Common tests & procedures
To lower your risk of getting rhabdomyolysis, you should:
- Start an exercise program slowly, and listen to your body. If you feel especially sore or tired during a workout, stop and rest. ...
- Stay hydrated and avoid getting overheated. ...
- Don’t abuse alcohol or take illegal drugs.
- Talk to your doctor about any medications you’re taking that may increase your risk of developing rhabdomyolysis. ...
How to treat rhabdomyolysis naturally at home?
The prognosis of Rhabdomyolysis is heavily dependent upon the underlying etiology, and the associated comorbidities. Despite the lack of any well-organized prospective studies, the available evidence from case reports and small retrospective studies suggests that rhabdomyolysis, when treated early and aggressively, has an excellent prognosis.
What is the prognosis of rhabdomyolysis?
- dark-colored urine
- muscle weakness
- intense muscle pain
How do you diagnose rhabdomyolysis?
Many people recover after rhabdomyolysis treatment. But most people have lingering muscle weakness for a few weeks after the injury. In up to 50% of rhabdomyolysis cases, people experience acute kidney injury. Some people need dialysis for an extended time if their kidneys cannot function. Living With
Can You recover from rhabdomyolysis?
How do you know if you have rhabdo?
The only way to know you have rhabdo is through a blood test that checks for the presence of a muscle protein, creatine kinase (CK), in the blood. If you suspect that you may have rhabdo, ask to have your CK levels checked.
What does it feel like to have rhabdo?
If you develop rhabdo, you might have one or more of these symptoms: Muscle cramps, aches, or pains that are more severe than expected. Dark urine (tea- or cola-colored) Feeling weak or tired, unable to complete job tasks or finish a workout routine.
Why do firefighters need repeated CK tests?
Reminds providers to check firefighters’ repeated (serial) CK levels if they show possible rhabdo signs and symptoms. Repeated tests let healthcare providers know if levels are increasing or decreasing.
How to test for CK?
A healthcare provider can do a blood test for CK: 1 The muscle protein CK enters the bloodstream when muscle tissue is damaged. 2 When rhabdo is present, CK levels will rise.
What does it mean to have an earlier diagnosis?
Seek immediate medical treatment. Earlier diagnosis means an earlier start to treatment and a greater chance of recovery without permanent health effects.
Does CK rise right away?
Like symptoms, the rise in CK may not appear right away.
Can a dipstick test detect rhabdo?
Urine dipstick tests are not a good way to diagnose rhabdo: These tests check for myoglobin (a muscle cell component) indirectly. Myoglobin is quickly cleared from the body so it may not be detected in urine while CK elevations in the blood may persist for days.
What is the hallmark of acute rhabdomyolysis?
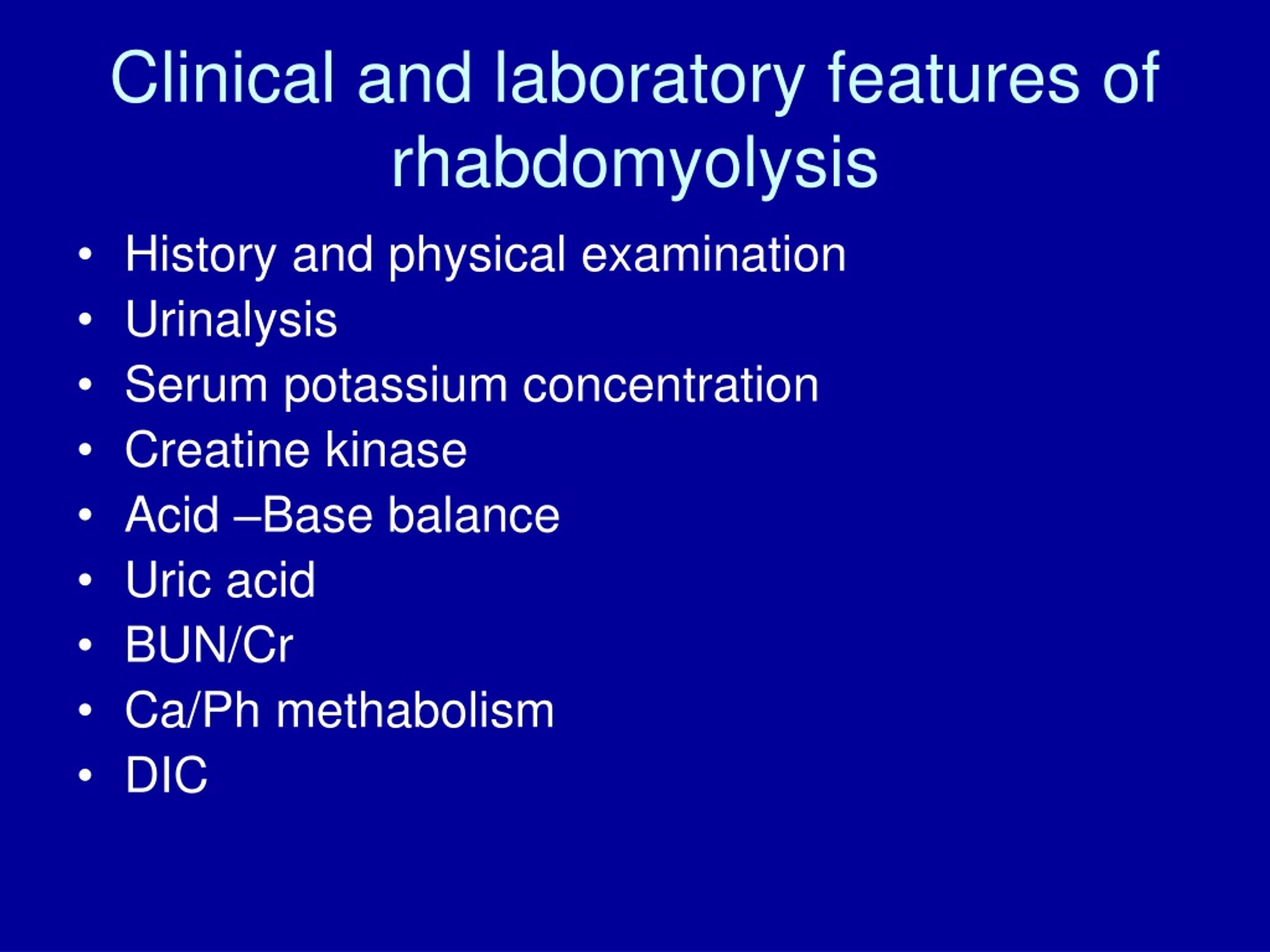
The hallmark of acute rhabdomyolysis is elevated CPK levels. In addition, reddish-brown urine from myoglobinuria may be present a 50% of cases. After triage and obtaining vital signs, basic labs including complete blood count, basic metabolic panel, liver function test, CRP, ESR, CPK levels, urinalysis, EKG, and chest X-ray should be obtained.
