
How do you manage STEMI?
STEMI Management 1 All patients must be triaged to a monitored resuscitation bay 2 IV access, and blood tests taken 3 Oxygen therapy avoid routine use of oxygen therapy among patients with SaO2 >; 93 % use when the SaO2 is below this level (or if the patient is shocked) (unless ... More items...
What is STEMI in cardiac emergency?
A STEMI is a true cardiac emergency, you must recognize a patient with a STEMI and arrange revascularization ASAP. Randomized trials have consistently shown better outcomes in terms or mortality and ischemic events with PCI.
When do you need a reperfusion for STEMI?
Indications All patients who present within 12 hours of symptom onset of STEMI should be considered for a reperfusion strategy, unless they have severe co-morbidities. Reperfusion is not routinely recommended in patients who present more than 12 hours after symptom onset.
What is the most important factor in a STEMI diagnosis?
The most important factor is how much damage there is to the heart muscle from the STEMI. That’s why it is so critical that you get medical attention quickly if you experience symptoms of a STEMI. Your healthcare provider is the best person to tell you what your outlook is, what to expect and what you can do to improve your situation.

How do you treat a patient with STEMI?
Aspirin. Early antithrombotic administration at the time of STEMI diagnosis consists of non-enteric-coated aspirin 162 mg to 325 mg (unless contraindicated) p.o., chewed immediately. Lifelong therapy using 81 mg to 325 mg daily should follow.
What is the first treatment for a STEMI?
Beta blockers – Patients with STEMI who do not have shock, HF, bradycardia, or heart block typically receive an oral beta blocker as part of the initial therapy for STEMI.
What is the protocol for a STEMI?
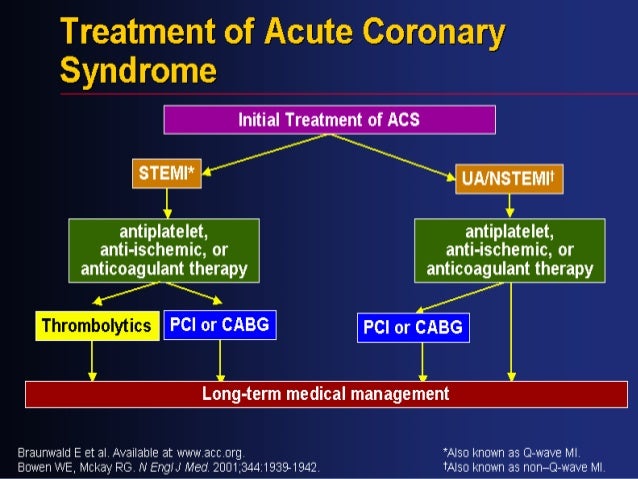
For patients who've had an ST-elevation myocardial infarction (STEMI), the standard of care is myocardial reperfusion using percutaneous coronary intervention (PCI) or thrombolytic agents. PCI is preferred, and time is of the essence.
What can you do with STEMI?
What are the treatment options for a STEMI?Option 1: Percutaneous coronary intervention (PCI) First, we look for where the blockage is located. ... Option 2: Thrombolysis. ... Option 3: Medications. ... Option 4: Coronary bypass surgery.
What is the best treatment for ST elevation MI STEMI?
Primary percutaneous coronary intervention (p-PCI) has become the treatment of choice for patients presenting with ST-segment elevation myocardial infarction (STEMI) when it can be performed expeditiously by an experienced team.
Which artery is blocked in a STEMI?
Anterior STEMI. This type of STEMI usually occurs when a blockage occurs in the left anterior descending (LAD) artery, the largest artery which provides blood flow to the anterior (front) side of your heart.
What is the goal of treatment for STEMI?
Background and objective: The goal of treatment of patients with ST-segment elevation acute myocardial infarction (STEMI) is to restore perfusion as soon as possible, preferably by primary percutaneous coronary intervention (PCI).
Can a STEMI resolve itself?
Patients presenting with ST-elevation myocardial infarction (STEMI), whose symptoms and electrocardiographic changes completely resolve upon admission and before the administration of reperfusion therapy, pose a therapeutic dilemma.
How long does it take to recover from a STEMI?
Most patients stay in the hospital for about a week or less. Upon returning home, you will need rest and relaxation. A return to all of your normal activities, including work, may take a few weeks to 2 or 3 months, depending on your condition. A full recovery is defined as a return to normal activities.
