Why is the regulation of calcium levels so important?
why is regulating calcium levels so important -calcium is a vital mineral -calcium drops, blood cannot clot, muscles cannot contract, transport of materials across a cell membrane may fall.
Why is osmoregulation so important?
osmoregulation is important for body cells because it maintains the required concentrations of minerals and water in the cells .also helps in maintaining the shape and size of the cells . What is the process of osmoregulation? Osmoregulation is the process of maintaining salt and water balance (osmotic balance) across membranes within the body.
What does calcium homeostasis depend on?
Calcium homeostasis is dependent on the direction of the diffusive gradient and the UF rate. Transfer from dialysate to patient is negatively correlated with the degree of UF. Calcium homeostasis is also related to oral calcium intake, vitamin D prescription, parathyroid hormone levels, and phosphate levels.
Why is too much calcium harmful?
Too much calcium over time can cause an irregular heart beat and can lower blood pressure. In serious cases too much calcium can be damaging to the brain (and this is why calcium binding proteins are believed to be good for cognitive function). This can then result in confusion, fits and loss of consciousness.
What is the ionized form of calcium?
The ionized form is the physiologically active form . Hypercalcemia is defined as an ionized Ca + concentration greater than 2.7 mEq/L or a total serum Ca + concentration greater than 10.5 mg/dl. The most common causes are metastatic malignancy and hyperparathyroidism. The mnemonic stones, bones, psychic moans, and abdominal groans is used to remember the signs and symptoms of hypercalcemia. Treatment for hypercalcemia should be initiated in symptomatic patients, those with dehydration, or asymptomatic patients with a Ca + concentration greater than 12 mg/dl. Initial treatment is volume repletion. Medications to decrease mobilization of Ca from bone may be considered in the ED setting if the Ca + concentration is greater than 14 mg/dl or the patient is symptomatic. Glucocorticoids are used in certain cases.
What is the calcium level of a PD?
Several studies have shown that a PD solution calcium level of 1.0 to 1.25 mmol/L can lead to adequate calcium balance and phosphate control with oral calcium binders and reduces the risk of hypercalcemia. However, hypocalcemia may occur, especially if compliance with vitamin D analogs or calcium-containing phosphate binders is incomplete. Lower dialysate calcium levels are available (0.6–1.0 mmol/L) and are used by some centers in PD patients with severe hyperparathyroidism who need increasingly high doses of calcitriol. The introduction of cinacalcet in the recent past has largely obviated the need for high-dose vitamin D therapy, although low-dose supplementation is still required to prevent significant hypocalcemia. The earlier formulations containing 1.75 mmol/L are still used in hypocalcemic patients and in patients who are nonadherent to prescribed calcium or calcitriol supplements.
What is the normal calcium level?
Whereas the normal serum ionized calcium level varies from 1.15 to 1.29 mmol/L, the calcium concentration of dialysate (in which all of the calcium is ionized) usually ranges from 1.25 to 1.79 mmol/L.
How are calcium and phosphate homeostasis controlled?
Calcium and phosphate homeostases are controlled by bidirectional calcium and phosphate fluxes, occurring at the levels of intestine, bone, and kidney. The latter organ plays a central role in regulating the extracellular concentration of either ion. Sensitive and efficient regulatory mechanisms, involving extracellular calcium sensing, are triggered by changes in calcium demand or supply. Similarly, the renal handling of phosphate can adjust its capacity to meet the need for phosphate of the organism. Not only calciotropic peptides or steroid hormones are capable of modifying the different calcium and phosphate fluxes to various extents, but also a variety of local factors are implicated in the regulation of calcium and phosphate homeostasis, in order to protect the organism against a deficiency or an overload. Finally, by directly influencing renal tubular calcium and phosphate transports, or by releasing calcium from intracellular stores, calcium itself plays the role of an effector on homeostatic mechanisms.
What is the normal calcium concentration?
Normal serum calcium concentration varies between laboratories, but is usually 8.5 to 10.5 mg/dL (2.1 to 2.6 mmol/L) and it represents the sum of the three circulating fractions: 45% protein bound (albumin ∼80%, globulins ∼20%), 15% complexed to anions (citrate, bicarbonate, lactate, phosphate), and 40% free, or ionized. The ionized calcium is the physiologically active form, which is recognized by the calcium-sensing receptor (CaSR). The main hormonal regulators of ionized calcium are parathyroid hormone (PTH) and 1,25 dihydroxyvitamin D (1,25D).