What is rhabdomyolysis in the body?
Rhabdomyolysis is a state of muscle injury that can lead to several forms of systemic insult, with the most important being acute kidney injury, electrolyte imbalance, and disseminated intravascular coagulation. The systemic complications associated with rhabdomyolysis result from the leakage of muscle intracellular components into the bloodstream. This activity reviews the causes, pathophysiology, and presentation of rhabdomyolysis and highlights the role of the interprofessional team in its management.
What is the color of myoglobin in urine?
With the release of an excess amount of myoglobin, heme-containing myoglobin is excreted in urine resulting in tea- colored urine. Its half-life is about 2 to 4 hours and is metabolized into bilirubin. Only 50% of patients with rhabdomyolysis may have reddish-brown color urine; myoglobinemia can be detected before the elevation of CPK. Because of the shorter half-life and rapid metabolism, myoglobinuria may not always be detected. Urine dipstick detects hemoglobin and myoglobin as blood; a follow-up microscopic evaluation for RBC should be done to rule out hemoglobinuria. The sensitivity of myoglobinuria in rhabdomyolysis is less than 25%. [40] Sometimes proteinuria may also be seen secondary to proteins released by damaged myocytes and changes in the glomerulus. Various biomarkers are being investigated for early diagnosis of heme-containing pigment-induced AKI. [41]
What is rhabdomyolysis in skeletal muscle?
Rhabdomyolysis means dissolution of skeletal muscle , and it is characterized by leakage of muscle cell contents, myoglobin, sarcoplasmic proteins (creatinine kinase, lactate dehydrogenase, aldolase, alanine, and aspartate aminotransferase), and electrolytes into the extracellular fluid and the circulation. The word rhabdomyolysis is derived from the Greek words rhabdos (rod-like/striated), mus (muscle), and Lucis (breakdown). [1] The common symptoms and signs are muscle weakness, pain/myalgia, local swelling and may be associated with dark red color urine/myoglobinuria. It can range from mild elevation in creatinine phosphokinase to medical emergencies like compartment syndrome, intravascular fluid depletion, Disseminated intravascular coagulation, pigment induced acute kidney injury (AKI), and cardiac arrhythmias. Laboratory diagnosis of rhabdomyolysis shows elevations in serum creatine phosphokinase (CPK), and there is no specific established serum level cut-off. Many physicians use three-five times the upper limit of normal Values of 100 to 400 IU/L (approximately 1000 IU/liter) for diagnosis. Rhabdomyolysis is one of the major causes of acute renal failure. [2] If identified early, the prognosis of acute kidney injury with rhabdomyolysis is relatively benign. [3] The etiology of rhabdomyolysis can be classified as traumatic and nontraumatic. Important causes of traumatic rhabdomyolysis are crush syndrome from accidents, earthquakes, and other natural and manufactured disasters. Not every muscle trauma leads to rhabdomyolysis and renal failure. Alternative causes for acute renal failure like dehydration, sepsis, drugs should always be evaluated. Seizures, alcohol use, drugs, prolonged bedridden state are common causes of nontraumatic rhabdomyolysis. [4]
What is the normal CPK level?
