
Atrial natriuretic peptide (ANP
Atrial natriuretic peptide
Atrial natriuretic peptide or atrial natriuretic factor is a natriuretic peptide hormone secreted from the cardiac atria. Natriuretic peptides are a family of hormone/paracrine factors that are structurally related. The main function of ANP is causing a reduction in expanded extracellular fluid volume …
What is the function of atrial natriuretic peptide?
Atrial natriuretic peptide. Atrial natriuretic peptide ( ANP) or atrial natriuretic factor (ANF) is a natriuretic peptide hormone secreted from the cardiac atria. Natriuretic peptides (ANP, BNP, and CNP) are a family of hormone/paracrine factors that are structurally related. The main function of ANP is causing a reduction in expanded...
What is atrial natriuretic factor?
Atrial natriuretic factor (ANF), brain natriuretic peptide (BNP), and C-type natriuretic peptide (CNP) are a family of polypeptides that play an important role in maintaining cardiovascular homeostasis. ANF and BNP are produced and secreted by the atria of the heart and have diuretic and natriuretic activity.
How is ANP secreted from the heart?
ANP is secreted in response to: Increased sodium concentration ( hypernatremia ), though sodium concentration is not the direct stimulus for increased ANP secretion Three types of atrial natriuretic peptide receptors have been identified on which natriuretic peptides act.
Where does natriuretic peptide act in the kidney?
Natriuretic Peptides. Atrial natriuretic peptide (ANP) and B-type natriuretic peptide act at many sites in the kidney and elsewhere to decrease left atrial pressure and blood pressure and increase renal salt excretion. As shown in Figure 33-1, a major site of ANP action in the kidney is along the medullary collecting tubule.
What is the action of atrial natriuretic hormone?
The atrial natriuretic hormone (ANP) is a cardiac hormone which gene and receptors are widely present in the body. Its main function is to lower blood pressure and to control electrolyte homeostasis.
What triggers the release of ANP?
Volume loading, vasoconstrictor agents, immersion in water, atrial tachycardia and high salt diets have been reported to increase the release of cardiac ANP, thereby suggesting that the peptide is released in response to an increase in atrial pressure.
How does atrial natriuretic affect blood pressure?
Atrial natriuretic factor (ANF) antagonizes vasoconstriction induced by numerous smooth muscle agonists and also lowers blood pressure in intact animals. ANF has particularly marked relaxant effects on angiotensin II-contracted vessels in vitro.
How does ANP control blood pressure?
When blood sodium levels and pressure are increased, ANP is secreted from the heart. It binds to its receptor in the kidney and blood vessels, and promotes salt excretion, lowers blood volume and relaxes the vessel.
Does ANP increase or decrease blood pressure?
Atrial natriuretic peptide (ANP) decreases arterial blood pressure and lowers mean circulatory filling pressure by decreasing venous compliance.
What happens when ANP is released?
ANP stimulates vasodilation of the afferent arteriole of glomerulus: this results in increased renal blood flow and an increase in glomerular filtration rate. Increased glomerular filtration, coupled with inhibition of reabsorption, results in increases in excretion of water and urine volume - diuresis!
How does atrial natriuretic hormone affect the kidneys?
effect on kidney function This hormone, called atrial natriuretic peptide (ANP), exerts a vasodilator effect on the kidney and also reduces tubular reabsorption of sodium. Both actions result in increased urinary elimination of salt and water and tend to restore atrial pressure toward the normal.
What is the activity of atrial natriuretic peptide?
Atrial natriuretic peptide (ANP) is a cardiac hormone that regulates salt-water balance and blood pressure by promoting renal sodium and water excretion and stimulating vasodilation. ANP also has an anti-hypertrophic function in the heart, which is independent of its systemic blood pressure-lowering effect.
How does ANP cause vasodilation?
We found that ANP causes a vasodilatation of the blood vessels which supply the glomeruli and a vasoconstriction of the arterioles which drain them. This substantiates the finding that increased filtration pressure participates in the natriuretic response.
Does ANP increase heart rate?
In both positions ANP had dose dependent effects of increasing heart rate (HR) and maximal acceleration whilst lowering an index of systemic vascular resistance (ISVR). In the erect position ANP also lowered systolic blood pressure.
How does ANP decrease sodium reabsorption?