What is the mechanism of calcium homeostasis?
Calcium homeostasis involves the following mechanisms: calcium absorption in the gastrointestinal tract, excretion of the calcium within the renal tubules, and deposition into or removal of the calcium from the bone.
What is the optimal calcium concentration for dialysate?
The majority of physicians now prescribe a more physiologic calcium concentration (1.25–1.55 mmol/L) because of concern relating to calcium “overload” and vascular mineralization.
What is the importance of calcium homeostasis?
Calcium homeostasis. Precise maintenance of the physiologic levels of both extracellular and intracellular ionized calcium is essential to life. Calcium and phosphate homeostasis is complex, yet three important hormones are responsible for modulating most of the extracellular control of these minerals. Parathyroid hormo ….
What are the stimuli that stimulate renal tubules?
A major stimulus to its production by proximal renal tubule cells is elevated PTH and decreased serum levels of calcium and phosphate. The absence of PTH as well as high serum calcium and phosphate levels can reduce its synthesis and secretion.
Which hormone is responsible for maintaining calcium and phosphate homeostasis?
Calcium and phosphate homeostasis is complex, yet three important hormones are responsible for modulating most of the extracellular control of these minerals. Parathyroid hormone acts directly on bone and kidney and indirectly on the intestine to maintain or restore the serum calcium level.
Does calcium decrease calcitonin?
A diminution in serum calcium decreases calcitonin production and release. The role of calcitonin in normal human physiology, however, remains in dispute. Finally, the biologically potent metabolite of vitamin D, 1,25(OH)2-D, stimulates intestinal absorption of calcium and phosphate.
What happens if you decrease Ca2+ in blood?
A decrease in Ca2+ in blood, PTH will be secreted from parathyroid gland and stimulate
What is the rapid phase of bone?
Rapid phase: begins in minutes and increases progressively for several hours, results from activation of already existing bone cells (osteocytes) to promote calcium & phosphate absorption
Can a parathyroid gland be removed?
removal of 2 parathyroid glands will not cause any abnormalities, but removal of 3 or more will cause transient hypoparathyroidism
Can thiazide cause hypercalcemia?
Hypercalcemia can also be due to thiazide diuretics.
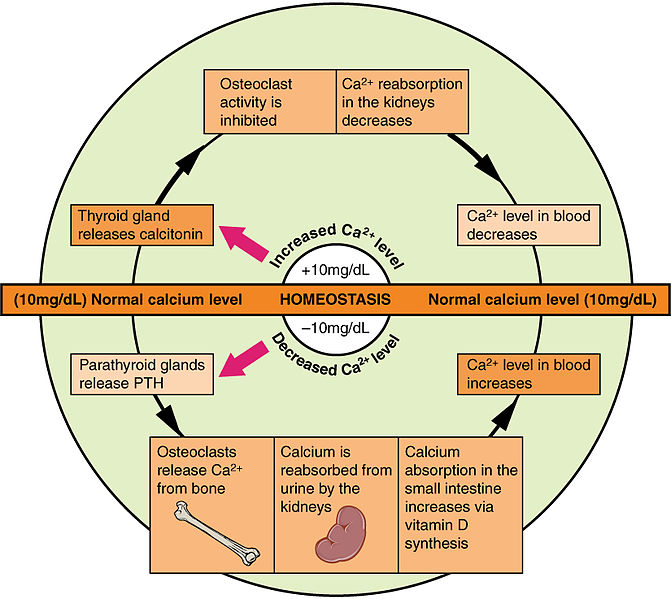
What happens when calcium levels are too high?
When blood levels of calcium get too high, the thyroid gland is stimulated to release calcitonin ( [link] ), which inhibits osteoclast activity and stimulates calcium uptake by the bones, but also decreases reabsorption of calcium by the kidneys. All of these actions lower blood levels of calcium.
What is the function of the parathyroid gland?
When calcium is not binding to these receptors, the cells release PTH, which stimulates osteoclast proliferation and resorption of bone by osteo clasts. This demineralization process releases calcium into the blood. PTH promotes reabsorption of calcium from the urine by ...
Why does the parathyroid gland not release calcium?
