitor can display normal or wide QRS complexes, as well as other abnormalities, which include:
- Low or high-amplitude T-waves
- Prolonged PR and QT intervals
- Atrioventricular disassociation
- Complete heart block
- Ventricular complexes without P-waves
...
Rules for PEA and Asystole.
| PEA Regularity | Any rhythm including a flat line (asystole). |
|---|---|
| QRS | Possible QRS complex or none detectable. |
What types of rhythms are not associated with pea?
Examples include sinus rhythm, atrial fibrillation, bundle branch blocks, or idioventricular rhythms (a rhythm where you would expect and pulse and there is none). Rhythms which are pulseless, such as ventricular fibrillation, pulseless ventricular tachycardia, and asystole, are not associated with PEA.
How is pea interpreted on an ECG?
The ECG interpretation for a patient exhibiting signs of PEA could be the same as normal sinus rhythm. For this reason, treating the patient’s symptoms, particularly when it comes to pulseless electrical activity, is vitally important. Rather than merely reacting to and relying on the rhythms that are being displayed on the ECG monitor.
What is a pea arrest rhythm?
Characteristics of the PEA arrest rhythm may help with determining who would benefit from aggressive postcardiac care interventions such as therapeutic hypothermia. 2,8,18,9 Even though most providers define PEA as an electrical rhythm with absent mechanical activity, Mehta further delineated PEA into pseudo-PEA and true PEA.
What does pea stand for?
Pulseless Electrical Activity (PEA) Algorithm 1 What is PEA. PEA is the abbreviation for a type of cardiac arrest known as pulseless electrical... 2 Signs and Symptoms of PEA. With PEA, the heart muscle is completely disassociated from... 3 PEA Treatment. Of the H’s and T’s, the most common potentially reversible causes...

How do you know if a rhythm is PEA?
The only way to know if a stopped heart involves PEA is with an electrocardiogram, which isn't always available outside of a hospital setting. Fortunately, the treatment for cardiac arrest is always the same, regardless of whether or not PEA is involved.
How does PEA present on ECG?
The electrocardiogram (ECG) interpretation displays heart rhythm activity with similarities to a normal sinus rhythm, but the patient has no palpable pulse. In PEA, the heart's electrical activity is present, but the heart muscle is not responding to the electrical impulses.
Which are characteristics of PEA or pulseless electrical activity?
Pulseless electrical activity (PEA), also known as electromechanical dissociation, is a clinical condition characterized by unresponsiveness and impalpable pulse in the presence of sufficient electrical discharge.
What is the difference between PEA and asystole?
Know the Difference Between PEA and Asystole Asystole is the flatline reading where all electrical activity within the heart ceases. PEA, on the other hand, may include randomized, fibrillation-like activity, but it does not rise to the level of actual fibrillation.
How can you identify a pulseless ventricular tachycardia on an ECG?
Electrophysiology identifying factors for pulseless ventricular tachycardia include; tachycardia (>100 bpm), wide QRS complexes (> 120 milliseconds), atrioventricular (AV) dissociation, presence of fusion or capture beats and an electrical axis between -90 to -180.
What are the 6 causes of pulseless electrical activity?
Various causes of pulseless electrical activity include significant hypoxia, profound acidosis, severe hypovolemia, tension pneumothorax, electrolyte imbalance, drug overdose, sepsis, large myocardial infarction, massive pulmonary embolism, cardiac tamponade, hypoglycemia, hypothermia, and trauma.
What is the difference between ventricular fibrillation and PEA?
VF was defined as a pulseless condition with characteristic features on the cardiac recording performed by EMS. PEA was defined as the absence of a palpable pulse with the appearance of an organized electric rhythm on cardiac monitoring. Asystole was defined as the absence of electric activity on cardiac monitoring.
Does no pulse mean no heartbeat?
During cardiac arrest, an electrical problem makes your heart stop pumping blood to your body. Without blood flowing, you become unconscious and don't have a pulse.
Can you have a blood pressure with PEA?
Pulseless electrical activity is diagnosed based on a patient having an organized, non-shockable rhythm and no palpable pulse. However, PEA is not always a cardiac arrest state. In many cases, patients with PEA have underlying cardiac activity and detectable arterial blood pressure.
Do you defibrillate PEA?
Rhythms that are not amenable to shock include pulseless electrical activity (PEA) and asystole. In these cases, identifying primary causation, performing good CPR, and administering epinephrine are the only tools you have to resuscitate the patient.
What are the 3 non shockable rhythms?
The two nonshockable rhythms are pulseless electrical activity (PEA) and asystole and the two shockable rhythms are pulseless ventricular tachycardia and ventricular fibrilation.