In the medullary collecting duct, ANP reduces sodium reabsorption by inhibiting the cyclic nucleotide-gated cation channels, the epithelial sodium channel, and the heteromeric channel transient receptor potential-vanilloid 4 and -polycystin 2 and diminishes vasopressin-induced water reabsorption.
What is the function of atrial natriuretic peptide quizlet?
Atrial natriuretic peptide is a hormone that controls blood pressure in part by increasing the urinary excretion of sodium. The parathyroid glands maintain adequate levels of blood calcium.
What stimulates atrial natriuretic peptide release quizlet?
what stimulates secretion of atrial natriuretic peptide ANP? an adnormal increase in blood volume which causes the distention of the atria.
What regulates atrial natriuretic peptide?
Atrial NP (ANP) is secreted exclusively by atrial myocytes, whereas brain NP (BNP) is secreted predominantly by ventricular myocytes, albeit at a low rate. In response to acute and chronic stress, ventricular myocytes up-regulate the synthesis and secretion of ANP and BNP.
What stimulus causes the release of atrial natriuretic hormone from the atria of the heart quizlet?
Atrial natriuretic peptide (ANP) is released by cells in the wall of the right atrium of the heart in response to increased pressure caused by high blood volume.
Where does ANP act on kidney?
In the kidney, ANP binds to the natriuretic peptide receptor-A (NPR-A) and enhances its guanylyl cyclase activity, thereby increasing intracellular cyclic guanosine monophosphate production to promote natriuretic and renoprotective responses.
What does the ANP hormone do?
ANP hormone helps regulate electrolyte homeostasis within the body fluids. It even helps reduce the heart overload in pathological states including...
What is the function of ANP?
The main function of ANP is to enhance the excretion of sodium and water from the body through urine. Thus, this hormone of cardiac origin acts on...
How does atrial natriuretic peptide regulate blood pressure?
ANP, or atrial natriuretic peptide, regulates blood pressure by decreasing blood volume. This is mainly achieved by increasing the glomerular filtr...
What stimulates ANP?
ANP stimulates the excretion of sodium and water by inhibiting their reabsorption in the kidneys. It also stimulates vasodilation of afferent arter...
What happens when a natriuretic peptide is bound to a receptor?
Binding of a natriuretic peptide induces a conformational change in the receptor that causes receptor dimerization and activation. The binding of ANP to its receptor causes the conversion of GTP to cGMP and raises intracellular cGMP.
When was the natriuretic factor first discovered?
The discovery of a natriuretic factor (one that promotes kidney excretion of salt and water) was first reported by de Bold in 1981 when rat atrial extracts were found to contain a substance that increased salt and urine output in the kidney.
What is NEP inhibitor?
Several inhibitors of NEP are currently being developed to treat disorders ranging from hypertension to heart failure. Most of them are dual inhibitors (NEP and ACE ). In 2014, PARADIGM-HF study was published in NEJM. This study considered as a landmark study in treatment of heart failure. The study was double blinded; compared LCZ696 versus enalapril in patients with heart failure. The study showed lower all cause mortality, cardiovascular mortality and hospitalization in LCZ696 arm. Omapatrilat (dual inhibitor of NEP and angiotensin-converting enzyme) developed by BMS did not receive FDA approval due to angioedema safety concerns. Other dual inhibitors of NEP with ACE/angiotensin receptor are (in 2003) being developed by pharmaceutical companies.
What are ANP precursors used for?
ANP and related peptides are used as biomarkers for cardiovascular diseases such as stroke, coronary artery disease, myocardial infarction and heart failure.
What are the three types of natriuretic peptide receptors?
They are all cell surface receptors and designated: guanylyl cyclase-A (GC-A) also known as natriuretic peptide receptor-A (NPRA/ANP A) or NPR1.
What is the BNP in the heart?
These effects may be blunted or negated by various counter-regulatory mechanisms operating concurrently on each of these secondary effects. Brain natriuretic peptide (BNP) – a misnomer; it is secreted by cardiac muscle cells in the heart ventricles – is similar to ANP in its effect.
What is ANF in medical terms?
Pang from Queen's University. Atrial natriuretic peptide ( ANP) or atrial natriuretic factor (ANF) is a natriuretic peptide hormone secreted from the cardiac at ria that in humans is encoded by the NPPA gene. Natriuretic peptides (ANP, BNP, and CNP) are a family of hormone/paracrine factors that are structurally related.
