
Tissue plasminogen activator produces clot lysis through the following sequence:
- tPA binds to fibrin on the surface of the clot
- Activates fibrin-bound plasminogen
- Plasmin is cleaved from the plasminogen associated with the fibrin
- Fibrin molecules are broken apart by the plasmin and the clot dissolves
What is the process of fibrinolysis?
Fibrinolysis is the process of breaking down the clot (the fibrin meshwork) into water-soluble fragments (fibrin degradation products or FDPs). Fibrinolysis (thrombolysis) is one of the steps of hemostasis (or to be precise, it occurs after hemostasis to dissolve the blood clot and restore the normal blood flow).
What is fibrin clot breakdown?
Fibrin clots are meant to be temporary structures formed to stop bleeding. After the process of wound healing has started, the ridged clot must be broken down to reduce the risk of thrombosis. The process of clot breakdown or fibrinolysis is orchestrated by the plasmin system.
What is the difference between fibrinolysis and anticoagulation?
Now, anticoagulation occurs during primary and secondary hemostasis and helps regulate clot formation, whereas clot retraction and fibrinolysis occur after primary and secondary hemostasis are complete, and help a clot contract and degrade.
What is the role of plasmin in the pathophysiology of fibrin clots?
Fibrin clots are lysed by plasmin, a serine protease that circulates in the blood as the inactive proenzyme, plasminogen. Free circulating plasmin is rapidly inhibited by α2 -antiplasmin.

What happens to a clot during fibrinolysis?
Fibrinolysis is the enzymatic breakdown of fibrin in blood clots. Plasmin cuts the fibrin mesh at various places, leading to the production of circulating fragments that are cleared by other proteases. Primary fibrinolysis is a normal body process.
What breaks down a fibrin clot?
Plasmin is the enzyme that breaks down fibrin. It is activated from inactive plasminogen by tissue plasminogen activator (t-PA) and urokinase.
What happens in clot retraction and fibrinolysis?
Clot retraction generally occurs within 24 hours of initial clot formation and decreases the size of the clot by 90%. Following clot retraction, a separate process called fibrinolysis occurs which degrades the fibrin of the clot while macrophages consume the expended platelets, thus preventing possible thromboembolism.
How is fibrin dissolved?
Fibrin clots are dissolved by the fibrinolytic system, acting in a series of enzymatic reactions with positive and negative feedback. In vivo, there is a careful balance between clotting, the conversion of fibrinogen to fibrin, and fibrinolysis, the proteolytic dissolution of the clot (Fig. 13.1).
What is clot dissolution?
Dissolution of Fibrin Clots (Fibrinolysis) tPA is released from endothelial cells by secretagogues generated following injury, including thrombin, and binds to fibrin. Active tPA cleaves plasminogen to plasmin which then digests the fibrin to soluble degradation products.
What is the mechanism of fibrinolysis?
Fibrinolysis is the process of proteolytic digestion of fibrin aimed at dissolving a clot or a thrombus to restore the blood flow. The central enzyme in fibrin lysis is plasmin, a serine protease formed from its inactive precursor, plasminogen, upon the action of activators, triggered by various pathologic stimuli.
What are the processes involved in clot retraction?
The 3 steps of this process for platelets are adhesion, aggregation, and finally, retraction. The clot retraction study measures the time taken for a platelet plug to undergo this last step, which indicates overall platelet function.
What is responsible for the contraction or retraction of the clot after it has formed?
Platelets play a key role in thrombin generation, clot formation, retraction, and lysis. Clot retraction is caused by normal or hyperactive platelet function and measured in vitro by measuring the volume of serum extruded from the clot or a decrease in size of the clot mass [67].
How does plasmin dissolve blood clots?
Plasmin cleaves fibrin. Plasmin is a serine protease that hydrolyzes the peptide bonds located on the carboxyl side of lysines and arginines in fibrin. Cleaving bonds in fibrin leads to the dissolution of the clot.
How does plasmin break down fibrin?
Plasmin breaks down cross-linked fibrin into soluble fibrin degradation products. Plasminogen is also converted to plasmin by both tPA and urokinase-type plasminogen activators. Plasmin cleaves tPA and urokinase to more active two-chain polypeptides that degrade the fibrin in the circulation.
Does bromelain dissolve fibrin?
In vitro and in vivo studies have suggested that bromelain is an effective fibrinolytic agent as it stimulates the conversion of plasminogen to plasmin, resulting in increased fibrinolysis by degrading fibrin [49, 50].
How do you reduce fibrin?
Increase your dietary intake of healthy fats (olive oil), omega-3s, and fiber. Some supplements may also help. If your fibrinogen levels are very high, your doctor may also prescribe fibrate or antiplatelet medication.
Does bromelain dissolve clots?
Bromelain is able to dissolve the clots because of its fibrinolytic properties.
