
When performing Biological Indicator Population Verification testing, BIs are macerated using a validated technique such as blending or by sterile glass beads. Then that macerate is heat shocked and the suspension is diluted to yield colonies in the range of 30–300 colony-forming units (CFU) and then plated. Other methods can be used as required.
What is a biological indicator test?
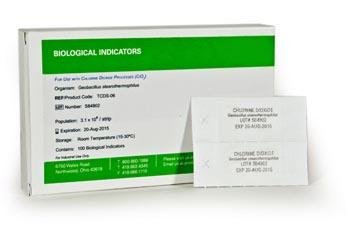
Biological Indicator Testing Procedure A biological indicator is made up of a carrier material, on which bacterial spores with a defined resistance to the sterilization process have been applied. The carrier material is enclosed within a glassine envelope or a vial.
What happens if growth is detected on a biological indicator test?
If growth is detected, the test is a fail. 1 Regardless of the type of process or application, Sterile Processing staff should always follow the manufacturer's instructions for use (IFUs) when using a biological indicator to monitor sterilization processes.
What factors should I consider when purchasing biological indicators?
Factors that may be considered when deciding which biological indicators to purchase include incubation time, brand name, cost, range and variety of products, validated applications and ease of use. Refer to ISO 11138-7:2019 for more information on supplier selection.
How do you determine the resistance of a biological indicator?
Most medical device manufacturers have defined acceptance criteria when it comes to the resistance of their biological indicators (BIs). The resistance of a BI can be determined by verification of the D-value or by verification of the survival/kill time response characteristics.
How do you determine the biological indicator of an autoclave?
stearothermophilus, a microorganism that is inactivated when exposed to 121.1oC saturated steam for a minimum of 20 minutes. Autoclaves used to treat biological waste will be evaluated with a biological indicator by EHS on a quarterly basis.
What is an biological indicator?
Biological indicator refer to organisms, species or community whose characteristics show the presence of specific environmental conditions. Other terms used are indicator organism, indicator plant and indicator species.
What is an example of a biological indicator?
One example of a bioindicator is lichens. These plants, which live on surfaces such as trees or rocks or soil, are very sensitive to toxins in the air. This is because they obtain their nutrients mostly from the air. We can tell our forests have clean air by the amount and types of lichens on the trees.
What are the two types of biological indicators?
STERIS biological indicators are available in two different species of spores, Bacillus atrophaeus for ethylene oxide (EO) and dry heat applications, and Geobacillus stearothermophilus for steam sterilization applications.
What is biological indicators in microbiology?
Biological Indicators: Biological indicators are test systems that contain viable microorganisms with a defined resistance to a specific sterilization process. They help monitor whether the necessary conditions were met to kill a specified number of microorganisms for a given sterilization process.
How many types of biological indicators are there?
There are at least three different types of biological indicators. Some biological indicators may also contain two different species and concentrations of spores.
How often should a biological indicator be put in the sterilizer?
How often should biological monitoring (spore testing) be done? A spore test should be used on each sterilizer at least weekly. Users should follow the manufacturer's directions for how to place the biological indicator in the sterilizer. A spore test should also be used for every load with an implantable device.
What is the difference between chemical indicator and biological indicator?
A biological indicator is used to ensure the chamber of your autoclave is getting completely saturated in the sterilization process. And the Chemical Indicators are used to be certain the steam is covering the entire load, and that the instruments are receiving the necessary amount of steam for proper sterilization.
How do you test an autoclave?
To check that the autoclave is functioning properly, the Vacuum Test, Bowie-Dick Test and Helix Test are carried out before the autoclave is used; Biological and chemical checks (sterilisation indicators) are performed during the sterilisation cycle to ascertain whether or not sterilization parameters are met.
What are the 3 types of sterilization?
Types of SterilizationSteam Sterilization.Dry Heat Sterilization.Ethylene Oxide (EtO) Sterilization.
What are the three types of sterilization monitoring?
The effectiveness and proper performance of a sterilizer must be confirmed through a combination of three types of monitoring: physical or mechanical, chemical and biological. Use of one type of indicator does NOT replace the need to use the other two types.