What is ANP in kidneys?
Atrial natriuretic peptide (ANP) is a hormone that is synthesized by atrial myocytes and is released in response to increased atrial distention. From: National Kidney Foundation Primer on Kidney Diseases (Sixth Edition), 2014. Download as PDF. About this page.
Where is ANP expressed?
In the adult heart, ANP gene is expressed predominantly in the atria where ANP mRNA represents 1–3% of total mRNA.
What is ANF in plasma?
Atrial natriuretic factor (ANF) or atrial natriuretic peptide (ANP) consists of mixtures of peptides of various lengths. Studies have shown that the circulating form of ANF in plasma consists of a 28-amino acid residue ANF (ANP), whereas the rat and human atrium largely stores pro-ANF (γ-ANP), containing 126 amino acid residues, ...
What is ANP in fish?
Atrial natriuretic peptide (ANP) is the first hormone isolated from the heart as a potent natriuretic/diuretic and hypotensive factor. ANP has an intra-molecular ring structure connected by two cysteine residues and N-terminal and C-terminal extensions from it. ANP is present in mammals, amphibians and bony fishes, but absent in birds, reptiles, cartilaginous fishes, and cyclostomes. ANP induces profound natriuresis/diuresis, hypotension, and inhibition of aldosterone secretion in mammals and amphibians. In teleost fish, ANP is a hypotensive hormone but its osmoregulatory effect is more versatile. In eels, ANP potently inhibits drinking and intestinal NaCl absorption, exerts a weak antidiuretic effect and stimulates cortisol secretion, all of which promote seawater adaptation. In human, ANP is an important target for diagnosis and treatment of heart failure. ANP knockout results in salt-sensitive hypertension.
Where is the ANP gene stored?
ANP is synthesized as a prepropeptide from mRNA originating from three exons of ANP gene. Prepropeptide and its derivative ANP propeptide are stored in the cells. Proteolytic cleavage of the propeptide sequences results in the formation of mature (low molecular mass) ANP 99–126 and N-terminal N-proANP 1–98.
Where is ANF found?
Additionally, ANF has been found in the brain, and centrally medicated effects on fluid volume regulation may be important. Elevated plasma ANF has been noted in humans with a variety of diseases ranging from congestive heart failure to obstructive lung disease to chronic renal failure.
Which receptor binds to the truncated ANF derivative?
The R 2 receptor specifically binds the truncated ANF derivative, ANF–NH 2 (cANF), whereas this analog does not activate the R 1 receptor. Therefore, cANF has been utilized in numerous studies to identify specific ANF binding to the R 1 receptor and to displace binding from the R 2 receptor.
What is the function of the natriuretic peptide?
Atrial natriuretic peptide: an essential physiological regulator of transvascular fluid, protein transport, and plasma volume
How does ANP affect the vascular system?
In addition to these renal effects, ANP causes both vasodilation, by relaxing vascular smooth muscle, and an acute increase in vascular permeability via receptors on the microvascular endothelium (4, 5). These mechanisms also decrease blood volume by favoring redistribution of plasma protein and fluid from the vascular space to the interstitial space. Thus, a key question concerning the role of ANP in the regulation of plasma volume is the relative importance of the renal versus the nonrenal actions of ANP. Renkin and Tucker (5) argued that the extrarenal actions of ANP enable it to preferentially regulate plasma volume. The study reported by Sabrane, Kuhn, and colleagues in this issue of the JCI(6) provides new data to support this hypothesis by investigating the regulation of plasma volume in transgenic mice in which one of the common receptors for ANP has been selectively deleted in vascular endothelium.
What is the role of ANP in vascular permeability?
In summary, although ANP-dependent modulation of vascular permeability was recognized soon after the discovery of ANP, the importance of changes in vascular permeability in regulating the distribution of water between the plasma space and the interstitial space has not been widely recognized. The elegant study by Sabrane, Kuhn, and colleagues (6) establishes the primary role of ANP-dependent increases in the permeability of the vascular endothelial barrier to plasma proteins in the chronic control of plasma volume. The study also points the way to important new experiments and approaches for investigating in what way defects in ANP-dependent mechanisms regulating endothelial permeability may contribute to the development of cardiovascular disease, including hypertension.
What is the main pathway for transvascular fluid transport?
