- Using a booted (or padded) clamp, begin at the dressing and clamp the drainage tubing momentarily.
- Look at the water-seal/air leak meter chamber. Keep moving the clamp down the drainage tubing toward the chest drainage system, placing it at 20 to 30 cm intervals. ...
- When you place the clamp between the source of the air leak and the water-seal/air leak meter chamber, the bubbling will stop. ...
How do you manage a patient with a chest tube?
Prior to managing a patient with a chest tube, review reason for the chest tube, the location of the chest tube, normal volume of drainage, characteristics of the drainage, date of last dressing change, and any previously recorded air leaks measurements.
How do you monitor a chest tube drain?
Chest Tube Drainage System Monitoring and Care 1 Review the doctor’s orders regarding chest tube care. 2 Confirm the patient’s identity using at least two patient identifiers according to your facility’s policy. ... 3 Explain the procedure to the patient. 4 Perform hand hygiene before providing patient care. ... More items...
How do you remove a chest drain from a patient?
Place newly prepared drainage system in a position adjacent to the old system as set up as per chest drain set up. If there are multiple drains insitu, clamp all drains before removal. Instruct patient exhale and hold if they are old enough to cooperate; if not, time removal with exhalation as best as possible.
Can a chest tube be clamped for drainage?
The tube must remain unobscured and unclamped to drain air or fluid from the pleural space. There are a few exceptions where a chest tube may be clamped; see special considerations below. Chest tube drainage systems are replaced only when the collection chamber is full or the system is contaminated.

What are the responsibilities of a nurse to the patient with a chest tube drainage?
Nurses' responsibilities when managing a chest drainObservation of the patient. ... Observations of the drainage system. ... Pain management. ... Suction and chest drains. ... Clamping drains. ... Milking and stripping drainage tubing. ... Changing drainage bottles. ... Drainage tubing.More items...•
What is the nurse's priority assessment when caring for a patient with a chest tube?
What are the nursing responsibilities when caring for a client with a chest tube to a drainage system? Look at the client first- (color, level of consciousness, airway patency, respiratory rate, depth, rhythm, chest movement- symmetry, lung sounds, lips/ nailbeds).
What are the three basic components of a chest tube drainage system?
Three-compartment chest drainage systems They include a collection chamber, a water-seal chamber and a suction control chamber, which are interconnected. Fluid or air drain into the collection chamber.
How do I monitor my chest drain?
Bubbling and swinging should be assessed with the patient deep breathing and if possible coughing. This also has the benefit of assessing adequacy of analgesia. These features indicate that the drain is still functioning. Absence of swinging indicates that the drain is occluded or is no longer in the pleural space.
Can nurses flush chest tubes?
An RN certified in the RNSP (Advanced RN Intervention) Interpleural Irrigation and/ or Medication Administration may irrigate chest tubes when working in their targeted area.
What is the nurse's responsibility during chest tube insertion?
NURSING ALERT: Always keep chest drainage system upright and below the level of patient's chest. and attach new drainage system while submerging distal end of chest tube in sterile water. If there are visible clots in tubing, obtain a physician's order to gently “milk” chest tube.
What color should chest tube drainage be?
The first few days after your surgery, the fluid draining from your chest may be dark red. This is common. As you heal, it may look pink or pale yellow. If fluid is draining from your chest, it will flow through your chest tube and into your Pneumostat's collection chamber.
How much fluid should drain from a chest tube?
The authors conclude that using a drainage threshold of 200 mL per day for chest tube removal in patients with uninfected pleural fluid and no evidence of air leaks may safely decrease costs and length of stay following thoracic operative procedures.
Where should bubbling be in a chest tube?
In summary, in “wet” suction drains, whether evacuating fluid or air, the only chamber that should be constantly bubbling is the suction control chamber when it is attached to the vacuum regulator.
