Explore
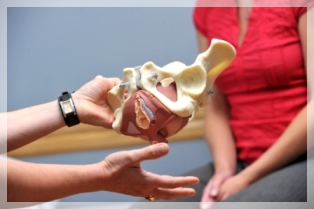
Identifying Pelvic Organ Prolapse By Mary O'Dwyer. When the prolapse skews more to one side, a levator ani tendon tear (from the pubic bone) is suspected. When a vaginal wall bulges into your inserted fingers (and not out of the vaginal entrance), the prolapse is contained internally.
How do you identify a pelvic organ prolapse?
While the spirit may be resilient, the tissue that holds the pelvic organs in place can have a hard time standing up to the demands. Over time, these tissues stretch and become weak. When they do, the bladder, small bowel, rectum or uterus can slip down toward the vagina—a condition known as pelvic organ prolapse (POP).
What is pelvic organ prolapse (POP)?
Pelvic organ prolapse. Overview. When the muscles and ligaments supporting a woman's pelvic organs weaken, the pelvic organs can drop lower in the pelvis, creating a bulge in the vagina (prolapse). Women most commonly develop pelvic organ prolapse years after childbirth, after a hysterectomy or after menopause.
What causes pelvic organ prolapse in women?
When your organs sag or droop out of their normal position, this is called a prolapse. Prolapses can be small—with just a little movement—or large. A small prolapse is called an incomplete prolapse. A bigger prolapse (called a complete prolapse) is one where the organ has shifted significantly out of its normal place.
What is a small prolapse called?

How do I know which pelvic organ prolapse?
Types of prolapse the bladder bulging into the front wall of the vagina (anterior prolapse) the womb bulging or hanging down into the vagina (uterine prolapse) the top of the vagina sagging down – this happens to some women after they have had surgery to remove their womb.
What is the most common organ to prolapse?
Dropped bladder (called cystocele). This is the most common type of pelvic organ prolapse. This happens when the bladder drops into or out of the vagina.
What body parts can prolapse?
The most common organ associated with prolapse is the bladder. Additional organs include the urethra, uterus, vagina, small bowel and rectum. The “dropping” of these organs happens when the muscles that hold these organs get weak or are stretched.
How is prolapsed organ diagnosed?
Tests for pelvic organ prolapse might include:Bladder function tests. Some tests are as simple as finding out whether your bladder leaks when it's put back into place at the time of your physical exam. ... Pelvic floor strength tests. ... Magnetic resonance imaging (MRI). ... Ultrasound.
When should I worry about a prolapse?
A 'heavy', 'dragging' sensation in the vagina. The feeling of 'something coming out' the vaginal passage or an observable bump/lump bulging out of the vagina. Pain with intercourse. Bladder symptoms including: weak urine stream, feelings of incomplete bladder emptying and recurrent urinary tract infections.
How do I know if my prolapse is severe?
Signs and symptoms of moderate to severe uterine prolapse include:Sensation of heaviness or pulling in your pelvis.Tissue protruding from your vagina.Urinary problems, such as urine leakage (incontinence) or urine retention.Trouble having a bowel movement.More items...•
What can be mistaken for prolapse?
The most common disorders that pelvic organ prolapse is mistakenly diagnosed as include urinary and fecal incontinence, constipation, and irritable bowel disease.
What should you not do with a prolapse?
If you have pelvic organ prolapse, avoid things that could make it worse. That means don't lift, strain, or pull. If possible, try not to be on your feet for long periods of time. Some women find that they feel more pressure when they stand a lot.
Can you get a bloated stomach with a prolapse?
Abdominal bloating and/or flatulence can be a huge problem for women with prolapse problems. Some ladies find that by the end of the day their abdomen is so bloated that it puts strain on their belly and their prolapse causing abdominal pain and pelvic floor dragging and bulging.
At what stage of prolapse require surgery?
Consider surgery if the prolapse is causing pain, if you are having problems with your bladder and bowels, or if the prolapse is making it hard for you to do activities you enjoy. An organ can prolapse again after surgery. Surgery in one part of your pelvis can make a prolapse in another part worse.
Can a prolapse correct itself?
Prolapsed organs cannot heal themselves, and most worsen over time. Several treatments are available to correct a prolapsed bladder.
What does a prolapse feel like inside?