The main pathway for water exchange between the plasma and interstitial space is through the intercellular cleft between adjacent endothelial cells, at sites where there are infrequent narrow breaks in the junctional strands . The glycocalyx on the endothelial cell surface forms an additional series resistance at the entrance to the intercellular cleft on the vascular side. Figure Figure1B1B illustrates details of the flow of the plasma ultrafiltrate (low-protein concentration) through the interendothelial cleft in Figure1A at the site of a break in the junctional strand. The glycocalyx has a low but finite permeability to the plasma proteins and is the main permeability barrier to plasma proteins that cross via the endothelial cleft. With this arrangement, the plasma protein concentration, with osmotic pressure πgin the very narrow space beneath the glycocalyx can be maintained at a lower level than the protein concentration in the interstitial space (with osmotic pressure πt). Relevant to the results reported by Sabrane et al. (6), the magnitude of πgcan be modified by increases or decreases in the permeability of the glycocalyx to plasma proteins. It can also be modified by changes in the tissue plasma protein concentration far away from the cleft (because of the back diffusion of the proteins from the interstitial space; see ref. 8for more details). Thus, as illustrated in Figure Figure1C,1C, the plasma protein osmotic pressure opposing fluid filtration (πc– πg) may be significantly greater than the plasma-to-tissue colloid osmotic pressure (πc– πt), and it is the magnitude of (πc– πg) rather than (πc– πt) that should be considered as the principal osmotic pressure determinant of transvascular water flow in the Starling principle. Thus, regulation of the plasma protein permeability of the glycocalyx by ANP-dependent mechanisms may be just as important as other ANP-dependent mechanisms, such as changes in the permeability of vesicular and large-pore pathways illustrated in Figure Figure1A.1A. This is an area for further investigation.
How does ANP affect plasma volume?
Atrial natriuretic peptide (ANP) acts acutely to reduce plasma volume by at least 3 mechanisms: increased renal excretion of salt and water, vasodilation, and increased vascular permeability. Authors of a study in this issue of the JCIperformed a knockout of the receptor for ANP in vascular endothelia in order to distinguish the effects of ANP-dependent increases in vascular permeability from those of other endocrine actions of ANP in the regulation of plasma volume. The knockout mice exhibited reduced vascular permeability to plasma protein, resulting in chronically increased plasma volume, arterial hypertension, and cardiac hypertrophy. Renal excretion and vasodilation did not account for these changes. Thus ANP-induced increases in endothelial permeability may be critical to the ability of ANP to lower arterial blood pressure.
Which endothelium is critically involved in the hypotensive and hypovolemic actions of atrial?
See the article "Vascular endothelium is critically involved in the hypotensive and hypovolemic actions of atrial natriuretic peptide" in volume 115 on page 1666.
What is the osmotic pressure used in the Starling principle?
It is usually assumed that the osmotic pressure due to the average interstitial protein concentration (πt) can be used in the Starling principle to describe net water flow (Jv).
What is the role of atrial natriuretic peptide in heart failure?
Atrial natriuretic peptide hormone of cardiac origin, which is released in response to atrial distension and serves to maintain sodium homeostasis and inhibit activation of the renin-angiotensin-aldosterone system. Congestive heart failure is a clinical syndrome characterized by increased cardiac volume and pressure overload with an inability to excrete a sodium load, which is associated with increased activity of systemic neurohumoral and local autocrine and paracrine mechanisms. Circulating atrial natriuretic peptide is greatly increased in congestive heart failure as a result of increased synthesis and release of this hormone. Atrial natriuretic peptide has emerged as an important diagnostic and prognostic serum marker in congestive heart failure. In early heart failure, it may play a key role in preserving the compensated state of asymptomatic left ventricular dysfunction. Despite increased circulating atrial natriuretic peptide in heart failure, the kidney retains sodium and is hyporesponsive to exogenous and endogenous atrial natriuretic peptide. The mechanism for the attenuated renal response is multifactorial and includes renal hypoperfusion, activation of the renin-angiotensin-aldosterone and sympathetic nervous systems. Therapeutic strategies to potentiate the biologic actions of atrial natriuretic peptide may prolong the asymptomatic phase and delay progression to overt congestive heart failure.
Why is the natriuretic peptide important?
