Full Answer
When is plateau pressure measured?
Plateau pressure is measured when inhalation is complete and right before a person begins to exhale, when there is no air flowing through the lungs. Both lung compliance and positive end-expiratory pressure (PEEP) impact plateau pressure. Lung compliance is a measure of the ability of the lungs to expand during inhalation.
How to understand plateau pressure?
In order to properly understand plateau pressure, a person must first be knowledgeable about the basic anatomy of the lungs, particularly the bronchioles and alveoli. The bronchioles are tiny tube-like branches in the lungs, and alveoli are tiny air sacs that are located at the end of the bronchioles. When a person inhales, oxygen travels ...
What is plateau pressure?
Plateau pressure is the pressure in the alveoli after a mechanically ventilated patient inhales. Mechanical ventilation refers to when a patient is hooked up to a machine that helps them breathe. Plateau pressure is also known as ''alveolar pressure'' and ''transpulmonary pressure''. Lesson. Quiz.
How long does a mechanical ventilator hold the time between inhalation and exhalation?
When measuring plateau pressure, the mechanical ventilator is often programmed to hold the time between inhalation and exhalation for 0.5-1.0 second.
What is the condition where fluid accumulates in the alveoli?
Acute respiratory distress syndrome (ARDS ): a condition when fluid accumulates in the alveoli, which can be caused by conditions such as sepsis, pneumonia, injuries to the chest, or COVID-19. Pulmonary fibrosis: a condition when the tissues of the lungs become scarred, thick, and stiff.
What are the mechanics of a ventilator?
Lung Mechanics. Although most modern ventilators are capable of providing a wide range of spirometric, airway pressure and flow, and static and dynamic compliance measurements, simple measures of lung mechanics should be chosen that are easily measured and reproducible.
What is plateau pressure?
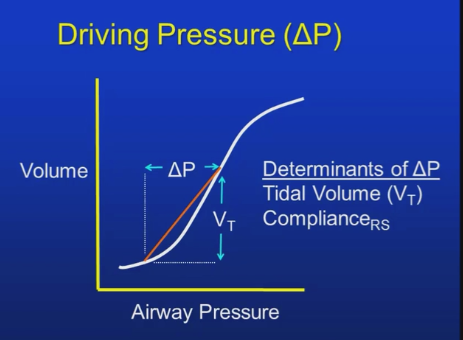
During mechanical ventilation, plateau pressure is often used as a surrogate for transpulmonary pressure (pressure used to distend the lung), when it is actually a measure of transrespiratory system pressure.
What is APRV in CPAP?
APRV is a form of lung-protective, open-lung ventilation. By setting the P High (upper CPAP level) in APRV, the airway pressure functions as a hybrid combining plateau pressure and PEEP level to maintain nearly complete recruitment pressure.
What is the best recruitment strategy for a ventilator?
The ideal recruitment strategy would be a sustained, noncyclic plateau pressure maintained at a level that minimizes atelectasis and limits tidal hyperinflation (i.e., continuous airway pressure set to the maintain lung aeration much like a recruitment maneuver). CO2 removal requires cyclic action (ventilation) to exhaust metabolic combustion. A ventilator strategy that achieves these basic concepts may provide a balanced approach of recruitment, limited overdistention, and adequate CO 2 removal. APRV is a form of lung-protective, open-lung ventilation. By setting the P High (upper CPAP level) in APRV, the airway pressure functions as a hybrid combining plateau pressure and PEEP level to maintain nearly complete recruitment pressure. APRV resembles a continuous recruitment maneuver that accommodates ventilation with a brief release of the CPAP phase. Thus, APRV uses the expiratory limb of the volume-pressure cure, and de-recruitment is minimized. 13,19,20 Because ventilation in APRV does not require additional airway pressure above the P High, plateau pressure levels are not exceeded to accommodate tidal volumes. This allows the P High to remain within the pressure limits considered safe (30 to 35 cm H 2 O). Because CO 2 removal (ventilation) is accomplished during the brief release phase or with spontaneous breathing throughout the P High (CPAP phase), de-recruitment and atelectasis formation are limited. Conventionally, the release time is less than 1 second.
How does APRV work?