In the condition described, the parathyroid glands are not responding to the signal that there is sufficient calcium in the blood and they keep releasing P TH, which causes the bone to release more calcium into the blood . Ultimately, the bones become fragile and hypercalcemia can result.
Why is vitamin D important for bones?
Explain how these might be connected. Vitamin D is required for calcium absorption by the gut. Low vitamin D could lead to insufficient levels of calcium in the blood so the calcium is being released from the bones. The reduction of calcium from the bones can make them weak and subject to fracture.
How does the body regulate calcium levels?
The body regulates calcium homeostasis with two pathways; one is signaled to turn on when blood calcium levels drop below normal and one is the pathway that is signaled to turn on when blood calcium levels are elevated .
What is the process of calcium homeostasis?
Explain the process of calcium homeostasis. Calcium is not only the most abundant mineral in bone, it is also the most abundant mineral in the human body. Calcium ions are needed not only for bone mineralization but for tooth health, regulation of the heart rate and strength of contraction, blood coagulation, contraction ...
What is the cause of low calcium levels?
Hypocalcemia , a condition characterized by abnormally low levels of calcium, can have an adverse effect on a number of different body systems including circulation, muscles, nerves, and bone. Without adequate calcium, blood has difficulty coagulating, the heart may skip beats or stop beating altogether, muscles may have difficulty contracting, nerves may have difficulty functioning, and bones may become brittle. The causes of hypocalcemia can range from hormonal imbalances to an improper diet. Treatments vary according to the cause, but prognoses are generally good.
What happens when calcium levels fall?
If the serum calcium level falls, the parathyroid glands release PTH into the blood and this signals cells in bone (osteoclasts) to release calcium from the bone surfaces. PTH also signals the kidney to reclaim more calcium before it is excreted in the urine and also stimulates synthesis of the active form of vitamin D.
Which hormone is released by the thyroid gland?
Special cells that reside in the thyroid gland along with thyroid hormone containing cells release another hormone, calcitonin, into the blood. Calcitonin signals osteoclasts to slow down removal of calcium from bone; this action tends to lower levels of blood calcium.
Where does PTH come from?
PTH comes from the parathyroid glands located behind the thyroid gland in the lower part of the neck and calcitonin comes from cells in the thyroid gland, both of which monitor and maintain calcium levels in the blood. The active form of vitamin D is synthesized in the kidney under the control of PTH. Special cells that reside in the thyroid gland ...
Which hormone regulates calcium levels in the blood?
There are at least three hormones intimately involved in the regulation of the level of calcium in the blood: parathyroid hormone (PTH), calcitonin and calcitriol (1, 25 dihydroxyvitamin D, the active form of vitamin D).
How does the body maintain calcium levels?
How the Body Maintains Calcium Levels. The body maintains very tight control over the calcium circulating in the blood at any given time. The equilibrium is maintained by an elegant interplay of calcium absorbed from the intestines, movement of calcium into and out of the bones, and the kidney’s reclamation and excretion of calcium into the urine.
Does shutting off calcitonin release calcium?
Conversely, shutting off calcitonin allows osteoclasts to get back in business to release needed calcium from bone. The PTH system provides long-term, day-to-day regulation of calcium levels by many hormones working in concert.
Does the body release calcium from bones?
The body also has a minute to minute regulation of calcium levels from osteocytes in bone—these cells can instantly release needed calcium or instantly stop releasing calcium depending on immediate needs (too little or too much calcium coming into the bloodstream).
What is the role of calcium in the kidney?
The kidney plays a key role in this process by the fine regulation of calcium excretion. More than 95% of filtered calcium is reabsorbed along the renal tubules. In the proximal tubules, 60% of filtered calcium is reabsorbed by passive mechanisms. In the thick ascending limb, 15% of calcium is reabsorbed by paracellular diffusion through paracellin-1 (claudin-16). The calcium sensing receptor (CaSR) in the basolateral membrane of the thick ascending limb senses the change in iCa2+and inhibits calcium reabsorption independent to PTH and 1,25(OH)2D3. The fine regulation of calcium excretion occurs in the distal convoluted tubules and connecting tubules despite the fact that only 10-15% of filtered calcium is reabsorbed there. Transient receptor potential vanilloid 5 (TRPV5) and 6 (TRPV6) in the apical membrane act as the main portal of entry, calbindin-D28Kdelivers Ca2+in the cytoplasm, and then Na2+/Ca2+exchanger (NCX1) and plasma membrane Ca2+-ATPase in the basolateral membrane serve as an exit. In the cortical collecting duct, TRPV6 is expressed, but the role might be negligible. In addition to PTH and 1,25(OH)2D3, acid-base disturbance, diuretics, and estrogen affect on these calcium channels. Recently, klotho and fibroblast growth factor 23 (FGF23) are suggested as new players in the calcium metabolism. Klotho is exclusively expressed in the kidney and co-localized with TRPV5, NCX1, and calbindin-D28K. Klotho increases calcium reabsorption through trafficking of TRPV5 to the plasma membrane, and also converts FGF receptor to the specific FGF23 receptor. FGF23:klotho complex bound to FGF receptor inhibits 1α-hydroxylase of vitamin D, and contributes to calcium reabsorption and phosphate excretion in the kidney.