What is plasmin function?
The main physiological function of plasmin is a blood clot fibrinolysis and restore normal blood flow.
What is the difference between fibrinolysis and thrombolysis?
Thrombolysis refers to the dissolution of the thrombus due to various agents while fibrinolysis refers specifically to the agents causing fibrin breakdown in the clot. Antifibrinolytics, such as aminocaproic acid (ε-aminocaproic acid) and tranexamic acid are used as inhibitors of fibrinolysis.
How to measure fibrinolysis?
The ELT measures fibrinolysis by clotting the euglobulin fraction (primarily the important fibrinolytic factors fibrinogen, PAI-1, tPA, alpha 2-antiplasmin, and plasminogen) from plasma and then observing the time required for clot dissolution. A shortened lysis time indicates a hyperfibrinolytic state and bleeding risk. Such results can be seen in peoples with liver disease, PAI-1 deficiency or alpha 2-antiplasmin deficiency. Similar results are also seen after administration of DDAVP or after severe stress.
What is the name of the drug that reduces plasmin activity?
Alpha 2-antiplasmin and alpha 2-macroglobulin inactivate plasmin. Plasmin activity is also reduced by thrombin-activatable fibrinolysis inhibitor (TAFI), which modifies fibrin to make it more resistant to the tPA-mediated plasminogen.
What is the product of coagulation?
In fibrinolysis, a fibrin clot, the product of coagulation, is broken down. Its main enzyme plasmin cuts the fibrin mesh at various places, leading to the production of circulating fragments that are cleared by other proteases or by the kidney and liver .
What is the role of fibrinolytic system?
The fibrinolytic system is closely linked to control of inflammation, and plays a role in disease states associated with inflammation. Plasmin, in addition to lysing fibrin clots, also cleaves the complement system component C3, and fibrin degradation products have some vascular permeability inducing effects.
What is the process of preventing blood clots from growing?
Fibrinolysis is a process that prevents blood clots from growing and becoming problematic. This process has two types: primary fibrinolysis and secondary fibrinolysis. The primary type is a normal body process, whereas secondary fibrinolysis is the breakdown of clots due to a medicine, a medical disorder, or some other cause.
Why do they give a thrombus blocker?
They are given following a heart attack to dissolve the thrombus blocking the coronary artery; experimentally after a stroke to allow blood flow back to the affected part of the brain; and in the event of a massive pulmonary embolism .
Which molecule binds to fibrin?
Third, thrombin proteolytically cleaves fibrinogen or factor I, into fibrin or factor Ia which binds with other fibrin proteins to form a fibrin mesh.
How does coagulation slow down?
By inhibiting both the intrinsic and common pathway, coagulation slows down dramatically.
What happens when there is a lot of thrombin around a damaged blood vessel?
When there’s a lot of thrombin around a damaged blood vessel, excess thrombin binds to thrombomodulin and it can no longer participate in the coagulation cascade.
What is the most important point of clot regulation?
Now, the most important point of clot regulation is when a coagulation factor called thrombin is produced .
What cofactor forms cross links between fibrin chains?
Factor XIIIa combines with a calcium ion cofactor to form cross links between the fibrin chains, further reinforcing the fibrin mesh.
What is the role of thrombin in the intrinsic pathway?
Activated platelets change their shape to form tentacle-like arms that allow them to stick to other platelets. Second, thrombin activates two cofactors ; factor V used in the common pathway, and factor VIII used in the intrinsic pathway.
Why is thrombin important?
Thrombin, or factor II, is a very important clotting factor, because it has multiple pro-coagulative functions. Think of thrombin as the accelerator on a car--the pedal that takes secondary hemostasis from 20 miles per hour to 100 miles per hour! First, thrombin binds to receptors on platelets causing them to activate.
What is the best way to break down a clot?
Unlike blood thinners, they do break down the clot. They work by turning on plasmin, which jump-starts your body’s natural process for clearing things out.
How does the body turn on a clot?
To turn it on, your body releases a substance known as an activator. It wakes up plasmin and tells it to get to work tearing things down. That mainly means breaking up the mesh-like structure that helps the clot work so well.
Why do you need blood thinners?
Blood thinners are also used to help prevent clots after a stroke or pulmonary embolism (when a blood clot travels to an artery in your lungs ). Blood thinners don’t dissolve the clot, but they can stop it from getting bigger and keep new ones from forming. That gives your body time to break up the clot.
How do blood thinners work?
Different blood thinners work in different ways: 1 Direct oral anticoagulants (DOACs) keep your body from making fibrin, the protein the forms the clot’s mesh. 2 Heparin keeps one of your body’s key clotting proteins, thrombin, from doing its job. 3 Warfarin ( Coumadin) slows down your liver ’s ability to make the proteins you need for clotting.
