Unfractionated Heparin (UFH) is a fast-acting blood thinner that works together with antithrombin, a natural protein in the body, to block clot formation. Specifically, UFH binds to antithrombin and enhances its ability to inhibit two of the body’s most potent clotting factors – factor Xa and factor IIa – usually within minutes.
What drugs prevent clotting?
- glycoprotein platelet inhibitors
- platelet aggregation inhibitors
- protease-activated receptor-1 antagonists
What are the side effects of heparin?
The more common side effects of this drug include:
- bruising more easily
- bleeding that takes longer to stop
- irritation, pain, redness, or sores at the injection site
- allergic reactions, such as hives, chills, and fever
- increased liver enzymes on liver function test results
What is the antidote for heparin?
The activity of this heparin is reversible with the use of an antidote named protamine. This synthetic heparin is cheaper and safer according to the researchers. Owing to these factors, there has been a significant increase in the growth impetus in the ...
Is heparin an anticoagulant?
The heparins are a group of anticoagulants that consist of unfractionated heparin, low molecular weight heparins, and heparinoids.
See more
How quickly does heparin break up a clot?
It is usually given in the hospital by IV (a small needle inserted in a vein), but it can also be given by an injection under the skin. IV heparin works rapidly; within minutes of receiving it, most patients have excellent anticoagulation that will prevent further clotting.
Does heparin break down existing clots?
Heparin will not dissolve blood clots that have already formed, but it may prevent the clots from becoming larger and causing more serious problems.
What does heparin do to blood clots?
Heparin is a drug that stops your blood from clotting or forming blood clots. It is also called an anticoagulant or a blood thinner.
How does heparin stop clotting?
Heparin is a medication that inhibits clotting by activating your body's anti-clotting processes. One of the anticlotting processes uses a type of blood protein called antithrombin. Heparin works by activating antithrombin, and then antithrombin keeps other parts of the clotting process from working normally.
What's the most common side effect of heparin?
The more common side effects of this drug include: bruising more easily. bleeding that takes longer to stop. irritation, pain, redness, or sores at the injection site.
What is the miracle drug that dissolves blood clots?
tPA quickly dissolves the clots that cause many strokes. By opening a blocked blood vessel and restoring blood flow, tPA can reduce the amount of damage to the brain that can occur during a stroke. To be effective, tPA and other drugs like it must be given within a few hours of the stroke symptoms beginning.
How do I know if heparin is working?
Monitoring heparin with daily blood testing. Patients treated with heparin are monitored by a blood test daily to see if their dose is optimal. The blood test used to check a patient's heparin level is the activated partial thromboplastin time (aPTT).
What is most serious complication with heparin?
Hemorrhage, the most frequent and most feared complication of heparin therapy, does not occur spontaneously in all patients receiving large doses of heparin. However, in certain populations, hemorrhage must be anticipated and appropriate modifications made in the heparin dosage.
Why is heparin only given in the hospital?
Patients who are unable to get out of bed in the days following surgery are at greater risk of forming clots, making heparin a commonly used drug in intensive care units.
What is the main action of heparin?
Heparin is a sulfated polysaccharide with a molecular weight range of 3000 to 30 000 Da (mean, 15 000 Da). It produces its major anticoagulant effect by inactivating thrombin and activated factor X (factor Xa) through an antithrombin (AT)-dependent mechanism.
What is the mechanism of action of heparin?
Heparins bind to antithrombin (AT) and induce a conformational change that makes AT an efficient inactivator of coagulation factors. Unfractionated heparin inhibits thrombin (factor IIa) by forming a ternary complex.
Why would heparin be stopped immediately?
Results and conclusions: The severe morbidity and potential mortality associated with heparin-induced thrombocytopenia are caused mainly by thrombosis. If it is suspected, all heparin products should be immediately stopped. Platelet counts usually return to normal after the heparin is discontinued.
Do blood thinners break up existing clots?
Blood-thinning medications are commonly used to prevent blood clots from forming or getting bigger. Thrombolytic medications can break up existing clots.
Do blood thinners help existing blood clots?