How many kDa is FGF23?
The full length of FGF23 is about 30 kDa, and then inactivated by cleavage to 18 kDa N-terminal fragment and 12 kDa C-terminal fragment24). (b) Suggested mechanism of the FGF23:klotho complex action; Klotho binds to FGF receptor (FGFR) and converts it to a specific receptor for FGF23.
How much calcium is absorbed in the renal system?
About 50% of plasma calcium (ionized and complexed form; ultrafilterable fraction, excluding the protein bound form) is freely filtered through the renal glomerulus, and 99% of the filtered calcium is actually reabsorbed along renal tubules (Table 1). The excreted calcium in the final urine is about 200 mg per day in an adult person with an average diet. Several factors are involved in the regulation of calcium in renal tubules. PTH and activated vitamin D enhance calcium reabsorption in the thick ascending limb (TAL), distal convoluted tubule (DCT) and/or connecting tubule (CNT), and estrogen promotes calcium absorption in the DCT/CNT1, 2). Acidosis contributes to hypercalciuria by reducing calcium reabsorption in the proximal tubule (PT) and DCT, and alkalosis vice versa3). Diuretics like thiazide and furosemide also alter calcium absorption in the renal tubules; thiazide promotes calcium reabsorption and furosemide inhibits it4, 5). Plasma calcium itself also controls renal calcium absorption through altered PTH secretion as well as via binding to the calcium sensing receptor (CaSR) in the TAL. To facilitate Ca2+reabsorption along renal tubules; (i) voltage difference between the lumen and blood compartment should be favorable for Ca2+passage, i.e., a positive voltage in the lumen; (ii) concentration difference should be favorable for Ca2+passage with a higher Ca2+concentration in the lumen; (iii) an active transporter should exist if the voltage or concentration difference is not favorable for Ca2+reabsorption. Each renal tubular segment has a different Ca2+concentration difference or voltage environment for its unique mechanism for calcium reabsorption.
Where is klotho expressed?
Recently, klotho and fibroblast growth factor 23 (FGF23) are suggested as new players in the calcium metabolism. Klotho is exclusively expressed in the kidney and co-localized with TRPV5, NCX1, and calbindin-D28K.
What factors affect calcium absorption in renal tubules?
Several factors are involved in the regulation of calcium in renal tubules. PTH and activated vitamin D enhance calcium reabsorption in the thick ascending limb (TAL), distal convoluted tubule (DCT) and/or connecting tubule (CNT), and estrogen promotes calcium absorption in the DCT/CNT1, 2).
What percentage of calcium is protein bound?
Approximately 40% of plasma calcium is protein-bound and 10% of calcium is in a complex with anions like phosphate, citrate, and sulfate etc. Only half of plasma calcium is in its free form (ionized form, iCa2+) and physiologically important1). The ionized calcium is tightly regulated by hormones like parathyroid hormone (PTH), ...
How much calcium is in the body?
Total body calcium in the adult human is about 1-2 kg and 99% of total calcium exists in bone. Even though only less than 1% of body calcium is in the extracellular space, maintaining the extracellular calcium concentration within a narrow range (8.5-10.5 mg/dL) is very important for calcium homeostasis. Approximately 40% of plasma calcium is ...
How much calcium is released from bone?
Although calcium flow to and from the bone is neutral, about five mmol is turned over a day. Bone serves as an important storage point for calcium, as it contains 99% of the total body calcium. Calcium release from bone is regulated by parathyroid hormone. Calcitonin stimulates incorporation of calcium in bone.
What is the role of calcium in homeostasis?