Normal CPK levels are 20 to 200 IU/L. Elevated levels usually at least five times the upper limit of normal is considered rhabdomyolysis. CPK exists in four significant isoenzymes, CK- MM, CK-MB, and CK-BB. The CK-MM is specific for skeletal muscle, CK-MB 1 and 2 specific for cardiac muscle, and CK BB for the brain. Its half-life is 36 hours. Serum CPK levels begin to rise within 2 to 12 hours after the injury peaks within 1 to 5 days. It declines after 3 to 5 days in the absence of muscle injury. The suspect continued muscle injury and compartment syndrome in cases of Persistently elevated CPK levels [39]
How long does it take to recover from rhabdomyolysis?
With better treatment, the mortality rates have decreased over the recent years, but the disorder still carries significant morbidity. Rapid intervention with aggressive hydration is the key to prevent renal injury and renal failure. Many patients take months to recover the muscle mass even after recovery, and some even have residual pain for a few years. [54] [55] [Level 5] With an interprofessional healthcare team approach to diagnosis and care that includes clinicians (MDs, DOs, PAs, NPs), specialists, nurses, and pharmacists, patients with rhabdomyolysis can achieve good outcomes and avoid the long-term sequelae of this condition. [Level 5]
What causes rhabdomyolysis?
The common causes of rhabdomyolysis are trauma, exertion, muscle hypoxia, infections, metabolic and electrolyte disorders, drugs, toxins, and genetic defects. [10] Recurrent episodes of rhabdomyolysis should prompt workup to identify underlying defects seen in muscle metabolism. The muscle damage can be from direct injury/trauma or by metabolic inequalities resulting in direct sarcolemmic injury or ATP depletion within the muscle fiber. Depletion of ATP impairs intracellular calcium regulation (usually, muscle cells maintain low levels of calcium at rest and increased calcium necessary for actin–myosin-binding during contraction), resulting in a persistent increase in sarcoplasmic calcium, causing persistent contraction, energy depletion, and activation of calcium-dependent proteases, phospholipases and eventual destruction of myofibrillar, cytoskeletal, and membrane proteins, followed by lysosomal digestion of fiber contents.
What is the best treatment for rhabdomyolysis?
If the rhabdomyolysis is severe enough to cause kidney damage, you may need dialysis. Dialysis extracts (removes) some of your blood, takes out toxins, and returns the filtered blood.
How long does it take for rhabdomyolysis to show symptoms?
Rhabdomyolysis symptoms can range from mild to severe. Symptoms usually develop one to three days after the muscle injury, though some people may not even notice muscle soreness. The main signs of rhabdomyolysis include: Muscle swelling. Weak, tender and sore muscles.
What is rhabdomyolysis?
Rhabdomyolysis. A rare condition, rhabdomyolysis is a muscle injury where the muscles break down. This is a life-threatening condition. Groups of people who have a higher risk of developing this condition include endurance athletes, firefighters, members of the military and older people. Urology 216.444.5600.
How to check myoglobin levels?
Order a urine test to check the levels of myoglobin in your urine. Take a sample of your blood to measure levels of creatnine kinase, a protein that muscles release when they disintegrate. After a diagnosis of rhabdomyolysis, doctors may order a muscle biopsy to find the cause. For a muscle biopsy, your doctor will:
Why does rhabdomyolysis happen?
Causes of rhabdomyolysis include: High-intensity exercise: Jumping into an exercise program too fast can lead to rhabdomyolysis when muscles don’t have time to heal after an intense workout. Severe dehydration and overheating: Heat causes faster muscle breakdown.
How long does it take to recover from rhabdomyolysis?
Many people recover after rhabdomyolysis treatment. But most people have lingering muscle weakness for a few weeks after the injury. In up to 50% of rhabdomyolysis cases, people experience acute kidney injury. Some people need dialysis for an extended time if their kidneys cannot function.
Why do people get rhabdomyolysis?
People can get rhabdomyolysis as a result of an inherited muscle disease (such as muscular dystrophy ). People who have certain metabolic or mitochondrial disorders also have a higher risk of rhabdomyolysis. A metabolic disorder affects the way energy moves into the cells.