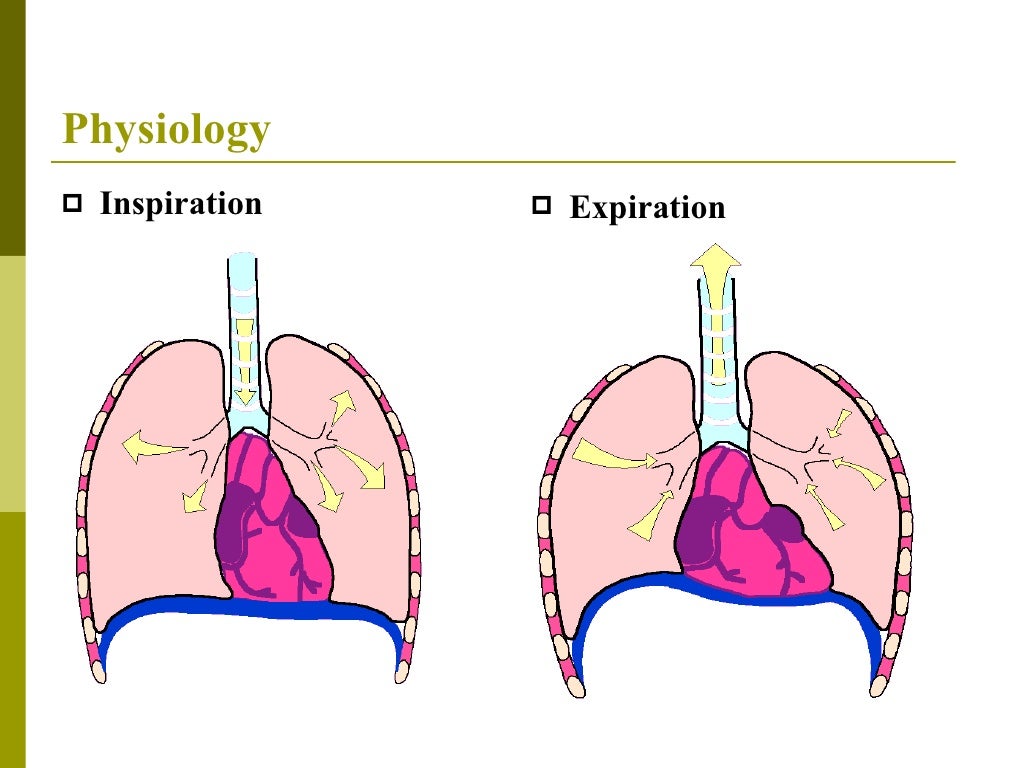
What are the principles of chest drainage?
Negative pressure during inspiration causes water level to rise slightly. Positive pressure during expiration pushes air and fluid out of the pleural space and into the tube and collection bottle. Air bubbles out of tube into the underwater seal. Fluid drains by gravity, mixing with water and raising the fluid level.
How much should a chest tube drain per hour?
The tube will be connected to the chest drainage system and may be connected to suction. In the trauma setting, an initial output of 1500 mL or 200 mL/hr over 4 hours is an indication to perform a thoracotomy since such high output is likely a vascular injury that requires surgical repair.
How do you know if a chest tube has an air leak?
Start by examining the air-leak detection chamber in the water seal of the drainage device. An air leak presents as small air bubbles; the amount of bubbling indicates the degree of the leak. If you notice bubbling, determine location of the leak.
Which of the following are the responsibility of the RN in a client with a chest tube select all that apply?
The nurse is responsible for monitoring and maintaining the chest tube drainage system. This includes recording drainage, monitoring for air leaks or kinks, assessing suction settings, monitoring patient's respiratory status, and assisting the physician with removal of the chest tube.
What should you do first after your patient has a chest tube inserted?
A chest tube drainage system disconnecting from the chest tube inside the patient is an emergency. Immediately clamp the tube and place the end of chest tube in sterile water or NS. The two ends will need to be swabbed with alcohol and reconnected. Bleeding may occur after insertion of the chest tube.
Which of the following is the most appropriate nursing intervention for pneumothorax?
The most important interventions focus on reinflating the lung by evacuating the pleural air. Patients with a primary spontaneous pneumothorax that is small with minimal symptoms may have spontaneous sealing and lung re-expansion.
Which actions when taken by the nurse can prevent chest tube occlusions?
