Angle the tip of the otoscope towards the person’s nose. This follows the normal angle of the ear canal. From here, move the otoscope gently at different angles. This allows you to view the person’s eardrum and canal walls.
How do you assess the appearance of a nose?
Inspect the nose for any deformity, asymmetry, inflammation, or skin lesions (Jarvis, 2011). Test the patency of the nostrils by pushing each nostril wing shut with your finger while asking the patient to sniff inward. View each nasal cavity with the person’s head erect and then with the head tilted back (Jarvis, 2011).
How should I approach the examination of a patient with nasal polyps?
Approach the examination in a systematic way, but be prepared to be instructed to move on quickly to certain sections by any examiner. Inspect the external nose, both anteriorly and laterally for: Ask the patient to tilt their head back (or gently tip the end of the nose up) and inspect the anterior nares; use a pen torch or otoscope if necessary.
How do you check for a dislocated nose?
Internal. Carefully elevate the tip of the nose with your thumb, so that the nasal cavity becomes visible. Use a pen torch or otoscope as a light source to externally illuminate the cavity (elevating the tip of the nose will also assess for columellar dislocation). 4. Inspect the nasal mucosa for any abnormalities (including the septum).
How do you use an otoscope for a hearing test?
Angle the otoscope. Angle the tip of the otoscope towards the person’s nose. This follows the normal angle of the ear canal. From here, move the otoscope gently at different angles. This allows you to view the person’s eardrum and canal walls. Stop the exam at any sign of increased pain or discomfort.
How do you examine a nose with an otoscope?
Inspect inside of nose with otoscope with largest ear speculum. Tilt patient's head back slightly and insert speculum gently into vestibule of each nostril. Avoid contacting nasal septum as this is a sensitive area. Hold otoscope handle to one side to avoid patient's chin and improve mobility.
How do you inspect nose?
Method Of ExamA large otoscope.A speculum.Or by tilting the tip of nose with pen light.Observe and describe the following. Describe the position and contour of the septum. Note the color of the mucous membrane. Inspect the inferior and middle turbinates. Identify drainage sites of maxillary and ethmoid sinuses.
How do you assess sinus and nose?
Steps to palpate the nose and sinuses include:With your thumb, gently palpate one sinus at a time. Use a circular motion to palpate. ... Palpate the nose for airflow/patency. ... Gently palpate the external nose if trauma/injury or lesions are present. ... Note the findings:
What should you look for when assessing your nose?
Nose ExaminationNote any deformities or asymmetry of the nose.When inspecting the nasal vestibule, note the color of the nasal mucosa as well as the presence of any bleeding, discharge, or swelling of the mucosa.Note the presence of ulcers, or polyps.
How do you describe nasal mucosa?
The mucosa, or mucous membrane, is a type of tissue that lines the nasal cavity. Mucous membranes are usually moist tissues that are bathed by secretions such as in the nose.
What is patency of the nose?
Patency emanates from the word “patent”, which is equivalent to the word “open”. Nasal patency is thus a measure of how open the nose is, and it is not equivalent to airflow or resistance to airflow.
What are two physical assessment techniques do we use for the sinuses?
Besides the history and physical examination, the primary diagnostic aids for sinusitis are radiologic imaging and nasal endoscopy.
What sinuses can be assessed through examination?
Only the frontal and maxillary sinuses are accessible for clinical exam. Physical assessment of the paranasal sinuses, along with the patient's signs and symptoms, can help you to identify certain conditions such as acute sinusitis involving the frontal or maxillary sinuses.
How does the nurse check for nasal patency?
Nasal Patency. Check the patency of each naris by standing directly in front of the patient and occluding the patient's left naris with the index finger of your right hand. Ask the patient to breathe normally through the right naris.
How do you know if its sinuses?
Common signs and symptoms of sinusitis include: Post nasal drip (mucus drips down the throat). Nasal discharge (thick yellow or green discharge from nose) or stuffy nose. Facial pressure (particularly around the nose, eyes, and forehead), headache and or pain in your teeth or ears.
Where to insert otoscope?
Insert the otoscope slowly into the ear canal. Place the otoscope at your patients ear, not in it. [6]
How to hold otoscope?
Handle the otoscope properly. Turn the otoscope’s light on and hold your otoscope “upside down” between your thumb and pointer finger like a pen or pencil. Place the back of your hand along the person’s cheek so that otoscope is steady and braced. While the position may feel awkward at first, it soon will feel natural.
What is an otoscope?
This article has been viewed 33,736 times. An otoscope is a medical instrument used by a doctor to examine the ear. The otoscope magnifies the inside of the ear to detect problems or issues with the outer and middle ears, such as Swimmers ear, earwax build-up, or otitis media. It generally has a magnifying glass, ...
How to straighten ear canal?