Is there a pulse with PEA?
Pulseless electrical activity (PEA) is a clinical condition characterized by unresponsiveness and the lack of a palpable pulse in the presence of organized cardiac electrical activity. Pulseless electrical activity has previously been referred to as electromechanical dissociation (EMD).
What does sinus bradycardia look like on an ECG?
0:091:37Sinus Bradycardia ECG - EMTprep.com - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo as you'll recall from our other video a normal sinus rhythm is a rate between 60 and 100 beatsMoreSo as you'll recall from our other video a normal sinus rhythm is a rate between 60 and 100 beats per minute with a p-wave normal QRS the T wave sinus bradycardia is going to be a essentially.
What is the heart rate in PEA?
Pulseless electrical activity frequently manifests as a very slow QRS complex with heart rates less than 40 beats per minute.
What is true PEA?
True PEA represents a more severe pathophysiology in which there is a complete absence of mechanical contractions—a true uncoupling of cardiac mechanical activity from the cardiac rhythm. 11 Unlike the reduced aortic pressures of pseudo-PEA, true PEA is characterized by the absence of any aortic pulse pressures. 11 True PED is characterized by profoundly slow rhythms with wide QRS complexes. 11 The electrical component is characterized by an abnormal automaticity, usually seen at a slow ventricular rate with a wide QRS complex (QRS >0.12 seconds). 11 Etiologies frequently associated with true PEA include large myocardial infarction, multiorgan failure, profound metabolic imbalances such as hyperkalemia, drug overdoses, hypothermia, acidosis, and prolonged cardiac arrest. 11
What is PEA in cardiac arrest?
PEA, formerly known as electromechanical dissociation, occurs in patients who have organized cardiac electrical activity without a palpable pulse. 11 The absence of mechanical contractions is produced by factors that deplete myocyte high-energy phosphate stores and inhibit myocardial fiber shortening, including hypoxia, ischemia, metabolic acidosis, and ionic perturbations (particularly potassium and calcium changes). 14 All cardiac arrest rhythms—that is, pulseless rhythms—that fall outside the category of pulseless ventricular tachycardia, ventricular fibrillation, or asystole are considered pulseless electrical activity. 11
How common is a PEA in hospital?
Several studies have shown the incidence of PEA in-hospital to be approximately 35% to 40% of arrest events. 20,15 For out-of-hospital cardiac arrest, the incidence of PEA is 22% to 30%. 5,6 PEA arrests are associated with a poor prognosis, with a survival to discharge rate between 2% and 5% for out-of-hospital cardiac arrest. 17,3 In addition, pulseless electrical activity after countershock is correlated with a worse prognosis than PEA presenting as the initial rhythm, with 0% to 2% of patients in post-countershock PEA surviving to discharge. 13 Furthermore, post-countershock PEA with a slow and wide complex rhythm is associated with a worsened prognosis compared to the rapid, narrow complex PEA. 11
What is pseudo PEA?
Pseudo-PEA is a profound state of cardiogenic shock that is inadequate to maintain perfusion pressure (and thus a nondetectable pulse). 11 Pseudo-PEA has the presence of aortic pulse pressures with a perfusion pressure less than 60 mm Hg. 14 In pseudo-PEA, cardiac electrical activity is present with myocardial contractions that are not adequate to produce a palpable pulse. 11 Pseudo-PEA is a form of severe shock in which diminished coronary perfusion leads to decreased myocardial function, thus further propagating hypotension. 14 The pathologic insult causing the pseudo-PEA impedes the cardiovascular system’s ability to provide circulation throughout the body. 11 In the spectrum of PEA etiologies, pseudo-PEA is frequently caused by hypovolemia, tachydysrhythmias, decreased cardiac contractility, or obstructions to circulation, such as pulmonary embolism, tamponade, and tension pneumothorax. 4 Pseudo-PEA rhythms are often narrow QRS complex tachycardias. 11
What is PEA treatment?
PEA is a disease process with multiple etiologies, and effective treatment likely includes reversing the cause of cardiac arrest. 7 Understanding the potential pulseless electrical activity causes and treatments will enable providers to give the best possible care in a situation that statistically does not have positive outcomes.
What is a PEA?
PEA is the abbreviation for a type of cardiac arrest known as pulseless electrical activity. PEA is an organized rhythm without a pulse where the electrical activity of the heart may appear normal, but the heart muscle is not responding. Performing high quality CPR is the initial treatment for PEA. In addition to CPR, identifying underlying causes ...
How to treat PEA?