Rather than producing a tidal volume by elevating airway pressure above the preset PEEP (as in traditional ventilation), tidal volumes during APRV are generated by releasing the airway pressure from P High to P Low (a lower CPAP level). During APRV, release ventilation lowers airway pressure and lung volume , reducing the risk for overdistention. APRV does not require an increase in airway pressure above P High to augment ventilation, allowing the process of ventilation to be directed away from lung inflation and distention. By contrast, conventional ventilation increases airway pressure, elevating lung volumes and potentially increasing the risk for overdistention.
What does APRV do?
During APRV, release ventilation lowers airway pressure and lung volume, reducing the risk for overdistention. APRV does not require an increase in airway pressure above P High to augment ventilation, allowing the process of ventilation to be directed away from lung inflation and distention.
What is the use of tidal volume in ALI/ARDS?
Increased elastic recoil is common to restrictive lung diseases such as ALI/ARDS, resulting in increased expiratory gas flow. With APRV, pressure is interrupted to release tidal volume and is driven by lung recoil stored during the P High period (T High) and gas compression. During traditional ventilation, inspiratory tidal volumes must overcome airway impedance and elastic forces of the restricted lung from its resting volume, increasing the energy or pressure required to distend the lung and chest wall. Furthermore, as compliance decreases, the inspiratory limb of the volume-pressure curve shifts to the right; that is, more pressure is required to deliver a set tidal volume. However, the expiratory limb remains unaffected by the prevailing volume-pressure relation and extends throughout all phases of injury.
When does plateau pressure apply?
Plateau pressure applies when there is not airflow in the circuit. That is when inspiration is complete. This pressure is determined by the lung compliance. So it follows that if there is a problem with the compliance the plateau pressure will rise.
What happens when you ventilate the lung?
If we ventilate the lung then the airway pressure will go up and the flow will increase (1) . When we release the breath, the pressure will go down, and the flow will move in the opposite direction as the air moves out (2). The flow then returns to base line (3).
Is peak pressure a reflection of lung compliance?
So, remember, peak pressure (circled) is a reflection of the airways and plateau pressure is a reflection of lung compliance.
How much pressure is required for mechanical ventilation?
Proper management of mechanical ventilation also requires an understanding of lung pressures and lung compliance. Normal lung compliance is around 100 ml/cmH20. This means that in a normal lung the administration of 500 ml of air via positive pressure ventilation will increase the alveolar pressure by 5 cm H2O. Conversely, the administration of positive pressure of 5 cm H2O will generate an increase in lung volume of 500 mL. When working with abnormal lungs, compliance may be much higher or much lower. Any disease that destroys lung parenchyma like emphysema will increase compliance, any disease that generates stiffer lungs (ARDS, pneumonia, pulmonary edema, pulmonary fibrosis) will decrease lung compliance.
How many breaths does a ventilator give?
In assist control, if the rate is set at 12 and the patient breathes at 18, the ventilator will assistwith the 18 breaths, but if the rate drops to 8, the ventilator will take over controlof the respiratory rate and deliver 12 breaths in a minute.
What is invasive mechanical ventilation?
Invasive mechanical ventilation is an intervention that is frequently used in acutely ill patients requiring either respiratory support or airway protection. The ventilator allows gas exchange to be maintained while other treatments are given to improve the clinical condition. This activity reviews the indications, contraindications, ...
How does mechanical ventilation affect the lungs?
Normal respiratory physiology works as a negative pressure system. When the diaphragm pushes down during inspiration , negative pressure in the pleural cavity is generated, this , in turn, creates negative pressure in the airways that suck air into the lungs.
Why do asthma patients get air traps?
In asthma, air trapping is caused by inflammation, bronchospasm, and mucus plugs, not airway collapse. The strategy to prevent auto-PEEP is similar to the strategy used in COPD.
What is the effect of ventilation?
Its most important effect is the removal of carbon dioxide (CO2) from the body, not on increasing blood oxygen content. Ventilation is measured as minute ventilation in the clinical setting, and it is calculated as respiratory rate (RR) times tidal volume (Vt). In a mechanically ventilated patient, the CO2 content of the blood can be modified by changing the tidal volume or the respiratory rate.
What is the positive pressure that will remain in the airways at the end of the respiratory cycle?
PEEP: The positive pressure that will remain in the airways at the end of the respiratory cycle (end of exhalation) is greater than the atmospheric pressure in mechanically ventilated patients. For a full description of the use of PEEP, please review the article titled “Positive End-Expiratory Pressure (PEEP).”