Straighten the ear canal. Use your opposite hand to gently pull the outer ear up and back on patients older than 12 months. Straightening your patient’s ear canal can make it easier to examine the ears. Pull the outer ear down for babies and children younger than 3 years old.
How to treat ear infection?
The ear is a very sensitive organ and can injure easily if improperly examined. Avoid pulling, pushing, or generally being rough with the patient you are examining. This can calm your patient and minimize the risk of injury from sudden movements.
What to ask a patient about pressure?
Ask your patient if the pressure is acceptable to them. For example, “Is the pressure I’m using ok, Mr. Neumaier? Let me know if you have any discomfort.”
Can you use an otoscope with caution?
Use caution with an otoscope. Your doctor is trained in proper techniques and can minimize the risk of injury from improper use.
How to inspect nose?
General Inspection. Begin with an overall inspection of the nose. Evaluate the size and shape. Lift the lip of the nose with a gloved thumb to obtain a better view and observe the colour and texture of the skin. Butterfly rash over the nasal bridge.
What is anterior rhinoscopy?
Anterior rhinoscopy. Deliberately and systematically inspect the roof of the nose and along the floor of the nose. Make a note of any particular dryness but remember that as the patient ages, the tendency is for the nose to become gradually dry.
Does nose get dry as you age?
Make a note of any particular dryness but remember that as the patient ages, the tendency is for the nose to become gradually dry.
How to open nose with head lamp?
Nasal Cavity. Use a head lamp with a nasal speculum to gently open up the nose. Place the index finger in the middle of the speculum. Use your middle and ring finger to support the speculum on each side.
How to check anterior nares?
Ask the patient to tilt their head back (or gently tip the end of the nose up) and inspect the anterior nares; use a pen torch or otoscope if necessary. Check for the same characteristics as listed above.
Where to inspect nose?
Inspect the external surface of the nose from the front, side and behind the patient to identify any abnormalities.
How to see a patient's nasal cavity?
Nasal cavity. Sit facing the patient with your knees together and to one side of the patient’s knees. Ask the patient to look forward, keeping their head in a neutral position. Carefully elevate the tip of the nose with your thumb, so that the nasal cavity becomes visible.
What does it mean when your nose is reducing airflow?
Reduced airflow through a particular nostril may indicate the presence of something blocking that air passage, such as a polyp, deviated nasal septum or foreign body.
What is the function of turbinates in the nose?
The turbinates are projections of bone which are covered in nasal mucosa and control airflow through the nose, exposing it to a large surface area of mucosa which both warms and cleans the air prior to it arriving at the lungs.
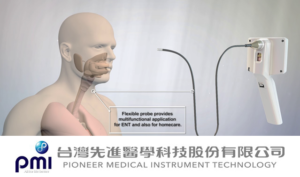
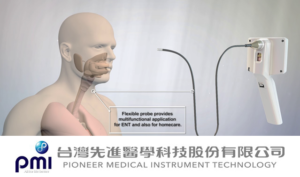
What is the name of the otoscope with a large speculum?
Nasal speculum (also known as Thudiculum’s speculum) or an otoscope with a large speculum.
What is the speculum attached to the nose called?
Further assessment can be performed using an otoscope with a large speculum attached (inserting only the very tip into the nose) or using a nasal speculum (also known as Thudiculum’s speculum) which widens the nasal cavity to allow you to peer in using a light source.
What is the nasal septum?
The nasal septum is the bone and cartilage in the nose that separates the nasal cavity into the two nostrils. The nasal vestibule is the most anterior part of the nasal cavity. It is enclosed by the cartilages of the nose and lined by the same epithelium as the skin.
What is an otoscope exam?from ncbi.nlm.nih.gov
The otoscope exam helps to assess the condition of the external auditory canal (EAC), tympanic membrane (TM), and the middle ear. Mastering the otoscope exam leads to accurate diagnoses, allowing for targeted treatment and prevention of complications. Early stages of otologic diseases can be present in the absence of complaints such as ear pain, ear fullness, and hearing loss.
Why is otoscopy important for otitis media?from ncbi.nlm.nih.gov
A normal TM will respond by concaving into the middle ear cavity. The most common cause of decreased TM mobility is middle ear effusion. Therefore, pneumatic otoscopy aids in the diagnosis of acute o titis media (AOM) and otitis media with effusion (OME). Recent clinical practice guidelines report that AOM should not receive a diagnosis without evidence of middle ear effusion shown by pneumatic otoscopy. Other causes of decreased TM mobility are tympanosclerosis, TM retraction, and TM perforation. [8][9][10][11][12][13]
What is MOE in otoscope?from ncbi.nlm.nih.gov
MOE, severe sequelae of OE, is an invasive infection of the EAC and skull base. Early diagnosis is critical; therefore, MOE should be a consideration with any patient with refractory OE, fever above 39 C, diabetes mellitus, or immunosuppression. On the otoscope exam, granulation tissue is visible along the floor of the EAC at the bony-cartilaginous junction (i.e., isthmus). Cranial nerve exams are warranted when evaluating for MOE. Spread to the stylomastoid foramen can present with facial nerve palsy. Spread to the jugular foramen can present with glossopharyngeal, vagus, or accessory nerve palsies. MRI and CT (without contrast) scans are useful in diagnosis, with CT being more sensitive for bone erosion. The mainstay treatment for MOE is culture-sensitive long-term antibiotic therapy, and in some cases, surgical debridement. [27][28][29]
How does an ear exam work?from healthline.com
How is an ear examination performed? Your doctor may dim the lights in the exam room to make it easier to see your ear canal and eardrum with an otoscope. An otoscope is a handheld light with a removable plastic tip shaped like a cone that allows the doctor to look inside your ear. Your doctor will gently pull in the following directions ...