Key Points. Calcium homeostasis regulates calcium flow to and from the bones. Inadequate calcium levels can result in osteoporosis. Calcium release from bone is regulated by parathyroid hormone. Calcitriol regulates the levels of calcium and phosphorus in the blood and helps maintain a healthy skeletal system.
What is the mechanism by which the body maintains adequate calcium levels in order to prevent hypercalcemia or hypocalcemia?
calcium homeostasis: Calcium homeostasis is the mechanism by which the body maintains adequate calcium levels in order to prevent hypercalcemia or hypocalcemia, both of which can have important consequences for health. calcidiol: A prehormone that is produced in the liver by the hydroxylation of vitamin D3 ...
How does bone resorption affect calcium levels?
The process of bone resorption by the osteoclasts releases stored calcium into systemic circulation and is an important process for regulating calcium balance. As bone formation actively fixes circulating calcium in its mineral form by removing it from the bloodstream, resorption actively unfixes it, thereby increasing circulating calcium levels.
What happens when the calcium level of the thyroid gland increases?
When blood calcium concentration rises, the parafollicular cells of the thyroid gland increase calcitonin secretion into the blood. At the same time, the parathyroid glands reduce parathyroid hormone secretion into the blood. The resulting high levels of calcitonin in the blood stimulate the bone to remove calcium from the blood plasma and deposit it as bone.
What is the enzyme that produces calcidiol?
calcidiol: A prehormone that is produced in the liver by the hydroxylation of vitamin D3 (cholecalciferol) by the enzyme cholecalciferol 25-hydroxylase. Calcium metabolism or calcium homeostasis is the mechanism by which the body maintains adequate calcium levels.
What happens when calcium levels are too low?
Removal of calcium from the bone is also inhibited. When the blood calcium level is too low, calcitonin secretion is inhibited and PTH secretion is stimulated . This results in the removal of calcium from the bone to correct blood calcium levels.
How does PTH affect calcium levels?
PTH acts to increase serum calcium by increasing active vitamin D and stimulating bone remodeling. It is regulated primarily by serum calcium with some contribution from circulating vitamin D levels.
What hormone is secreted by parathyroid cells?
Parathyroid hormone ( PTH) is a protein hormone synthesized, processed and secreted by the parathyroid chief cells in response to changes in serum ionized calcium levels. Drop in serum calcium levels trigger secretion of PTH via reduced binding to the calcium sensing receptors ( CaSR ). Furthermore, a rise in vitamin D levels suppress PTH secretion.
What are the effects of PTH on the kidneys?
Parathyroid hormone actions: Major effects of PTH are mediated in kidneys and bone . Renal effects. Increased calcium reabsorption: Stimulates calcium transport in the DCT and the thick ascending loop of henle (TALH) through up-regulation of TRPV5 (calcium channel) and calbindin both directly and indirectly via rise in vitamin D levels.
How is calcium homeostasis controlled?
Figure 1: Calcium homeostasis is a process controlled by chiefly by hormones vitamin D and PTH. Vitamin D enters circulation via synthesis in the skin or intestinal absorption and is subsequently converted to its active form, 1,25 (OH) 2 D via separate hydroxylation processes in the liver and kidneys. Both 25 (OH)D and 1,25 (OH) 2 D are regulated by classical negative feedback. PTH acts to increase serum calcium by increasing active vitamin D and stimulating bone remodeling. It is regulated primarily by serum calcium with some contribution from circulating vitamin D levels.
How does vitamin D increase production?
Increases vitamin D production: Stimulates hydroxylation of vitamin D by rapidly inducing transcription of 1α-hydroxylase in the proximal tubule. Inhibits transcription of 24-hydroxylase gene in proximal tubule increasing availability of active form of vitamin D. Bone effects.
What is the goal of calcium homestasis?
The overall goal of calcium homestasis is to maintain biologically active ionized [Ca] within a narrow acceptable range (1.1-1.4 mmol/L) in order for critical functions such as signal transduction, neuronal activation and muscle contraction to work.
Which hormone is produced in the parafollicular cells of the thyroid gland?
Calcitonin. Produced in the parafollicular cells of the thyroid gland, calcitonin acts to correct hypercalcemia by directly opposing the effects of PTH by inhibiting intestinal absorption of calcium, inhibiting osteoclastic activity and inhibiting reabsorption of calcium in the nephron.