Now that you know where the popliteal artery is located, here’s how you can identify it:
- In a seated or lying position, slightly bend your leg at the knee, but not so bent that your foot is flat on the floor.
- Place your hands around the front of your knee so your fingers are on the back portion of your knee.
- Find the fleshy middle portion of the back middle of your knee.
How do you identify the popliteal artery?
Now that you know where the popliteal artery is located, here’s how you can identify it: In a seated or lying position, slightly bend your leg at the knee, but not so bent that your foot is flat on the floor. Place your hands around the front of your knee so your fingers are on the back portion of your knee.
What is a noninvasive test for popliteal artery disease?
This noninvasive test may be done before or after exercise or while you flex your foot up and down, which puts your calf muscle to work. Magnetic resonance angiography (MRA) shows the calf muscle that is trapping the artery. It can also reveal how much of the popliteal artery is narrowed.
What does a popliteal pulse test show?
Some of the conditions where a doctor may check the popliteal pulse include: Peripheral artery disease (PAD). PAD occurs when damage or narrowing of the arteries affects blood flow to the lower legs. Popliteal artery aneurysm.
What is MRA test for popliteal artery?
Magnetic resonance angiography (MRA) shows the calf muscle that is trapping the artery. It can also reveal how much of the popliteal artery is narrowed. You may be asked to flex your foot or press it against a board during this test. Doing so helps your doctor determine how blood is flowing to your lower leg.

How do you test for popliteal artery?
Wrap your hand around your knee so your fingers are against the soft spot in the back of your knee. Slowly press your fingers into this soft spot until you can feel your pulse. It should feel like a steady pulse once or twice per second. This is your popliteal pulse.
What happens if the popliteal artery is blocked?
Long-term pressure on the popliteal artery can cause the artery to narrow (stenosis), causing pain and cramping with just slight activity, such as walking. In severe cases or when undiagnosed, the nerves and muscles in the leg can become damaged. Blood clots may occur in the lower leg (deep vein thrombosis).
What is the preferred maneuver to diagnose popliteal entrapment syndrome?
A combination of the magnetic resonance imaging (MRI) with arteriography has been reported to be one of the most accurate diagnostic approaches for the PAES[6][7].
How do you expose the popliteal artery?
Below-knee popliteal artery exposure. The knee is flexed and rotated laterally. A roll is placed below the calf. A longitudinal incision is made 1-2 cm below the posterior edge of the tibia in the midleg and is extended proximally or distally as needed.
What are the symptoms of a blocked artery in your leg?
Symptoms include leg pain, numbness, cold legs or feet and muscle pain in the thighs, calves or feet....Exams and TestsA whooshing sound when the stethoscope is held over the artery (arterial bruits)Decreased blood pressure in the affected limb.Weak or absent pulses in the limb.
What does a popliteal blood clot feel like?
The symptoms of a popliteal vein thrombosis include pain, swelling, and tenderness around the area of the clot. While the vein is closer to the surface of the skin in the back of the knee, a clot can form anywhere in the blood vessel. The skin over the affected area may also feel warm to the touch.
How common is popliteal artery entrapment syndrome?
Popliteal artery entrapment syndrome (PAES) is a rare vein condition in the leg. It happens when tendons and muscles squeeze the knee's main (popliteal) artery, limiting blood flow to the lower leg. PAES tends to affect male athletes under 30, largely runners.
How do you know if you have popliteal aneurysm?
Symptoms of Popliteal Aneurysms Pain behind the knee. An edema (collection of watery fluid) in the lower leg. Foot pain. Ulcers on the skin of the feet that don't heal.
What is popliteal artery stenosis?
Popliteal artery stenosis or occlusive disease is a common occurrence in elderly patients, diabetics, smokers and those with cardiovascular disease. It leads to significant morbidity and mortality by reducing or completely blocking blood supply through the popliteal artery and into the lower leg.
How successful is leg bypass surgery?
Overall, bypass surgery is immediately successful in 90 to 95 percent of cases. The short and long-term success of the procedure is most closely linked to two factors: 1) the material employed for the bypass graft itself and 2) the quality of the arteries in the lower leg to which the graft is attached.
How long is the recovery time after popliteal bypass surgery?
Most patients will spend an average of two to five days in the hospital following popliteal bypass surgery. You'll need to take a few weeks off from work. Your surgeon will tell you when it is okay for you to try more strenuous activities. Full recovery will take six to eight weeks.
What are possible postoperative complications of a femoral popliteal bypass?