Blood thinners are medicines that prevent blood clots from forming. They do not break up clots that you already have. But they can stop those clots from getting bigger. It's important to treat blood clots, because clots in your blood vessels and heart can cause heart attacks, strokes, and blockages.
When should you not use heparin?
You should not use heparin if you have uncontrolled bleeding or a severe lack of platelets in your blood. Do not use this medicine if you have ever been diagnosed with “heparin-induced thrombocytopenia,” or low platelets caused by heparin or pentosan polysulfate.
Can blood clots dissolve without blood thinners?
Typically, your body will naturally dissolve the blood clot after the injury has healed. Sometimes, however, clots form on the inside of vessels without an obvious injury or do not dissolve naturally. These situations can be dangerous and require accurate diagnosis and appropriate treatment.
What is the purpose of protamine sulfate?
Protamine sulfate has been given to counteract the anticoagulant effect of heparin (1 mg per 100 units of heparin that had been given over the past four hours). It may be used in those who overdose on heparin or to reverse heparin's effect when it is no longer needed.
Why is heparin complex?
The three-dimensional structure of heparin is complicated because iduronic acid may be present in either of two low-energy conformations when internally positioned within an oligosaccharide. The conformational equilibrium is influenced by sulfation state of adjacent glucosamine sugars.
Why is heparin given intravenously?
Heparin is given parenterally because it is not absorbed from the gut, due to its high negative charge and large size. It can be injected intravenously or subcutaneously (under the skin); intramuscular injections (into muscle) are avoided because of the potential for forming hematomas. Because of its short biologic half-life of about one hour, heparin must be given frequently or as a continuous infusion. Unfractionated heparin has a half-life of about one to two hours after infusion, whereas LMWH has a half-life of four to five hours. The use of LMWH has allowed once-daily dosing, thus not requiring a continuous infusion of the drug. If long-term anticoagulation is required, heparin is often used only to commence anticoagulation therapy until an oral anticoagulant e.g. warfarin takes effect.
How much heparin saline flush is needed for angiography?
In angiography, 2 to 5 units/ml of unfractionated heparin saline flush is used to prevent the clotting of blood in guidewires, sheaths, and catheters, thus preventing thrombus from dislodging from these devices into the circulatory system .
What is heparin used for?
As a medication it is used as an anticoagulant. Specifically it is also used in the treatment of heart attacks and unstable angina. It is given by injection into a vein or under the skin.
Why did Dennis Quaid overdose on heparin?
The overdose allegedly arose because the labeling and design of the adult and infant versions of the product were similar. The Quaid family subsequently sued the manufacturer, Baxter Healthcare Corp., and settled with the hospital for $750,000. Prior to the Quaid accident, six newborn babies at Methodist Hospital in Indianapolis, Indiana, were given an overdose. Three of the babies died after the mistake.
How long does it take for hyperkalemia to appear after heparin?
The hyperkalemia can appear within a few days after the onset of heparin therapy.
Can blood clots in the leg come back after being treated with heprin?
Yes: Having a previous DVT increases the risk of recurrent DVT after you stop blood thinners. In unusual situations patient can develop new clots while on ... Read More
How can blood clots dissolve?
Blood clot removal: Blood clots in general are removed naturally from the body. The body has a system of clotting as well as a system to prevent too much clotting. Whenev... Read More
What is the treatment for clotting HX?
Clotting hx ?'s: Pregnancy with a history of clotting is treated usually with Lovenox or heparin for effective reduction of clotting incidence. Both medications are ef... Read More
Why do blood clots form in the heart?
Variety of causes: A variety of disorders can result in a blood clot within the heart. These range from genetic disorders to trauma to cancer syndromes. Most clots diss... Read More
What does "thin your blood" mean?
To thin you blood: To thin your blood to keep the clots from progressing.
How long does it take to video chat with a doctor?
Video chat with a U.S. board-certified doctor 24/7 in less than one minute for common issues such as: colds and coughs, stomach symptoms, bladder infections, rashes, and more.
Can you take Xarelto as prescribed?
Chances low: take the xarelto as prescribed and continue regular follow up wth your doc. Keep well hydrated.
Why do you need blood thinners?