If you see visible clots, squeeze hand-over-hand along the tubing and release the tubing between squeezes to help move the clots into the CDU. As a rule, avoid clamping a chest tube. Clamping prevents the escape of air or fluid, increasing the risk of tension pneumothorax.
What is a chest drain?
Chest drains also known as under water sealed drains (UWSD) are insert ed to allow draining of the pleural spaces of air, blood or fluid, allowing expansion of the lungs and restoration of negative pressure in the thoracic cavity. The underwater seal also prevents backflow of air or fluid into the pleural cavity.
Where is chest drain recorded?
Ensure that Chest Drain is recorded in the EMR under the LDA flowsheet
Why should tubing be secured to patient bed?
Tubing should be anchored to the patient’s skin to prevent pulling of the drain. In PICU and NICU tubing should also be secured to patient bed to prevent accidental removal. Ensure the unit is securely positioned on its stand or hanging on the bed. Ensure the water seal is maintained at 2cm at all times.
What is the valve effect of pneumothorax?
Tension Pneumothorax: One way valve effect which allows air to enter the pleural space , but not leave. Air builds up and forces a mediastinal shift. This leads to decreased venous return to the heart and lung collapse/compression causing acute life-threatening respiratory and cardiovascular compromise. Ventilated patients are particularly high risk due to the positive pressure forcing more air into the pleural space . Tension pneumothorax can result in rapid clinical deterioration and is an emergency situation
What is an under water seal drain?
Under Water Seal Drain (UWSD): Drainage system of 3 chambers consisting of a water seal, suction control and drainage collection chamber. UWSD are designed to allow air or fluid to be removed from the pleural cavity, while also preventing backflow of air or fluid into the pleural space
How to collect fluid from a tubing?
Procedure: Wait for the fluid to collect in a loop of the tubing. Perform hand hygiene, then don gloves & eye protection. Clean the sampling port, or for smaller sampling volumes you can use the patient tube, with an alcohol wipe and leave to dry for 20 seconds. Clamp the tubing above where the fluid has collecte.
How to stretch in dressing?
Lift corner from the skin and slowly stretch the in dressing in a motion that is parallel to the skin
What is the role of a nurse in a chest tube?
As part of this process, the nurse is responsible for making respiratory and thoracic assessments, obtaining vital signs that reflect effectiveness of therapy or impending complications, and knowing the appropriate interventions ...
What to do if you have difficulty breathing?
Tell the patient to report any breathing difficulty immediately. Notify the doctor immediately if the patient develops cyanosis, decreased oxygen saturation, rapid or shallow breathing, subcutaneous emphysema, chest pain, or excessive bleeding.
What does it mean when your pleural space is bubbling?
This bubbling occurs normally when the system is removing air from the pleural cavity. If bubbling isn’t readily apparent during quiet breathing, have the patient take a deep breath or cough. Absence of bubbling indicates that the pleural space has sealed. 5. Check the water level in the suction-control chamber.
How to check water level in a suction control?
Check the water level in the suction-control chamber. Detach the chamber or bottle from the suction source; when bubbling ceases, observe the water level. If necessary, add sterile water to bring the level to the 20-cm line or to the ordered level.
How to tell if a rotary dry suction is working?
Check that the rotary dry suction control dial is turned to the ordered suction mark, usually −20 cm suction, and verify that the appropriate indicator is present, indicating the desired amount of suction is applied. In some models, an orange float appears in an indicator window. Other models indicate that the correct amount of suction is being delivered when the bellows reach the calibrated triangular mark in the suction monitor bellows window. Always refer to the manufacturer’s instructions.
Why do you splint your arm during a thoracotomy?
Usually, the thoracotomy patient will splint his arm to decrease his discomfort. 5. Assess the patient for pain and administer ordered pain medication, using safe medication administration practices, as needed for comfort and to help with deep breathing, coughing, and ROM exercises. 6.
What happens if you occlusion an air vent?
Periodically check that the air vent in the system is working properly (if applicable). Occlusion of the air vent results in a buildup of pressure in the system that could cause the patient to develop a tension pneumothorax.
What to do if a chest tube is disconnected from the drainage system?