Circulating atrial natriuretic peptide is greatly increased in congestive heart failure as a result of increased synthesis and release of this hormone. Atrial natriuretic peptide has emerged as an important diagnostic and prognostic serum marker in congestive heart failure. In early heart failure, it may play a key role in preserving ...
Does the kidney retain sodium?
Despite increased circulating atrial natriuretic peptide in heart failure, the kidney retains sodium and is hyporesponsive to exogenous and endogenous atrial natriuretic peptide. The mechanism for the attenuated renal response is multifactorial and includes renal hypoperfusion, activation of the renin-angiotensin-aldosterone ...
Does atrial natriuretic peptide prolong asymptomatic phase?
Therapeutic strategies to potentiate the biologic actions of atrial natriuretic peptide may prolong the asymptomatic phase and delay progression to overt congestive heart failure.

Overview
Atrial natriuretic peptide (ANP) or atrial natriuretic factor (ANF) is a natriuretic peptide hormone secreted from the cardiac atria that in humans is encoded by the NPPA gene. Natriuretic peptides (ANP, BNP, and CNP) are a family of hormone/paracrine factors that are structurally related. The main function of ANP is causing a reduction in expanded extracellular fluid (ECF) volume by incr…
Clinical significance
A member of the natriuretic peptide gene family, NPPA encodes an important cardiac signaling molecule known as atrial natriuretic peptide/factor (ANP). ANP carries out endocrine functions of the heart. It acts as a diuretic by inhibiting sodium reabsorption in the kidneys. ANP also acts in the heart to prevent cardiac hypertrophy and to regulate vascular remodeling and energy metabolism. NPPA expression is varied throughout mammalian development into adulthood. Fe…
Discovery
The discovery of a natriuretic factor (one that promotes kidney excretion of salt and water) was first reported by Adolfo José de Bold in 1981 when rat atrial extracts were found to contain a substance that increased salt and urine output in the kidney. Later, the substance was purified from heart tissue by several groups and named atrial natriuretic factor (ANF) or ANP.
Structure
ANP is a 28-amino acid peptide with a 17-amino acid ring in the middle of the molecule. The ring is formed by a disulfide bond between two cysteine residues at positions 7 and 23. ANP is closely related to BNP (brain natriuretic peptide) and CNP (C-type natriuretic peptide), which all share a similar amino acid ring structure. ANP is one of a family of nine structurally similar natriuretic hormones: seven are atrial in origin.
Production
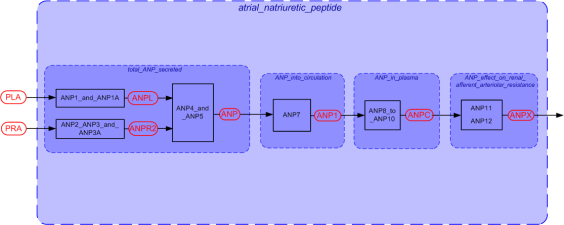
ANP is synthesized as an inactive preprohormone, encoded by the human NPPA gene located on the short arm of chromosome 1. The NPPA gene is expressed primarily in atrial myocytes and consists of 2 introns and three exons, with translation of this gene yielding a high molecular mass 151 amino acid polypeptide known as preproANP. The preprohormone is activated via post-translational modification that involves cleavage of the 25 amino acid signal sequence to produc…
Receptors
Three types of atrial natriuretic peptide receptors have been identified on which natriuretic peptides act. They are all cell surface receptors and designated:
• guanylyl cyclase-A (GC-A) also known as natriuretic peptide receptor-A (NPRA/ANPA) or NPR1
• guanylyl cyclase-B (GC-B) also known as natriuretic peptide receptor-B (NPRB/ANPB) or NPR2
Physiological effects
Maintenance of the ECF volume (space), and its subcompartment the vascular space, is crucial for survival. These compartments are maintained within a narrow range, despite wide variations in dietary sodium intake. There are three volume regulating systems: two salt saving systems, the renin angiotensin aldosterone system (RAAS) and the renal sympathetic system (RSS); and the salt excreting natriuretic peptide (NP) hormone system. When the vascular space contracts, the RAA…
Degradation
Modulation of the effects of ANP is achieved through gradual degradation of the peptide by the enzyme neutral endopeptidase (NEP). Recently, NEP inhibitors have been developed, such as Sacubitril and Sacubitril/valsartan. They may be clinically useful in treating patients in heart failure with reduced ejection fraction .