How long can you live after a STEMI?
Conclusions: Life expectancy of patients suffering a STEMI is nowadays intimately linked to survival in the first 30 days. After one year, the risk of death for both men and women seems similar to that of the general population.
Do you give fluids for a STEMI?
Abstract. Adequate hydration is recommended for acute ST-elevation myocardial infarction (STEMI) patients undergoing primary percutaneous coronary intervention (PCI) to prevent contrast-induced nephropathy (CIN).
What is the goal for PCI when treating a STEMI?
In the setting of acute ST-elevation myocardial infarction (STEMI), the primary goal of percutaneous coronary intervention (PCI) or fibrinolysis is to reestablish patency of the affected coronary artery and thereby improve perfusion of the myocardium.
What is in a STEMI kit?
The STEMI medication kit includes aspirin, clopidogrel, metoprolol, heparin, and nitroglycerin. An extra ECG machine was obtained for the ED and additional staff trained in its use. Guidelines were established for patients needing immediate ECG on arrival and for time intervals within the overall door-to-balloon time.
What is the best medication for pulmonary edema?
Morphine: Morphine is effective to relieve anginal chest pains and the sensation of dyspnea when pulmonary edema is present. There are also some beneficial hemodynamic effects including arterial vasodilation.
When to give an ACE inhibitor?
ACE inhibitors/Angiotensin receptor blockers: Either an ACE inhibitor or angiotensin receptor blocker should be given to all STEMI patients upon hospital discharge. Caution must be used in the acute setting in order to avoid hypotension which can worsen myocardial ischemia. Guidelines give the use of these drugs a class I indication when there is left ventricular systolic dysfunction or if the patient is diabetic. When left ventricular function returns to normal and the patient is not diabetic, the benefits are less clear. Usually ARBs are only given if ACE inhibitors are not tolerate due to cough or other side-effects.
Can beta blockers be given during STEMI?
Beta-blockers: While there is little data in regards to the efficacy of beta-blockers during UA/NSTEMI, there is an abundance during STEMI. Guidelines from the American Heart Association recommend early intravenous beta-blockers when no contraindication exists and there is angina, hypertension or tachycardia not related to heart failure. Otherwise, oral beta-blocker therapy is given in the acute setting. It is important NOT to give beta-blockers if there are signs of cardiogenic shock such as hypotension or pulmonary edema on chest x-ray. Long-term therapy (lifetime) has been shown to reduce MI incidence and improve mortality. Also, if left ventricular systolic dysfunction remains after a STEMI, beta-blockers are important for chronic systolic heart failure.
How to treat a STEMI patient?
Treatment of a STEMI patient can begin before the actual recognition of one occurs. Basic Life Support (BLS) providers can begin appropriate care by administering high flow O2, assessing vital signs and administering/assisting with oral aspirin and sublingual nitroglycerin depending on local protocols. When full ECG trained providers are available, rapid recognition should become the primary goal. While ACLS medications and interventions are important, ultimately the only cure to any STEMI is the eradication of the blockage and reperfusion of the damaged heart tissue. Pre-hospital providers should become familiarized with locations of cardiac catheterization laboratories. Studies have shown that in many scenarios, the total patient outcome/recovery is better when a patient is transported to cath labs and bypassing closer hospitals without them. As a result many rural hospitals and EMS services are designing new sets of protocols for the special treatment and transportation of STEMI patients.
What is the only cure for STEMI?
While ACLS medications and interventions are important, ultimately the only cure to any STEMI is the eradication of the blockage and reperfusion of the damaged heart tissue.
What does STEMI stand for?
The term STEMI is actually an acronym for (ST segment Elevated Myocardial Infarction). Ultimately in laymen's terms, this is a very grave heart attack that a victim's survivability is dependent upon quick and aggressive treatment from all care providers, beginning with First Responders and all the way to the cardiologist.
What is a STEMI?
So what exactly is a STEMI? The term STEMI is actually an acronym for (ST segment Elevated Myocardial Infarction). Ultimately in laymen's terms, this is a very grave heart attack that a victim's survivability is dependent upon quick and aggressive treatment from all care providers, beginning with First Responders and all the way to the cardiologist.
What is an inferior STEMI?
Another qualification for a STEMI is that there must be at least two leads of the same wall or contiguous (connected) walls that are elevated. So for instance should leads II and III be elevated this would be known as an Inferior STEMI. Or if leads V4 and V5 had elevation this would be known as an Antero-lateral STEMI. Note some the examples here.