Blood thinners are also used to help prevent clots after a stroke or pulmonary embolism (when a blood clot travels to an artery in your lungs ). Blood thinners don’t dissolve the clot, but they can stop it from getting bigger and keep new ones from forming. That gives your body time to break up the clot.
How do blood thinners work?
Different blood thinners work in different ways: 1 Direct oral anticoagulants (DOACs) keep your body from making fibrin, the protein the forms the clot’s mesh. 2 Heparin keeps one of your body’s key clotting proteins, thrombin, from doing its job. 3 Warfarin ( Coumadin) slows down your liver ’s ability to make the proteins you need for clotting.
How long does it take for a pulmonary embolism to dissolve?
A DVT or pulmonary embolism can take weeks or months to totally dissolve. Even a surface clot, which is a very minor issue, can take weeks to go away. If you have a DVT or pulmonary embolism, you typically get more and more relief as the clot gets smaller.
How does the body turn on a clot?
To turn it on, your body releases a substance known as an activator. It wakes up plasmin and tells it to get to work tearing things down. That mainly means breaking up the mesh-like structure that helps the clot work so well.
What is the protein that is released when you heal a clot?
When your body senses that you’ve healed, it calls on a protein called plasmin. Here’s the clever part: Plasmin is actually built into the clot itself. It’s there the whole time, but it’s turned off. It just hangs out and waits. To turn it on, your body releases a substance known as an activator.
How does heparin work?
Heparin keeps one of your body’s key clotting proteins, thrombin, from doing its job .
What happens if you have a pulmonary embolism?
You also may get sores called ulcers. About 4 in 100 people with a pulmonary embolism have long-term lung damage known as pulmonary hypertension. This means you have high blood pressure in your lungs, which can lead to issues like shortness of breath, tiredness, and chest pain.
What is unfractionated hematocrit?
Unfractionated Heparin (UFH) is a fast-acting blood thinner that works together with antithrombin, a natural protein in the body, to block clot formation. Specifically, UFH binds to antithrombin and enhances its ability to inhibit two of the body’s most potent clotting factors – factor Xa and factor IIa – usually within minutes.
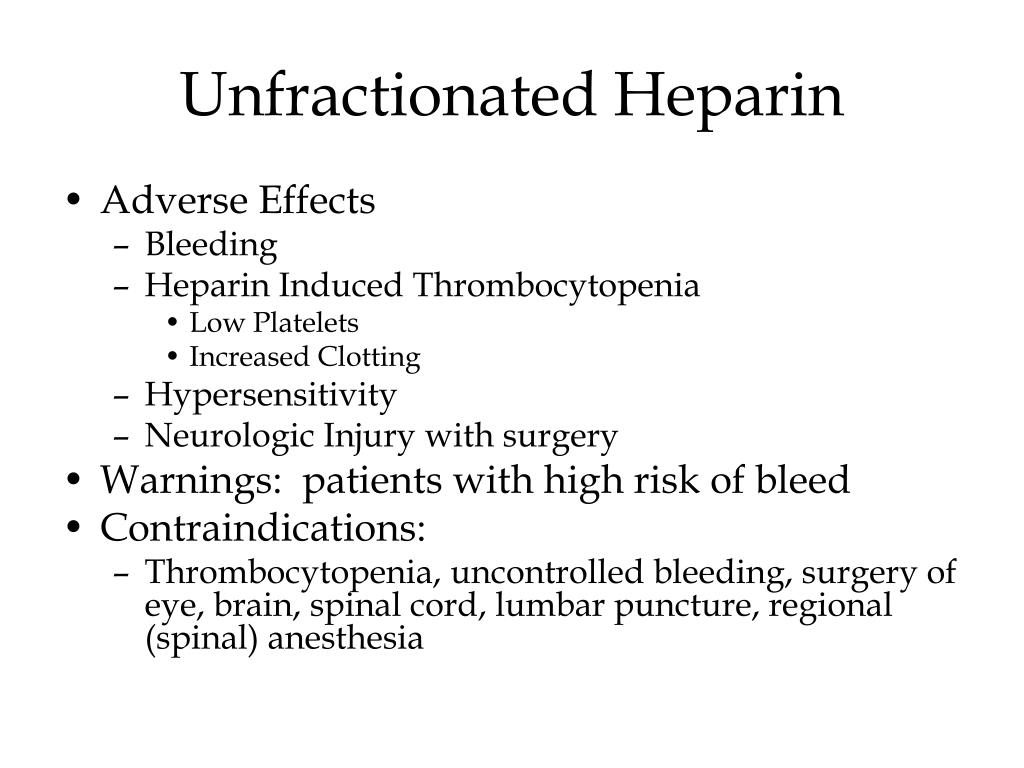
What are the side effects of heparin injection?