PEA is not a shockable rhythm and treatment for PEA involves high quality CPR, airway management, IV or IO therapy, and appropriate medication therapy . The primary medication is going to be 1mg epinephrine 1:10,000 every 3-5 minutes rapid IV or IO push. In order to correct PEA, the ultimate goal is to identify and treat the underlying cause of the cardiac arrest.
What is Pulseless Electrical Activity (PEA)?
Pulseless electrical activity, also commonly referred to as PEA, is a condition where the electrical activity of the heart isn’t accompanied by a palpable or effective pulse. Healthcare providers need to find the potential cause and correct it, which will hopefully restore the patient’s pulse.
What happens if you have a PEA?
A patient with PEA will be unconscious with no pulse or normal breathing. Pulseless electrical activity leads to a loss of cardiac output and discontinues blood supply to the brain. The skin may appear pallor due to a lack of oxygen in the blood.
What are the two pathways for cardiac arrest?
The algorithm consists of the two pathways for a cardiac arrest: Common medications used to treat VFib or pulseless V-tach include: Other medications, depending on the cause of the V-tach or pulseless V-tach arrest. Common medications used to treat asystole and pulseless electrical activity include:
What is the meaning of PEA?
Signs and Symptoms of Pulseless Electrical Activity (PEA) A patient with PEA will be unconscious with no pulse or normal breathing. Pulseless electrical activity leads to a loss of cardiac output and discontinues blood supply to the brain. The skin may appear pallor due to a lack of oxygen in the blood.
What is the most important algorithm for adult resuscitation?
The adult cardiac arrest algorithm is the most important algorithm for adult resuscitation. This algorithm outlines all of the assessment and management steps ACLS providers will need to know for all pulseless patients who do not initially respond to basic life support interventions, including the first shock from an AED.
What causes a PEA?
Hypoxia is one of the most common causes of PEA, leading to an estimated 1/2 of PEA events. With oxygen cut off, the heart no longer has the means with which to contract, even if the heart were otherwise fully capable of a contraction with electrical stimulation from an AED. Unless the oxygen is restored, the heart muscle will die, and death results. This patient probably needs intubation before shock will have an effect.
What is the defining factor of a PEA arrest?
The defining factor is that in PEA arrests, there really is no pulse. There is no cardiac output. There is cardiac activity, but for some reason that activity is fruitless.
How Common Is PEA Arrest?
PEA arrests are a surprisingly common occurrence in the hospital setting.
How Is PEA Treated?
If the PEA arrest is among the H and T, then it may be reversible. But you must treat the cause of the PEA arrest to reverse the state and obtain a shockable rhythm.
What Are Shockable vs. Non-shockable Rhythms?
A shockable rhythm is one caused by abnormalities in the electrical conduction in the heart. These include:
What Happens If You Shock PEA? Why not shock a PEA Arrest?
In a PEA arrest, similar to Asystole, the heart doesn’t have the means to use the shock you’re sending it because the primary cause has yet to be corrected.
What is a PEA arrest?
A PEA arrest is the first documented rhythm in as many as 38% of adults experiencing hospital cardiac arrest (IHCA).
What is a PEA?
PEA is one of many waveforms by ECG (including sinus rhythm) without a detectable pulse. PEA may include any pulseless waveform with the exception of VF, VT, or asystole (Figure 28). Hypovolemia and hypoxia are the two most common causes of PEA.
Can you take atropine during a PEA?
NO ATROPINE DURING PEA OR ASYSTOLE. Although there is no evidence that atropine has a detrimental effect during bradycardia or asystolic cardiac arrest, routine use of atropine during PEA or asystole has not been shown to have a therapeutic benefit.
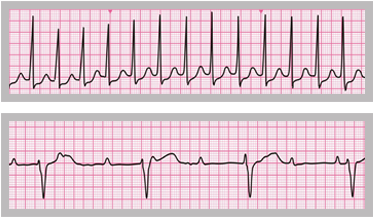
Is asystole a pulseless pulse?
Pulseless electrical activity (PEA) and asystole are related cardiac rhythms in that they are both life-threatening and unshockable cardiac rhythms. Asystole is a flat-line ECG (Figure 27). There may be a subtle movement away from baseline (drifting flat-line), but there is no perceptible cardiac electrical activity. Always ensure that a reading of asystole is not a user or technical error. Make sure pads have good contact with the individual, leads are connected, the gain is set appropriately, and the power is on. PEA is one of many waveforms by ECG (including sinus rhythm) without a detectable pulse. PEA may include any pulseless waveform with the exception of VF, VT, or asystole (Figure 28).