What is the pain of an ear exam?from healthline.com
chronic ear infections. a punctured eardrum. An ear exam may be slightly uncomfortable or painful if you have an ear infection. Your doctor will stop the exam and remove the otoscope if the pain worsens.
What are the symptoms of ear infection?from healthline.com
Your doctor will perform an ear examination, or otoscopy, if you have: 1 an earache 2 an ear infection 3 hearing loss 4 ringing in your ears 5 any other ear-related symptoms
Why does my eardrum light not reflect?from healthline.com
If the light doesn’t reflect off of your eardrum, it’s another indication that fluid may have collected behind the eardrum due to an infection.
How to tell if otoscope is working?
You can test if the otoscope is functioning properly by viewing print from a magazine or newspaper and measuring the approximate distance the otoscope tip is away from the print when everything is in clear focus. It should be somewhere between ½-3/4 inch away. The print should also be very clear and not distorted.
How to use an otoscope to see the eardrum?
The best way to practice using your otoscope is with the help of an adult volunteer who has ear canals relatively free of ceruman (ear wax). To see the eardrum, grasp the outer ear. Gently pull backward and slightly upward on the ear (see ear picture below).
What is the key to doing ear exams?
The key to doing ear exams is practice. The old saying practice makes perfect could not apply more to any situation than it does to doing ear exams. It is important to begin doing otoscope exams on a willing adult as opposed to a child. The ear canals are larger and the eardrum is easier to see in an adult. The key is to look into as many adult ear ...
Why can't I see my eardrum?
BOTTOM LINE: If the light is bright and the focus on the newsprint is clear at 1/2-3/4 inch from the tip of the specula then the reason you are not seeing the eardrum clearly while doing an exam is not the fault of the otoscope. There are other factors causing this (i.e. earwax, debris, or ear canal curvature). If the newsprint is blurry or the light dim then there is a defect in the otoscope.
How to straighten ear canal?
Gently pull backward and slightly upward on the ear (see ear picture below). This will help to straighten the ear canal for the best "line of sight.". Gently insert the otoscope while looking into its lens. You will begin to see when structures inside the ear come into focus.
How far away is the eardrum?
The eardrum is normally around 1 inch away from the entrance to the outer ear in adults and ¾ inch away in small children. When you subtract out the ¼ inch you normally insert the otoscope speculum into the ear canal your focal point should be between ½ and ¾ inches away when you look at the eardrum with the otoscope.
What is external otitis?
External Otitis - Swimmers Ear This is an infection of the ear canal itself. Notice the swelling of the ear canal.
How to palpate sinuses?
Using your thumbs palpate the frontal sinuses by pressing up and under the eyebrows, and over the maxillary sinuses below the cheekbones (Jarvis, 2011). Inspect The Mouth. Inspect the lips for color, moisture, cracking, or lesions. Inspect the teeth and gums.
What equipment is needed for nares?
The equipment needed for the assessment of the nares would include an Otoscope with short, wide-tipped nasal speculum attachment, penlight, two tongue blades, cotton gauze pad, and gloves. Normally the nose should be symmetric, midline, and in proportion to other facial features. Inspect the nose for any deformity, asymmetry, inflammation, ...
What color should tonsils be?
With a light observe the oval rough surfaced tonsils- the color should be pink, with some indentations or crypts. During the exam assess breath odor; halitosis (i.e., foul breath odor) may indicate poor oral hygiene or tooth decay. Assess for problems with speech (e.g., aphasia or dysphasia) or swallowing, which can be the result of stroke or other brain injury.
Nose and Sinuses
Inspection and palpation of the nose should be performed standing directly in front of the client while they are sitting upright on the examination table or a chair. It is important to don gloves as you may be in contact with bodily fluids such as nasal discharge.
Inspection
Normally, the nose is the same colour as the rest of the face with no discolourations such as redness. Describe the appearance and location of any discolourations noted.
Palpation
Begin with the frontal sinuses inferior to the eye brows over the bony ridge. Avoid the eye socket.