How common is inferior STEMI?
Statistically, Inferior STEMI's are the most common. They making up between 40-50 percent of all STEMI's.
What is a STEMI?
OVERVIEW. STEMI is a type of acute coronary syndrome that requires emergency reperfusion therapy. Definition and assessment of STEMI is described in Acute Coronary Syndromes.
Which is preferred to nitrates for the initial control of pain in the setting of STEMI?
Opioid analgesia is preferred to nitrates for the initial control of pain in the setting of STEMI.
How many units of heparin should be given for STEMI?
Heparin (i.e. “unfractionated”) bolus dose of 5000 units should be given in cases of patients who are to receive PCI for their STEMI.
How long after symptom onset should you reperfusion?
Indications. All patients who present within 12 hours of symptom onset of STEMI should be considered for a reperfusion strategy, unless they have severe co-morbidities. Reperfusion is not routinely recommended in patients who present more than 12 hours after symptom onset.
What blood pressure should be infused before thrombolysis?
If the patient is hypertensive (>180/110), then a GTN infusion may be commenced to bring the blood pressure below this level, before giving thrombolysis.
Can a STEMI be given IV?
If required in the setting of a STEMI this should be given as an IV infusion, rather than topically or sublingually
When should aspirin be given for ACS?
In all patients with possible ACS and without genuine contraindications, aspirin dissolved or chewed) should be given as soon as possible after presentation
What is a STEMI?
A STEMI is a true cardiac emergency, you must recognize a patient with a STEMI and arrange revascularization ASAP.
How long does it take for thrombolysis to work?
NOTE: Generally thrombolysis is most effective at 1-2hrs after symptom onset, with gradually reducing efficacy to 6 hrs. After 6h, efficacy is lower (Guidelines still recommend thrombolysis if within 12hrs – see below).
Is ST elevation a STEMI?
Not all ST elevation is a STEMI!#N#ST segment on an ECG can be elevated for a number of reasons:#N#Any wide QRS (generally > 120ms) or a large-amplitude QRS (such as LVH) produces a repolarization abnormality, which results in the shifting of the ST segment in the opposite direction of the main QRS vector, which is known as “discordant ST change”. (See Figure: “Normal ST Changes in LBBB or Pacing” Below)#N#Wide QRS or large-amplitude QRS patterns that can cause discordant ST changes include: RBBB, LBBB, LVH, RVH, Pacing, Metabolic QRS widening, Pre-excitation, etc.#N#Significant transmural ischemia due to supply/demand mismatch can also produce ST elevation.#N#ALWAYS rule out:#N#Aortic Dissection (can present as Inferior STEMI – look for 1. Tearing Pain, 2. Maximal intensity at onset, 3. involving the back.#N#PE – Calculate the wells score#N#Pericarditis – Pleuritic? positional? pericardial rub? effusion?#N#Mechanical complication: (VSD, papillary muscle rupture) look for new murmur, or sudden flash pulmonary edema.
How effective is reperfusion for myocardial injury?
Although timely and complete reperfusion is the most effective way of limiting myocardial injury and subsequent ventricular remodeling, 10 most other effective therapeutic strategies for reducing infarct size or MVO have not been translated into improved clinical outcomes, despite tremendous research efforts in this field. 5, 11 There is currently only one study demonstrating improved clinical outcome (cardiac mortality, hospitalization for heart failure) with remote ischemic conditioning (RIC) in patients with STEMI. 12 Several explanations, including imperfect study design and true lack of efficacy, have been proposed to be responsible for the difficulties in translation. 13 For example, in the field of cardioprotection, preclinical data may be inadequate, and study design problems relate to patient selection or inappropriate timing and mode of delivery of the cardioprotective agent. 14 Moreover, previous cardioprotection studies were mainly aimed at protecting cardiomyocytes and reducing infarct size, neglecting other targets notably the coronary microcirculation. 10, 11, 15 On the contrary, infarct size and MVO represent 2 complementary therapeutic targets for cardioprotection trials. 16
What is the role of distal embolization in MVO?