If the tube is disconnected from the drainage system, immediately clamp it! Depending on hospital policy, the entire chest tube may need to be replaced or the ends of the tube and drainage system sterilized prior to reconnection. This is why I’m paranoid about properly securing tubes to the drainage systems with zip ties!
What to do if tube falls out of chest?
If the tube falls out entirely from the chest, immediately apply an occlusive dressing like Xeroform gauze at end expiration. If this is done after inspiration, air entrained in the pleural space through the chest wall defect may now become trapped (pneumothorax).
What is the system of a chest tube?
After a chest tube is placed, it’s connected to a drainage system like an Atrium (which I’ll be referencing in this post). This closed system consists of three chambers: collection, water-seal, and suction control.
What happens when you water seal a patient?
When we “ water seal ” a patient, suction is removed and drainage is monitored to gravity along with signs of air reaccumulation (repeat chest x-ray in a few hours, symptoms of dyspnea, etc.) Depending on the physician’s preference and clinical circumstances, this is often a good test prior to removing the chest tube.
What happens during spontaneous inspiratory breath?
Remember that during a normal, spontaneous inspiratory breath, the diaphragm contracts downward increasing intrathoracic volume while simultaneously creating a “ negative pressure” relative to the outside world. Airflow is directed into the lungs from the environment down a pressure gradient. What’s to say that air can’t be pulled back into the chest via a tube sitting in the pleural space? The water-seal!
What is the purpose of the chylothorax chamber?
This chamber collects and measures output which can be marked at regular time intervals. The characteristics of the output can also be visually assessed (ie, milky chylothorax after initiation of nutrition may suggest thoracic duct injury). Remember that a drop of blood in a bucket of water will tint the entire thing red, so not all “red drainage” is considered “sanguineous.” Always ensure an airtight seal between tubing interfaces with adapters, tape, and zip ties.
Where to clamp a chest tube?
As far as clamping the chest tube, if I see an air leak that just doesn’t make sense, sometimes I’ll briefly clamp the tube at the exit point of the chest. If the leak persists, the leak is somewhere in the system itself. Chest tubes are also briefly clamped as the drainage system is changed.
How to transport a patient with a chest tube?
Nurses should facilitate transport of a patient with a chest tube without clamping the tube and should ensure that the container remains upright and attached safely to the bedside while also monitoring the drainage container. 13 The nurse should ensure that the water-seal drainage container remains below the chest-tube insertion site while transporting the patient; otherwise, the contents of the container can backflow into the pleural cavity. 13 If clamping a chest tube for transport is unavoidable (eg, it is not possible to keep the drainage container below the level of the chest), then a nurse trained in chest-tube management should monitor the patient for signs of deterioration in oxygen saturation or respiratory rate or an increase in respiratory distress and should unclamp the tube when the patient reaches the destination.17
What is the procedure for insertion of a chest tube?
The first one is trocar based (ie, the Seldinger technique). The second is a blunt-dissection method by using a finger and an arterial forceps.
How many chest tubes are there?
Typically, a single chest tube is inserted. To drain blood, pus, or lymph from the pleural cavity, the chest tube is inserted at a slightly lower intercostal space (eg, sixth or seventh). To drain air from the pleural cavity, the chest tube may be inserted at a higher intercostal space (eg, second). Sometimes, however, two tubes are inserted: one at a lower intercostal space to drain blood or pus and another at a higher intercostal space to resolve a pneumothorax.
How long did a woman have difficulty breathing after a gastrectomy?
A 70-year-old woman was admitted to the hospital with breathing difficulty six weeks after undergoing a gastrectomy for stomach cancer. The physician ordered a chest x-ray, which showed a pleural effusion (ie, excess fluid in the pleural cavity) ( Figure 1 ). The physician inserted an intercostal drainage tube (ie, chest tube) to drain the pleural effusion and attached the tube to an underwater seal so that air could not enter the pleural cavity. On the following day, when the surgical team assessed the patient, the surgeon noted that the water-seal chamber was completely empty. A nurse had mistakenly emptied the entire chest-tube container to measure daily output, which is not an indication for emptying a chest-tube-drainage container. Furthermore, the nurse did not then refill the water-seal chamber. The surgeon immediately placed a clamp on the chest tube while the water seal was reinstituted. A chest x-ray was taken and indicated that a pneumothorax had not occurred. The surgeon completed a critical incident report. The nurse responsible for emptying the chest-tube container admitted to not knowing how to formally manage chest tubes.