Symptoms of vaginal prolapse include the feeling of vaginal pressure or fullness — like you're sitting on a small ball — and the sensation that something has fallen out of your vagina. A cystocele or rectocele usually occurs with vaginal prolapse. Mild cases of vaginal prolapse do not require treatment.
How common is pelvic organ prolapse after hysterectomy?
Information on the rate of post-hysterectomy prolapse varies. The cumulative risk is described as 1% three years after hysterectomy and up to 15% fifteen years later. The risk is 5.5 times higher if hysterectomy was performed because of a descensus situation. Other investigations found an incidence of up to 46%.
How do you fix a prolapse without surgery?
The two non-surgical options for prolapse are pelvic floor muscle training (PFMT) and a vaginal pessary. PFMT can be effective for mild prolapse but is usually not successful for moderate and advanced prolapse. The main alternative to surgery for prolapse is a vaginal pessary.
Overview
When the muscles and ligaments supporting a woman's pelvic organs weaken, the pelvic organs can drop lower in the pelvis, creating a bulge in the vagina (prolapse). Women most commonly develop pelvic organ prolapse years after childbirth, after a hysterectomy or after menopause.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
How Is Pelvic Organ Prolapse Diagnosed?
If you think you may have pelvic organ prolapse, talk to your doctor. They’ll ask about your medical history and examine your pelvic organs to get an idea of how strong your pelvic floor muscles are. It may be all they need to do to make a diagnosis.
What Is Pelvic Organ Prolapse?
"Prolapse" refers to a descending or drooping of organs. Pelvic organ prolapse refers to the prolapse or drooping of any of the pelvic floor organs, including the:
What Is a Pelvic Floor Disorder?
The "pelvic floor" is a group of muscles that form a kind of hammock across your pelvic opening. Normally, these muscles and the tissues surrounding them keep the pelvic organs in place. These organs include your bladder, uterus, vagina, small bowel, and rectum.
What happens to pelvic floor after childbirth?
Sometimes, these muscles and tissues develop problems. Some women develop pelvic floor disorders following childbirth. And as women age, pelvic organ prolapse and other pelvic floor disorders become more common.
What happens when pelvic floor disorders develop?
When pelvic floor disorders develop, one or more of the pelvic organs may stop working properly. Conditions associated with pelvic floor disorders include:
What to do if you think you have pelvic prolapse?
If you think you may have pelvic organ prolapse, talk to your doctor. They’ll ask about your medical history and examine your pelvic organs to get an idea of how strong your pelvic floor muscles are. It may be all they need to do to make a diagnosis.
What is the role of genetics in pelvic prolapse?
Genetics may also play a role in pelvic organ prolapse. Connective tissues may be weaker in some women, perhaps placing them more at risk.
How to detect pelvic organ prolapse?
Many women are interested in learning self-examination skills for detecting pelvic organ prolapse (POP). Self-examination for POP is done in supported lying then standing, with one foot on a stool so gravity helps with assessment. Angle a mirror for observation and keep a pad and pen close to note any findings.
How to tell if a vaginal wall is prolapsed?
A definite bulge of the wall under your fingers indicates a front vaginal wall prolapse.
Why does my uterus prolapse during a lift?
If the PF muscles feel strong and coordinated during the lift, the utero- vaginal prolapse is more likely due to damage of supporting ligaments and connective tissue (rather than muscle weakness). If the cervix descends, a bearing down action is being used. Anterior (front) vaginal wall prolapse:
What happens to PF muscles after postpartum?
Returning to exercise or lifting heavy weights before regaining PF muscle strength and postural alignment postpartum, results in more strain and damage to pre-weakened muscle, supporting ligaments and connective tissue supports.
What causes pelvic floor damage?
Pelvic floor damage occurs when the pelvic floor fatigues part way through a workout. Building abdominal strength with upper abdominal bracing exercises increases intra abdominal pressure that has the potential to overwhelm pelvic floor control.
What happens if you have a larger waist?
Women with a larger waist measurement have a higher risk of pelvic floor dysfunction (incontinence and POP). Visceral fat accumulates internally around the pelvic organs forcing PF muscles to work harder to support the weighted organs.
How to tell if your back vagina is prolapsed?
Insert 1 or 2 fingers and place over the back vaginal wall (facing the rectum), to feel any bulging under your fingers, first with strong coughing and then sustained bearing down. A definite bulge under your fingers indicates a back vaginal wall prolapse.