Distal embolization is another important mechanism contributing to both myocardial injury and MVO. Coronary microembolization in experimental models causes regional contractile dysfunction. Of note, baseline myocardial perfusion starts falling when microspheres obstruct >50% of coronary capillaries. 26 Thus, the small number of emboli during primary PCI in the setting of STEMI, although not affecting baseline myocardial perfusion may create a local reacting milieu with release of inflammatory and vasoactive substances from coronary plaque, such as endothelin-1, tissue factor, and microparticles, which have the potential to increase the severity of the functional impairment of the coronary circulation. 27, 28 Moreover, in patients with STEMI, the coronary neutrophil extracellular traps burden correlates negatively with ST-segment resolution (STR) and positively with infarct size, thus suggesting that neutrophil extracellular traps may propagate thrombosis and inflammation distally into the infarcted myocardium and contribute to myocyte death during atheroembolism. 29 Finally, oxidative stress, ischemia per se, and soluble substances released from the ruptured plaque 27 reduce the bioavailability of nitric oxide, further contributing to the dysfunction of the myocardial microcirculation. 18 Distal embolization occurring during primary PCI probably represents only a part of the phenomenon, along with spontaneous distal embolization arising from ruptured or eroded plaques during the natural course of an acute coronary syndrome, and this may explain the negative results deriving from trials with distal filter protection devices. 31 However, the role of distal embolization during primary PCI is not so negligible, and a different approach may be probably useful to prevent MVO occurrence. Indeed, in the MASTER trial (Safety and Efficacy Study of MGuard Stent After a Heart Attack), patients with STEMI were randomized to conventional stent implantation or Mesh-covered embolic protection stent, and superior rates of epicardial coronary flow and complete STR were found in the Mesh-covered stent group. Of importance, this benefit was particularly evident among patients with a higher thrombus burden. 32
Does ischemic conditioning reduce infarct size?
Experimental studies over the past 3 decades demonstrated a cardioprotective role for ischemic conditioning. 10, 11, 100 In particular, RIC, using ≥1 cycles of brief limb ischemia and reperfusion, has been found in both small and large-animal MI models to reduce infarct size 101 but did not reduce the area of now-reflow in a pig model of reperfused MI. 102 Several clinical studies evaluated a possible protective role of ischemic conditioning on MVO. 103–107 In particular, in the CONDI trial (Remote Ischaemic Conditioning Before Hospital Admission, as a Complement to Angioplasty, and Effect on Myocardial Salvage in Patients With Acute Myocardial Infarction), remote ischemic perconditioning with 4 cycles of 5-minute arm ischemia/5-minute reperfusion during transport in the ambulance reduced infarct size but did not improve coronary blood flow. 103 A study by White et al demonstrated that remote ischemic perconditioning with 4 cycles of 5-minute arm ischemia/5-minute reperfusion at hospital admission reduced both infarct size and edema on CMR. 105 Also, remote ischemic postconditioning by 3 cycles of lower limb ischemia/reperfusion reduced edema and infarct size at CMR, improved STR during reperfusion, but did not improve TIMI frame count or myocardial blush grading. 104 Finally, in the LIPSIA CONDITIONING trial (Cardioprotection by Combined Intrahospital Remote Ischaemic Perconditioning and Postconditioning in ST-Elevation Myocardial Infarction), postconditioning alone with 4 cycles of 30-s reocclusion/reperfusion failed to improve myocardial salvage and MVO by CMR, but combined postconditioning with remote ischemic perconditioning by 3 cycles of 5-minute upper arm ischemia/5-minute reperfusion improved myocardial salvage, albeit reduced MVO only nonsignificantly 106 that translated in a reduced rate of MACE and new congestive heart failure after STEMI. 107 However, in the recent National Heart, Lung, and Blood Institute–sponsored trial, Traverse et al 8 found no reduction in infarct size in patients with STEMI with ischemic postconditioning but reduced MVO and improved LV functional recovery. Similarly, a study by Mewton et al 108 demonstrated that ischemic postconditioning reduced MVO in patients with STEMI treated with primary PCI. However, Verouhis et al 109 enrolling 93 anterior patients with STEMI and using a highly variable protocol of RIC did not demonstrate a reduced infarct size as a percentage of the area-at-risk (assessed by CMR at 4–7 days). The CONDI trial randomized 333 patients with STEMI to receive RIC or not in the ambulance during transportation to primary PCI. In the per protocol analysis of 251 patients, mean myocardial salvage index was higher in patients treated with RIC. In a secondary analysis involving longer-term follow-up to 4 years, compared with control treatment, RIC was associated with reductions in all-cause mortality and major adverse cardiac and cerebrovascular events 110 and a lowered economic deriving from reduced hospitalization for heart failure. 111 Some limitations of this trial include comparatively few primary outcome events (n=49). Of note, statin use was associated with increased efficacy of RIC to reduce infarct size. 112 However, these studies were underpowered for clinical outcome analyses, and the ongoing CONDI-2/ERICPPCI trial (Effect of Remote Ischaemic Conditioning on Clinical Outcomes in STEMI Patients Undergoing PPCI), which will investigate the effect of RIC on cardiac death and hospitalization for heart failure at 1-year in reperfused patients with STEMI, will shed further light on this topic.