Some possible complications may include:Heart attack.Irregular heart beats.Bleeding.Wound infection.Swelling of the leg.Blood clot in the leg.Fluid in the lungs.Bleeding where the catheter is put in after the procedure.More items...
How is popliteal artery occlusion treated?
Surgery is the only way to correct the abnormal calf muscle and free the trapped artery. Your doctor will likely recommend surgery if your symptoms significantly affect your everyday or athletic activities.
What is the function of the popliteal artery?
The popliteal artery provides blood supply to the soleus, gastrocnemius, plantaris, and distal portions of the hamstring muscles.
How long is the recovery time after popliteal bypass surgery?
Most patients will spend an average of two to five days in the hospital following popliteal bypass surgery. You'll need to take a few weeks off from work. Your surgeon will tell you when it is okay for you to try more strenuous activities. Full recovery will take six to eight weeks.
Which artery is the most common to have blockage?
When this happens, patients may go into cardiac arrest. Statistically, Niess said widow-makers are more likely to lead to brain injury and irregular heartbeat. Although blockages can occur in other arteries leading to the heart, the LAD artery is where most blockages occur.
What to do if you think you have popliteal artery entrapment syndrome?
If you think you may have popliteal artery entrapment syndrome, it's important that you make an appointment with your doctor. If popliteal artery entrapment syndrome is found early, your treatment may be easier and more effective. Because appointments can be brief, and because there's often a lot to discuss, it's a good idea to be prepared ...
What is the first test to diagnose PAES?
Tests used to rule out other conditions and diagnose PAES include the following: Ankle-brachial index (ABI) measurement is usually the first test done to diagnose PAES. Blood pressure measurements are taken in your arms and legs during and after walking on a treadmill.
What is catheter based angiography?
Catheter-based angiography allows your doctor to see how blood is flowing to and from the lower leg in real time. It's done if the diagnosis is still unclear after other, less invasive imaging tests.
Is it normal to have a physical exam for PAEs?
The findings from a physical exam usually are normal.
Can you drink before a blood test?
Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as not drinking or eating anything for a few hours. You may need to do this if your doctor orders blood tests.
Can you have a popliteal artery bypass?
If you've had the condition for a long time, you may need artery bypass surgery. Bypass surgery is usually done only on those who have severe narrowing of the artery (stenosis) due to long-term popliteal artery entrapment syndrome.
How to tell where the popliteal artery is located?
Now that you know where the popliteal artery is located, here’s how you can identify it: In a seated or lying position, slightly bend your leg at the knee, but not so bent that your foot is flat on the floor. Place your hands around the front of your knee so your fingers are on the back portion of your knee.
Where to find popliteal pulse?
When to see a doctor. Takeaway. The popliteal pulse is one of the pulses you can detect in your body, specifically in the portion of your leg behind your knee. The pulse here is from blood flow to the popliteal artery, a vital blood supply to the lower leg. Several medical conditions can affect blood flow to and from the popliteal pulse.
Why would a doctor check your pulse here?
A doctor might check for a popliteal pulse to evaluate how well blood is flowing to the lower leg. Some of the conditions where a doctor may check the popliteal pulse include:
What is the name of the artery that supplies oxygen to the lower leg?
Then it becomes the femoral artery in the upper thigh. Finally, the popliteal artery is behind the kneecap. The popliteal artery is the major supplier of oxygen-rich blood to the lower leg.
Why is the popliteal artery important?
The popliteal artery is important to give blood flow to the lower legs and muscles surrounding the knee. If you have problems with blood flow to one or both legs, regularly checking your popliteal pulse may help you monitor your conditions.
What is the name of the condition that causes pulsatile mass in the lower leg?
Peripheral artery disease (PAD). PAD occurs when damage or narrowing of the arteries affects blood flow to the lower legs. Popliteal artery aneurysm. When you experience a weakness in the popliteal artery, it can cause a pulsatile mass you can often feel. Popliteal artery entrapment syndrome (PAES).
How to feel a pulse in your knee?
Others call it the “kneepit” for short. Press with increasing pressure until you feel a pulsation in the back of the knee. The pulsation will feel like a heartbeat, usually steady and even in nature. Sometimes you may have to press very deep into the popliteal fossa to feel the pulse.
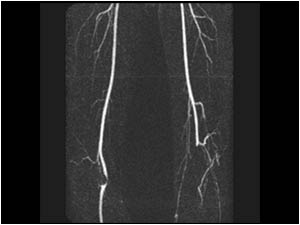
What is the best imaging for popliteal artery aneurysm?