How long does it take for a pulmonary embolism to dissolve?
A DVT or pulmonary embolism can take weeks or months to totally dissolve. Even a surface clot, which is a very minor issue, can take weeks to go away. If you have a DVT or pulmonary embolism, you typically get more and more relief as the clot gets smaller.
What is the protein that is released when you heal a clot?
When your body senses that you’ve healed, it calls on a protein called plasmin. Here’s the clever part: Plasmin is actually built into the clot itself. It’s there the whole time, but it’s turned off. It just hangs out and waits. To turn it on, your body releases a substance known as an activator.
How does heparin work?
Heparin keeps one of your body’s key clotting proteins, thrombin, from doing its job .
How do fibrin clots work?
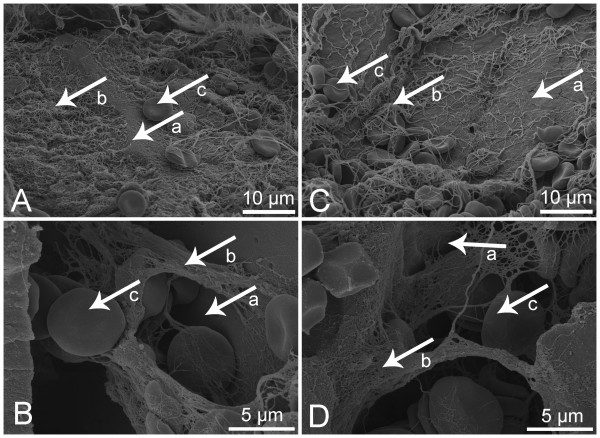
Fibrin clots are meant to be temporary structures formed to stop bleeding. After the process of wound healing has started, the ridged clot must be broken down to reduce the risk of thrombosis. The process of clot breakdown or fibrinolysis is orchestrated by the plasmin system. Physiologically, plasmin's precursor, plasminogen, circulates in the blood and binds to fibrin at specific binding sites, mainly lysine side chains [14,74,75]. Once bound to fibrin, this 92-kDa glycoprotein is converted to plasmin by one of two different activators: tissue plasminogen activator (tPA) or urokinase plasminogen activator (uPA). Plasminogen and tPA binding sites as well as initial plasmin cleavage sites are shown in Fig. 3.3 (left). tPA and uPA act in two different ways to produce plasmin. tPA, which is released by endothelial cells found on the lumen of blood vessels, can bind directly to fibrin [27]. As plasmin begins to degrade the clot, newly created lysine binding sites allow for further degradation of the clot [76]. If fibrin is absent, tPA is very weakly bound to plasminogen, resulting in a weak activation, but in the presence of fibrin, tPA can activate plasminogen in a highly accelerated manner [77]. This acceleration is a result of plasminogen and tPA binding sites on fibrin being close together. Conversely, uPA does not bind to fibrin under normal physiological conditions and therefore does not require fibrin to convert plasminogen into plasmin [78].
What is the function of fibrin clots in the fibrinolytic system?
Fibrinolytic System. Fibrin clots build up as an immediate response to tissue injury, but need to be removed during the following tissue remodeling phase. MCs are important cellular actors of the fibrinolytic process, which involves the activation of plasminogen into plasmin, a protease that dissolves fibrin clots.
What is the role of fibrinogen in coagulation?
Fibrin clot formation is a key event in the development of thrombotic disease and is the final step in a multifactor coagulation cascade . Fibrinogen is a large glycoprotein that forms the basis of a fibrin clot. Each fibrinogen molecule is comprised of two sets of Aα, Bβ, and γ polypeptide chains that form a protein containing two distal D regions connected to a central E region by a coiled-coil segment. Fibrin is produced upon cleavage of the fibrinopeptides by thrombin, which can then form double-stranded half staggered oligomers that lengthen into protofibrils. The protofibrils then aggregate and branch, yielding a three-dimensional clot network. Factor XIII, a transglutaminase, cross-links the fibrin stabilizing the clot protecting it from mechanical stress and proteolytic attack. The mechanical properties of the fibrin clot are essential for its function as it must prevent bleeding but still allow the penetration of cells. This viscoelastic property is generated at the level of each individual fiber up to the complete clot. Fibrinolysis is the mechanism of clot removal, and involves a cascade of interacting zymogens and enzymes that act in concert with clot formation to maintain blood flow. Clots vary significantly in structure between individuals due to both genetic and environmental factors and this has an effect on clot stability and susceptibility to lysis. There is increasing evidence that clot structure is a determinant for the development of disease and this review will discuss the determinants for clot structure and the association with thrombosis and vascular disease.
How do fibrin clots affect the tissue?