Uncontrolled bleeding (most serious side effect) Injection site reactions such as redness and irritation. Loss of bone strength. Elevated liver enzymes. Heparin induced thrombocytopenia (HIT) UFH is the preferred treatment for patients at high risk of bleeding complications, due to its short activity and reversibility.
Is heparin safe for pregnant women?
Heparins are the preferred anticoagulants for pregnant women because they don’t’ cross the placenta and, thus, are considered safe for the fetus. However, Low Molecular Weight Heparin (LMWH) is usually the treatment of choice over UFH in obstetrics for a variety of reasons.
Is a HIT more common than a LMWH?
HIT is 10-fold more common with UFH than LMWH. These antibodies result in a reduction in the number of platelets and cause clot formation. HIT is sometimes referred to inaccurately as “heparin allergy”.
Overview
Medical use
Heparin acts as an anticoagulant, preventing the formation of clots and extension of existing clots within the blood. While heparin itself does not break down clots that have already formed (unlike tissue plasminogen activator), it allows the body's natural clot lysis mechanisms to work normally to break down clots that have formed. Heparin is generally used for anticoagulation for the foll…
History
Heparin was discovered by Jay McLean and William Henry Howell in 1916, although it did not enter clinical trials until 1935. It was originally isolated from dog liver cells, hence its name (hepar or "ήπαρ" is Greek for "liver"; hepar + -in).
McLean was a second-year medical student at Johns Hopkins University, and was working under the guidance of Howell investigating pro-coagulant preparations, when he isolated a fat-soluble …
Adverse effects
A serious side-effect of heparin is heparin-induced thrombocytopenia (HIT), caused by an immunological reaction that makes platelets a target of immunological response, resulting in the degradation of platelets, which causes thrombocytopenia. This condition is usually reversed on discontinuation, and in general can be avoided with the use of synthetic heparins. Not all patients with heparin antibodies will develop thrombocytopenia. Also, a benign form of thrombocytopeni…
Physiological function
Heparin's normal role in the body is unclear. Heparin is usually stored within the secretory granules of mast cells and released only into the vasculature at sites of tissue injury. It has been proposed that, rather than anticoagulation, the main purpose of heparin is defense at such sites against invading bacteria and other foreign materials. In addition, it is observed across a number of widely different species, including some invertebrates that do not have a similar blood coagul…
Pharmacology
In nature, heparin is a polymer of varying chain size. Unfractionated heparin (UFH) as a pharmaceutical is heparin that has not been fractionated to sequester the fraction of molecules with low molecular weight. In contrast, low-molecular-weight heparin (LMWH) has undergone fractionation for the purpose of making its pharmacodynamics more predictable. Often either UFH or LMWH can be u…
Chemistry
Native heparin is a polymer with a molecular weight ranging from 3 to 30 kDa, although the average molecular weight of most commercial heparin preparations is in the range of 12 to 15 kDa. Heparin is a member of the glycosaminoglycan family of carbohydrates (which includes the closely related molecule heparan sulfate) and consists of a variably sulfated repeating disaccharide unit. The mai…
Other functions
• Blood specimen test tubes, vacutainers, and capillary tubes that use the lithium salt of heparin (lithium heparin) as an anticoagulant are usually marked with green stickers and green tops. Heparin has the advantage over EDTA of not affecting levels of most ions. However, the concentration of ionized calcium may be decreased if the concentration of heparin in the blood specimen is too high. Heparin can interfere with some immunoassays, however. As lithium hepar…