How are BIs aseptically placed?
In the Biological Indicator Sterility test, BIs are aseptically placed into soybean casein digest broth and incubated for the appropriate time and temperature , depending on the growth requirements for the indicator organism.
What is the number to call Nelson Labs for BIs?
If you have additional questions about Biological Indicators (BIs) Sterility test services, or would like to consult with the experts at Nelson Labs, just send us a request or call us at +1 (801) 290-7500.
What is a BI in sterilization?
Biological Indicators ( BIs) are widely used to monitor the efficacy of sterilization processes. BIs provide a high level of sterility assurance and are ideal monitors of the sterilization process. The BI Sterility test is performed on exposed BIs after completion of a sterilization load through either a validation or routine lot release monitoring.
How many days a week does Nelson Labs test?
Nelson Labs offers BI testing 7 days a week, 365 days a year with no holiday or weekend fees. Samples are tested immediately upon arrival and the final reports are uploaded to our secure website the same day BIs are released from incubation by 10:30AM (MST) from Monday to Friday.
What is a biological indicator?
A biological indicator (BI) is the only way to directly measure the lethality of a sterilization cycle. BIs are made using bacterial spores that are even harder to kill than any potential remaining microorganisms that may have survived the surgical equipment decontamination process.
Why are biological indicators used in sterilization?
Biological indicators are used to develop and validate sterilization processes, and therefore estimate SAL. The Importance of Proper Resistance. BIs contain a known number of live microorganisms (spores) to assess the adequacy of a sterilization cycle.
Why are self contained BIs activated?
After exposure to the sterilization process, self-contained BIs are activated to provide the spores with optimized growth media, and then must be incubated at the appropriate temperature to determine if any spores survived. For this reason, results are not immediately available.
What is sterility in biology?
Sterility is defined as being free from all living organisms.1 It is not practical to test every single device processed for the absence of microorganisms, so sterility is assumed according to the statistical probability that a given process killed every microorganism.
What is a biological indicator?
Biological indicators (BIs) provide information on whether necessary conditions were met to kill a specified number of microorganisms (bacterial spores) for a given sterilization process. STERIS’s full portfolio of biological indicators offer testing for a variety of applications including steam sterilization and vaporized hydrogen peroxide (VHP) sterilization. In these applications, Geobacillus stearothermophilus spores are primarily used due to their high resistance to these sterilization processes.
Why are geobacillus spores used?
In these applications, Geobacillus stearothermophilus spores are primarily used due to their high resistance to these sterilization processes. BIs are typically used within process challenge devices (PCD), designed to represent the most challenging products routinely processed for autoclave sterilization testing.
What is biological monitoring?
Biological monitoring is intended to verify that the sterilization conditions within the load were adequate to kill a known number of bacterial spores. As previously stated, biological monitoring is the only way to measure the lethality of a sterilization process.
Why is biological testing important?
Biological testing is an important part of the sterile processing technician’s roles and responsibilities. Due to the importance of BI testing, sterile processing personnel must make sure the test is performed correctly by checking the BI manufacturer’s instructions for use including, storing, performing and using the test correctly.
What should be documented in a log book?
Documentation. All biological testing should be accurately documented in a log book or other method, and include the following: • Date and time BI placed in autoreader/incubator. • The sterilizer number or other method of identification. • The cycle or load number.
How often should you test a sterilizer?
There are a number of times your sterilizer should be tested. These include: - Routine sterilizer efficacy testing which should be performed weekly, preferably each day the sterilizer is used. - All loads that contain implantable devices (devices that are implanted in the OR and remain in the patient for at least 30 days.
Where should the test pack be placed in the load?
Therefore, the placement and location of the test pack in the load is important. I always recommend that the test pack be placed on the autoclave cart (or inside the sterilizer for sterilizers without carts); FIRST, since the placement of the test pack is critical to the test results. Qualification Testing.
Can you do qualification testing in a non-tabletop sterilizer?
For qualification testing in non-tabletop sterilizers, the testing is performed in empty sterilizers. However for tabletop sterilizers, all biological testing, including qualification testing is always performed in a full load. Documentation.