Duplex ultrasonography (US) is the ideal screening and diagnostic imaging modality to detect a popliteal artery aneurysm and estimate its diameter. The US also provides detailed information regarding vessel patency, development of mural thrombus, and the status of outflow vessels. CT or magnetic resonance (MR) angiography are other alternatives to duplex ultrasonography and can accurately measure true lumen diameters as well as assist in the planning of operative repair. Conventional angiography is reserved for either elective endovascular repair of an aneurysm or in cases of threatening acute limb ischemia for initiation of thrombolytic therapy. [6][7][8]
What is the procedure to ligate the popliteal artery?
An alternative surgical approach is aneurysmectomy, followed by an interposition bypass with a prosthetic graft between the proximal and distal normal segments of the popliteal artery. However, the former method is more common.
What is the normal diameter of a popliteal artery?
The normal diameter of the popliteal artery varies from 0.7 to 1.1 cm. These focal dilations classify as fusiform (diffuse dilation) or saccular (asymmetrical). Popliteal artery aneurysms (PAAs) account for 85% of all peripheral aneurysms. Popliteal artery aneurysms are associated with abdominal aortic aneurysms 40% to 50% of the time.[1][2][3]
Why do popliteal aneurysms need to be repaired?
All symptomatic popliteal artery aneurysms require repair because of an increased incidence of thrombosis or limb loss. Asymptomatic aneurysms with a diameter greater than 2 cm are considered an indication for an elective operation to avoid complications such as limb-threatening ischemia. Greater than 45 angulation in asymptomatic aneurysms warrants surgical intervention because they can produce acute limb ischemia secondary to kinking of the vessel. [9][10][6]
What is a popliteal aneurysm?
A popliteal artery aneurysm is defined as a focal dilation in the artery, with the largest diameter being more than 50% of the normal. These focal dilations are classified as either fusiform or saccular. Popliteal artery aneurysms are associated with abdominal aortic aneurysms 40% to 50% of the time. They are usually asymptomatic, but may present with chronic symptoms due to mass effect. This activity describes the risk factors, diagnosis, and management of ruptured popliteal artery aneurysms and the role of the interprofessional team in caring for affected patients.
What is the most common cause of a popliteal fossa mass?
Both conditions usually present with chronic symptoms of claudication. However, the most common cause of a popliteal fossa mass is the Baker cyst , which is a benign swelling of the semimembranosus, or, more rarely, some other synovial bursa, found behind the knee joint. Orthopedic causes include prepatellar bursitis and meniscal cysts.
Where is the popliteal artery located?
It lies in the popliteal fossa accompanying its vein and terminates at the bifurcation into the anterior tibial artery and tibioperoneal trunk, which is located at the lower border of the popliteus muscle at the level of the tibial tuberosity.
What is the most common pathologic condition of the popliteal artery?
The popliteal artery can be affected by a variety of pathologic conditions, the most common of which is atherosclerosis. Affected patients are usually older, presenting with other risk factors for atherosclerosis, less acute symptoms, and disease at multiple levels. PAA and embolus also manifest in these patients, but symptoms will be more acute with occlusion of the popliteal artery. When aneurysm of the aorta or of the iliac, femoral, or popliteal artery is diagnosed in one location, appropriate imaging should be performed to find associated aneurysms. In younger patients and in those without generalized atherosclerosis , the differential diagnosis includes trauma, CAD, and PAES. A high degree of suspicion may be necessary to make these relatively rare diagnoses. Color duplex US with segmental arterial pressure readings or an ABI can help localize and determine the extent of popliteal artery disease. MR imaging and MR angiography are important imaging tools, especially in CAD and PAES. Angiography is usually performed prior to surgical treatment and in conjunction with interventional therapies such as angioplasty and thrombolytic therapy.
Where is the popliteal artery located?
The popliteal artery is located behind the knee in the popliteal fossa and is a direct extension of the superficial femoral artery after it passes through the adductor hiatus, an opening in the tendinous slip of the great adductor muscle of the thigh. The popliteal artery lies posterior to the femur and anterior to the popliteal vein. The popliteal artery and vein are normally located between the two heads of the gastrocnemius muscle (,,, Fig 1 ). Abnormalities in this relationship can produce popliteal artery entrapment syndrome (PAES). In the region of the knee, the popliteal artery gives off genicular and sural branches, eventually dividing into the anterior tibial artery and the tibioperoneal trunk. The tibioperoneal trunk further subdivides into the posterior tibial and peroneal arteries. The proximity of the popliteal artery to the distal femur makes it susceptible to injury when the distal femur is fractured or the knee is dislocated.