Fibrin clots are particularly affected by the presence of cells within the fiber network. The incorporation of platelets into the clot, which occurs relatively early during the wound-healing process, results in the formation of thinner fibers in areas of high platelet aggregation in comparison with the fibers present throughout the remainder of the clot [47 ]. Platelet α IIb β 3 interactions with fibrin cause the clot to become increasingly dense over time, resulting in the phenomenon known as clot retraction and conferring the network with resistance to tissue plasminogen activator-mediated fibrinolysis [ 10, 48 ]. During clot retraction, fibrinogen within the clot binds to α 5 β 1 integrin receptors on fibroblasts and endothelial cells on cell proliferation into the provisional matrix [ 5 ]. This overall densification of the network and binding of proliferating cells changes the cell shape and allows for complete healing of the wound site [ 5 ]. Platelets incorporated into a fibrin network also release platelet factor IV, which further decreases clot porosity and reduces the overall elastic modulus, and polyphosphate, which interacts with calcium to stabilize the clot and prolong lysis [ 48 ].
How is fibrin produced?
Fibrin is produced upon cleavage of the fibrinopeptides by thrombin, which can then form double-stranded half staggered oligomers that lengthen into protofibrils. The protofibrils then aggregate and branch, yielding a three-dimensional clot network.
What are the phases of fibrin thrombus formation?
The fibrin thrombus formation component of hemostasis occurs in three overlapping phases, initiation, amplification and propagation (Figure 13-2 ). The initiation phase begins with cell-based expression of tissue factor (TF) at the site of endothelial injury. Factor VII binds to the exposed TF and is rapidly activated. The factor VIIa/TF complex in turn generates factor Xa (FXa) and factor IXa (FIXa). FXa can activate factor V (FV) which complexes with FXa and generates small amounts of thrombin. During the amplification phase the pro-coagulant stimulus is transferred to the surface of platelets at the site of injury. The small amounts of thrombin enhance platelet adhesion, fully activate the platelets and activate factors V, VIII and XI. In the propagation phase the “tenase” complex of FIXa–FVIIIa is assembled on the platelet surface and efficiently generates FXa. Similarly the “prothrombinase” complex of FXa–FVa is assembled on the platelet surface and efficiently generates thrombin. Unlike FXa generated from TF–FVIIa interactions, FXa complexed to FV is protected from inactivation by tissue factor pathway inhibitor, assuring adequate thrombin generation. The resulting pro-coagulant, thrombin, activates factor XIII and cleaves fibrinopeptides (FPs) A and B from fibrinogen. The residual peptide chains aggregate by means of loose hydrogen bonds to form fibrin monomers. Under the influence of FXIIIa, fibrin monomers are converted into fibrin polymers, forming a stable fibrin clot. In the presence of thrombin, the mass of loosely aggregated intact platelets is transformed into a densely packed mass that is bound together by strands of fibrin to form a definitive hemostatic barrier against the loss of blood.
Why is clot lysis so fast?
Due to the fragile balance of lysis inhibitors, the speed of clot lysis is a complex combination of many different factors. Various factors in the blood are counteracting the conversion of plasminogen to plasmin while also competing with plasminogen to bind to fibrin.
Overview
Pharmacology
In a process called thrombolysis (the breakdown of a thrombus), fibrinolytic drugs are used. They are given following a heart attack to dissolve the thrombus blocking the coronary artery; experimentally after a stroke to allow blood flow back to the affected part of the brain; and in the event of pulmonary embolism.
Thrombolysis refers to the dissolution of the thrombus due to various agents while fibrinolysis r…
Physiology
Plasmin is produced in an inactive form, plasminogen, in the liver. Although plasminogen cannot cleave fibrin, it still has an affinity for it, and is incorporated into the clot when it is formed.
Tissue plasminogen activator (t-PA) and urokinase are the agents that convert plasminogen to the active plasmin, thus allowing fibrinolysis to occur. t-PA is r…
Measurement
Plasmin breaks down fibrin into soluble parts called fibrin degradation products (FDPs). FDPs compete with thrombin, and thus slow down clot formation by preventing the conversion of fibrinogen to fibrin. This effect can be seen in the thrombin clotting time (TCT) test, which is prolonged in a person that has active fibrinolysis.
FDPs, and a specific FDP, the D-dimer, can be measured using antibody-antigen technology. Thi…
Role in disease
Few congenital disorders of the fibrinolytic system have been documented. Nevertheless, excess levels of PAI and α2-antiplasmin have been implicated in metabolic syndrome and various other disease states.
However, acquired disturbance of fibrinolysis (hyperfibrinolysis), is not uncommon. Many trauma patients have an overwhelming activation of tissue factor and thus massive hyperfibrinolysis. H…
Fibrinolytic enzymes
• Anistreplase
• Desmoteplase
• Streptokinase
• Nattokinase
• Lumbrokinase
External links
• Graphical representation of the fibrinolytic pathway (site not available)