What is the space around the lungs called?
The potential space around the lungs is called the pleural cavity . Under normal conditions, the pleural cavity is maintained by negative pressure, which is important for ensuring lung expansion with deep inspiration. When blood (ie, hemothorax), 4 air (ie, pneumothorax), 5 pus (ie, pyothorax), 6 or lymph (ie, chylothorax) 7 collects in the pleural cavity, negative pressure is lost and lung expansion is restricted. The chest-tube drain allows fluid or air to drain from the pleural cavity . As a result of the negative pressure, however, the air may preferentially enter the pleural cavity , particularly if the size of the chest-wall defect or the chest tube is larger than the size of the trachea.
Why do you need a water seal for pleural drainage?
Whenever the pleural cavity is drained by a chest tube, whether it is for blood, air, pus, or lymph, the tube should be connected to a water-seal drainage container so that air is not inadvertently sucked into the chest. The water-seal drainage container normally is filled with approximately 375 mL of sterile water to the marked level.
Why should chest tubes not be clamped?
In this situation, the chest tube should not be clamped because clamping the tube can cause a tension pneumothorax, which can be lethal.
Why do you need to enter the chest before a chest tube?
For patients in extremis, expeditious entry into the chest is necessary to relieve tension physiology and prevent cardiopulmonary collapse quickly. For a retained hemothorax, before chest tube placement, a handheld suction device can be inserted into the chest cavity to evacuate the hematoma.
How does a chest tube work?
The chest tube is connected to the first bottle, and all subsequent bottles are connected in a series to a suction device. The first bottle collects drainage from the chest; the second bottle acts as the water seal preventing air and fluid from moving back into the chest, and the third acts as suction control.
What is the treatment for tension pneumothorax?
Tension pneumothorax diagnosis based on clinical suspicion should be immediately treated by thoracostomy tube placement .[4] If unable to place a thoracostomy tube, a needle decompression or a finger thoracostomy will temporize the patient by venting the chest.
How much pleural fluid is needed for continuous respiration?
About 10 to 20 mL of pleural fluid provides lubrication for continuous respiration. A pneumothorax occurs when air is introduced into the pleural space. As more air is introduced, the air within the pleural space will act as a space-occupying lesion, preventing the lung's reinflation.
What is the pleural space?
The pleural space encompasses both a left and a right cavity that is separated by the mediastinum. Within each of the two cavities are the corresponding lungs (2 lobes on the left and 3 lobes on the right). Inspiration is accomplished by negative pressure created by the diaphragm.
How many Fr tubes are there in a chest tube?
Chest tube: Prospective studies of trauma patients have shown no difference when using small-bore chest tubes (20 to 22 Fr) compared to the traditional 28 to 32 Fr tubes from ATLS 10 recommendations when appropriately managed. [14]
What should trauma patients have?
For trauma patients, the general thought is that all patients should have: IV access, supplemental oxygen with monitoring, hemodynamic monitoring, and advanced airway capability at the bedside.
What is the purpose of a chest tube?
Managing a chest tube and drainage system. Intercostal drainage tubes (ie, chest tubes) are inserted to drain the pleural cavity of air, blood, pus, or lymph. The water-seal container connected to the chest tube allows one-way movement of air and liquid from the pleural cavity.
What is the purpose of intercostal drainage tubes?
Intercostal drainage tubes (ie, chest tubes) are inserted to drain the pleural cavity of air, blood, pus, or lymph. The water-seal container connected to the chest tube allows one-way movement of air and liquid from the pleural cavity.
Can a chest tube be clamped?
The container should not be changed unless it is full, and the chest tube should not be clamped unnecessarily. After a chest tube is inserted, a nurse trained in chest-tube management is responsible for managing the chest tube and drainage system.