What is the most common type of aneurysm in the peripheral artery?
True aneurysms of the popliteal artery are the most common peripheral arterial aneurysms. Popliteal artery aneurysms (PAAs) are relatively uncommon compared with abdominal aortic aneurysms (AAAs), but recent studies have identified an increase in the prevalence of PAAs that may be due to greater access to imaging modalities such as US. Consequently, reports vary as to the ratio of PAAs to AAAs, which ranges from 1:8 to 1:23 (, 8,, 9 ). PAAs are associated with aneurysms in other locations. An AAA is present in 30%–50% of patients with a PAA. In contrast, PAAs are present in only about 10%–14% of patients with AAAs (, 9,, 10 ). PAAs are bilateral in 50%–70% of cases. These associations have important implications. In patients with a PAA, it is important to look for AAAs and a contralateral PAA. PAAs are usually found during the 6th and 7th decades of life and have a strong male predilection, with a male:female ratio ranging from 10:1 to 30:1 in published reports (, 10 –, 12 ).
What is the most common cause of popliteal artery occlusion?
Atherosclerosis is the leading cause of morbidity and mortality in the United States and is the most common cause of popliteal artery occlusion or stenosis. The pathogenesis of atherosclerosis is well established. Endothelial injury initiates a process whereby overproduction of cellular mediators eventually produces fibrotic plaque. This plaque may calcify, fracture, ulcerate, hemorrhage, and ultimately limit blood flow or cause thrombosis of the vessel. Risk factors for atherosclerosis include smoking, diabetes, advancing age, hyperlipidemia, hypertension, male gender, and a family history of the disease.
Which artery is affected by embolism?
Arterial Embolus. The popliteal artery, like any other peripheral artery, can be affected by embolism. Macroemboli have a tendency to lodge in the popliteal artery at the bifurcation into the tibioperoneal trunk and anterior tibial artery. An embolus in the lower extremities most often has a cardiac source.
What is noninvasive angiography?
Noninvasive arterial studies include color duplex ultrasonography (US) and an ABI with segmental lower-extremity arterial pressure readings or pulse volume recordings. These studies are cost effective and can help localize and determine the severity of lower-extremity arterial disease. MR angiography can provide noninvasive, arteriographic localization of disease, but at a greater cost. Gadolinium-enhanced three-dimensional time-of-flight MR angiography can provide diagnostic accuracy similar to that of standard contrast material–enhanced angiography. High-quality imaging requires a certain level of expertise and is best performed with a stepping table (, 2) or sequential imaging with multiple injections (, 3 ). There are still problems with variable runoff times and image degradation at the trifurcation due to venous filling. Conventional angiography is usually performed when endovascular or surgical intervention is required.
What is multilevel claudication?
Multilevel disease will manifest with more severe ischemic symptoms of rest pain and tissue loss. At physical examination, the patient will have a decreased or absent pulse at or below levels of significant disease. Bruits may be auscultated at levels of significant stenosis.
What does it feel like to have a missing popliteal pulse?
Talk to your doctor as soon as possible if you can’t find your pulse and you notice these other symptoms: Tingling or burning feeling in your legs. Numbness in your feet and legs. Cramping in one or both legs when you walk.
What does a weak popliteal pulse feel like?
Popliteal artery aneurysm. Your popliteal artery can develop weak spots like any other vein or artery in your body. A popliteal artery aneurysm will feel like a lump that pulses with your heartbeat.
What causes a popliteal pulse?
Your popliteal pulse is caused by your heartbeat. Your heart pumps blood through your body and your arteries pulse as your blood flows through them. The popliteal pulse is named after your popliteal artery. This is an important blood vessel that carries blood down through your leg to your feet.
Why do you have to press harder to find your pulse?
You may have to press harder to find it if you have health conditions that make your pulse weak or if you have a lot of muscle or fat tissue in your legs.
Where is the popliteal pulse located?
The location of the popliteal pulse is the soft spots behind your knees. Your popliteal pulse can help you monitor your health in several ways. Doctors might use it to help them diagnose and treat health problems and injuries.
How to feel your pulse?
Bend your leg a little, but not enough that your foot is flat on the floor. Wrap your hand around your knee so your fingers are against the soft spot in the back of your knee. Slowly press your fingers into this soft spot until you can feel your pulse.