Does ticagrelor reduce infarct size?
Recent experimental data have suggested that the platelet P2Y12 inhibitors may reduce infarct size when administered at the onset of reperfusion, conferring a postconditioning-like protection. 85, 86 However, a subanalysis of PLATO trial (The Study of Platelet Inhibition and Patient Outcomes) did not find differences with regard to myocardial perfusion between clopidogrel and ticagrelor, 87 and in the large ATLANTIC (Administration of Ticagrelor in the Cath Lab or in the Ambulance for New ST Elevation Myocardial Infarction to Open the Coronary Artery) study, prehospital administration of ticagrelor, in patients with acute STEMI, did not improve pre-PCI coronary reperfusion as assessed by STR. 88 The REDUCE-MVI trial (Reducing Micro Vascular Dysfunction in Acute Myocardial Infarction by Ticagrelor) did not find any differences in MVO or infarct size between ticagrelor and prasugrel. 89 Currently, the PITRI trial (Platelet Inhibition to Target Reperfusion Injury) is ongoing and is testing if intravenous cangrelor administered before reperfusion will reduce the incidence of MVO and limit infarct size in patients with STEMI treated with primary PCI. 90
Does ischemia cause inflammatory response?
However, a robust inflammatory response may lead to the occurrence of a significant interstitial myocard ial edema that not only is a consequence of sustained myocardial ischemia/reperfusion injury but also contributes to MVO by compressing capillaries and small arterioles and further decreasing flow through this dysfunctional microcirculation. 18 Moreover, the persistence of an inflammatory process in the chronic phase after MI may contribute to the occurrence of adverse ventricular remodeling and worse clinical outcomes. 127 Of note, statins represent one of the treatments able to attenuate inflammation in the context of MI, and probably the positive results of previously reported studies may be in part due to their anti-inflammatory effect. 75–78 However, specific therapies addressing inflammation have been disappointing overall and newer treatments are needed. 127 Probably, a tailored anti-inflammatory approach in patients with evidence of significant myocardial edema at CMR may select patients that effectively benefit from this treatment.
Does streptokinase help with reperfusion?
In a proof-of-concept randomized controlled trial, Sezer et al 113 reported that intracoronary administration of a reduced dose (250 kU) of streptokinase via the guiding catheter at the end of primary PCI improves myocardial reperfusion, instigating other clinical trials, such as T-TIME (A Trial of Low-Dose Adjunctive Alteplase During Primary PCI; http://www.clinicaltrials.gov. Unique identifier: NCT02257294), OPTIMAL (Optimal Coronary Flow After PCI for Myocardial Infarction; http://www.clinicaltrials.gov. Unique identifier: NCT02894138), RESTORE-MI (Restoring Microcirculatory Perfusion in ST-Elevation Myocardial Infarction; Australian New Zealand Clinical Trials Registry Number: 12618000778280), STRIVE (Adjunctive, Low-Dose tPA in Primary PCI for STEMI; http://www.clinicaltrials.gov. Unique identifier: NCT03335839), and a trial of intracoronary tenecteplase versus abciximab (EudraCT Number: 2010-022725-16). Two of these trials have recently reported. 114, 115 The T-TIME investigators tested the hypothesis that a strategy involving low dose intracoronary fibrinolytic therapy with alteplase (10 or 20 mg) infused during 5 to 10 minutes early after coronary reperfusion and before stenting would prevent and reduce MVO. One thousand five hundred twenty-seven patients had been screened, and 440 (28.8%) had been randomized (placebo, n=151; alteplase 10 mg, n=144; alteplase 20 mg, n=145) when the Data and Safety Monitoring Committee recommended that enrollment be discontinued due to futility. The amount (mean, SD) of MVO did not differ between the groups (2.32 [4.31] versus 2.61 [4.49] versus 3.48 [5.83] % LV mass; P =0.43). 114 Of interest, an increase in prothrombin F 1+2 concentrations was observed in the alteplase groups, despite achieving therapeutic anticoagulation with unfractionated heparin, and this undesired procoagulant effect of fibrinolytic therapy through thrombin activation may have led to microvascular thrombosis, limiting the efficacy of the intervention. 114 In the trial led by Morales-Ponce et al, 115 76 patients with anterior STEMI were randomized to treatment with either intracoronary tenecteplase or intravenous abciximab. At 4 months, infarct size measured by CMR was not different between the groups. In RESTORE-MI, enrollment involves a stratified approach with patient selection based on an increased IMR (>32) measured at the end of PCI. RESTORE-MI and STRIVE were designed as phase 3 trials and are still ongoing.