Can you have a popliteal artery rupture?
Knee or leg injuries. You might have injured your popliteal artery if you’ve had an injury like a dislocated knee. Checking the pulse there can help your doctor learn whether you’ve suffered a popliteal artery rupture. This rupture can be very dangerous if it’s not treated quickly.
How to tell if popliteal artery is hard?
Feel the firmness of the artery. When taking the pulse, the popliteal artery may feel more firm than the area surrounding it, but it shouldn’t be hard. If the artery is hard or overly firm, let a doctor know immediately.
Where to find popliteal pulse?
If you cannot feel the popliteal pulse, look for a pulse in the blood vessels running down the center of the foot. Feel for a pulse as you would with any other vessel.
How to find pulse in a person?
To find this pulse, first, have the person lie flat and flex their knee at a 45-degree angle. Hold their leg with one hand and curl your fingers underneath their knee with your other hand. Use the tips of your index and middle fingers to gently compress the artery.
Why is it important to have a popliteal pulse?
It’s an important vital sign, though, since the popliteal pulse can help in assessing peripheral artery disease, or determining the severity and nature of a knee or femur injury. If you can’t feel the pulse, this doesn’t necessarily mean anything is wrong.
How many beats should a popliteal pulse be?
If you’ve found it, you should feel a soft, regular beat. Look at a watch or a clock as you count the beats. A healthy pulse should be below 99 beats a minute and have a regular rhythm. To learn how to check the popliteal pulse for complications, read more from our Medical co-author.
How to feel a pulse in the foot?
Feel for a pulse as you would with any other vessel. Run your index and middle finger from the person’s big toe up to the middle of their foot to feel their dorsalis pedis pulse. It may feel faint or be difficult to find, but you should be able to find it pretty easily after a little practice.
How long to count pulse rate?
You can either count for a full 60 seconds to get the pulse rate, or count for 30 seconds and double the number of beats for a solid estimate.
What is the popliteal artery?
What is popliteal artery entrapment syndrome? The popliteal artery is the dominant source of blood supply to the leg below the knee. Due to an abnormal course of the popliteal artery and the calf muscle group, the artery can be compressed and reduce blood flow. The consequence of reduced flow from calf contraction is immediate ...
What is the surgical procedure for popliteal artery entrapment syndrome?
In some types of PAES, a 4- to 6-inch incision behind the knee can provide the necessary exposure to relieve the popliteal artery. In other PAES types, a 4- to 6-inch incision along the inner side of the calf is required for complete relief.
Why does popliteal artery entrapment syndrome occur?
During fetal development, as limbs develop, the abnormal transit of the calf muscle around the vascular bundle is thought to be the primary event that leads to PAES. It is not uncommon for PAES to manifest later in the teens and 20s, when many young people engage in athletic activities and weight resistance training; the calf muscle growth incites the problem. Furthermore, the problem tends to be more prevalent in males. This may stem from rapid muscle mass gains, which are typical of male puberty.
Why do people need a metallic stent?
Metallic stents are commonly used to treat vascular disease that develops due to atherosclerosis (hardening of the arteries). In most cases, patients with PAES have a normal artery, and a stent placement is not durable or successful. Indeed, stent placement can significantly complicate recovery and should be avoided.
What questions will a clinician ask you about PAD?
Your clinician will also ask you questions about how active you are able to be and if you have slowed down for any reason. Your medical record will be reviewed to assess other risk factors you have for PAD.
How old do you have to be to get a PAD test?
Anyone with symptoms or signs of peripheral artery disease (PAD) should be tested. Some people should be screened for PAD even in the absence of symptoms or signs, such as individuals older than 65 years, or those older than 50 with risk factors like diabetes or smoking. The diagnosis of PAD begins with a simple examination by your doctor ...
Is the ABI test reliable?
Your physician will look at this waveform, your ABI number, and other information to make a determination of PAD. This test is very reliable. If your doctor needs more information, however, they may have you get a similar test which includes blood pressure readings and waveforms from your thigh down to your big toe.
Can you have an invasive catheter angiogram?
Finally, you may have an invasive catheter angiogram that can serve as both a test and a treatment. This procedure involves injecting dye into the affected arteries and taking X-ray images to see where blockages may be. If blockages are found, your clinician may open up these arteries during the procedure. They can use a device to cut, drill or shave through the plaque to allow more blood to flow through.