Why do we need to rule out STEMI?
Ruling out a STEMI is the main reason 12-lead ECGs are obtained, and it is critical that you learn to identify them – even as nurses .
What is a STEMI?
A STEMI is an ST-Segment Elevation Myocardial Infarction – the worst type of heart attack. This type of heart attack shows up on the 12-lead EKG. An NSTEMI (or Non-STEMI) does not have any ST elevation on the ECG, but may have ST/T wave changes in contiguous leads. Patients with STEMI usually present with acute chest pain and need to be sent to ...
How long does a STEMI last?
Hyperacute T waves are first seen, which are tall, peaked, and symmetric in at least 2 contiguous leads. These usually last only minutes to an hour max.
Which ST segment is more specific to cardiac ischemia?
Horizontal and Down-sloping ST-segment depression are more specific to cardiac ischemia, whereas up-sloping tends to be less serious although still could indicate ischemia.
What causes ischemia in the heart?
This is usually caused by unhealthy eating habits, obesity, sedentary lifestyle, hyperlipidemia, smoking, and genetics.
What are the outcomes of NSTEMI?
The outcomes of patients with NSTEMI depend on the severity of the myocardial injury, compliance with treatment and other comorbidities. Patients who do not change their risk factors for the coronary disease have a poor outcome. [15][16](Level V)
Why does NSTEMI occur?
Finally, conditions relatively unrelated to the coronary arteries or myocardium itself such as hypotension, hypertension, tachycardia, aortic stenosis, and pulmonary embolism lead to NSTEMI because the increased oxygen demand cannot be met. [4][5] History and Physical.
What causes ACS in STEMI?
While the cause of this mismatch in STEMI is nearly always coronary plaque rupture resulting in thrombosis formation occluding a coronary artery, there are several potential causes of this mismatch in NSTEMI. There may be a flow-limiting condition such as a stable plaque, vasospasm as in Prinzmetal angina, coronary embolism, or coronary arteritis. Non-coronary injury to the heart such as cardiac contusion, myocarditis, or presence of cardiotoxic substances can also produce NSTEMI. Finally, conditions relatively unrelated to the coronary arteries or myocardium itself such as hypotension, hypertension, tachycardia, aortic stenosis, and pulmonary embolism lead to NSTEMI because the increased oxygen demand cannot be met. [4][5]
When should beta blocker therapy be started for NSTEMI?
Beta-blocker therapy should be started within 24 hours after the presentation in patients who do not have a contraindication.
Is a physical exam for ACS or NSTEMI?
Physical Exam for ACS and NSTEMI is often nonspecific. Clues such as back pain with aortic dissection or pericardial friction rub with pericarditis may point to an alternative diagnosis for a patient’s chest pain, but no such exam finding exists that indicates ACS as the most likely diagnosis. Signs of heart failure should increase concern for ACS but are, again, nonspecific findings. [6][7][8]
The Importance of The St Segment
12 Lead Placement and Interpretation
- When assessing a potential cardiac patient it is important to obtain a 12 lead ECG as soon as possible. A traditional 12 lead ECG looks at four planes of the heart. The Inferior (the bottom), the Anterior (the front), the Lateral (outside wall closest to the patients left arm), and finally the Septal (inside wall closest to the sternum). Obtaining a 12 lead ECG can allow a technician to locate th…
Pre-Hospital Treatment of STEMI
- In conclusion, no matter the STEMI location, it is a serious life threatening emergency and rapid assessment and treatment can drastically impact the quality of life for the patient. Statistically, Inferior STEMI's are the most common. They making up between 40-50 percent of all STEMI's. Of those, about 80 percent of the blockages are located in the right coronary artery. The most letha…