The receptor for insulin is a large protein that binds to insulin and passes its message into the cell. It has several functional parts. Two copies of the protein chains come together on the outside of the cell to form the receptor site that binds to insulin.
What kind of receptor does insulin use?
The insulin receptor ( IR) is a transmembrane receptor that is activated by insulin, IGF-I, IGF-II and belongs to the large class of receptor tyrosine kinase.
What are the normal levels of insulin?
Normal insulin levels for non-diabetics are usually between 60 and 100 mg/dl and may rise to 140 mg/dl after eating, reports the University of California. Diabetics may have insulin levels that range from as low as 25 mlU/L at fasting to as high as 30-230 mlU/L after recent glucose administration, reports Medscape.
What are insulin receptors called?
The insulin receptor (IR) exists in two alternatively spliced isoforms, IR-A and IR-B. The IGF-2 signaling molecule binds both its innate IGF-1 receptor as well as the insulin receptor variant A ( IR-A) with high affinity. Mitogenic and proliferative signaling via the canonical IGF-2 pathway is, therefore, augmented by IR-A.
Can your insulin stop working?
Your body does not reject injected insulin, however, if you are finding doses you are used to are not working as well or you are needing much higher doses, there could be a number of reasons for this. The first thing to check is the insulin itself.

How does insulin bind to insulin receptors?
The receptor belongs to the receptor tyrosine kinase superfamily and has orthologues in all metazoans. The structure of the unbound extracellular domain ("apo-receptor") has been solved. Insulin binds to two distinct sites on each a subunit of the receptor, crosslinking the two receptor halves to create high affinity.
How does insulin bind target tissue?
Insulin receptors (comprising 2 α and 2 β subunits) are present on the surface of target cells such as liver, muscle and fat. Insulin binding results in tyrosine autophosphorylation of the β subunit. This then phosphorylates other substrates so that a signalling cascade is initiated and biological responses ensue.
Does insulin bind to a receptor on the cell membrane?
The receptor for insulin is a large protein that binds to insulin and passes its message into the cell. It has several functional parts. Two copies of the protein chains come together on the outside of the cell to form the receptor site that binds to insulin.
What receptors do insulin act on?
Insulin activates the insulin receptor tyrosine kinase (IR), which phosphorylates and recruits different substrate adaptors such as the IRS family of proteins. Tyrosine phosphorylated IRS then displays binding sites for numerous signaling partners.
What is the mechanism of action of insulin in the body?
Insulin initiates its action by binding to a glycoprotein receptor on the surface of the cell. This receptor consists of an alpha-subunit, which binds the hormone, and a beta-subunit, which is an insulin-stimulated, tyrosine-specific protein kinase.
How does the binding of insulin to its receptor stimulate glucose uptake from the bloodstream?
How does the binding of insulin to its receptor stimulate glucose uptake from the bloodstream? It stimulates insertion of GLUT4 transporters in the cell membrane. It turns on genes so that more GLUT4 channel is made. It causes liver cells to release GLUT4.
Where are the receptors for insulin located quizlet?
The insulin receptor has two alpha units on the outside of the cell membrane and two beta units that extend from the membrane to the inside of the cell. The two alpha units allow insulin to bind to the insulin receptor, and the beta chains contain tyrosine protein kinase domains.
How many insulin receptors are in a cell?
Scatchard analysis of binding were biphasic and showed high affinity sites with a Kd of about 1.5 nM and capacity of about 10,000 receptors per cell; low affinity sites were much more numerous with a Kd of 88 nM for mouse and 998 nM for rat.
How does the cellular receptor for insulin work?
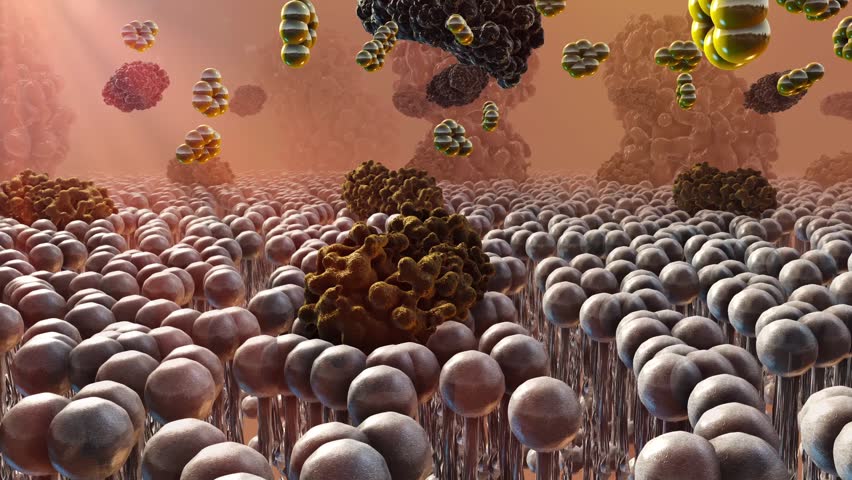
The cellular receptor for insulin helps control the utilization of glucose by cells Cells throughout the body are fueled largely by glucose that is delivered through the bloodstream . A complex signaling system is used to control the process, ensuring that glucose is delivered when needed and stored when there is a surplus. Two hormones, insulin and glucagon, are at the center of this signaling system. When blood glucose levels drop, alpha cells in the pancreas release glucagon, which then stimulates liver cells to release glucose into the circulation. When blood glucose levels rise, on the other hand, beta cells in the pancreas release insulin, which promotes uptake of glucose for metabolism and storage. Both hormones are small proteins that are recognized by receptors on the surface of cells. Signal Transduction The receptor for insulin is a large protein that binds to insulin and passes its message into the cell. It has several functional parts. Two copies of the protein chains come together on the outside of the cell to form the receptor site that binds to insulin. This is connected through the membrane to two tyrosine kinases, shown here at the bottom. When insulin is not present, they are held in a constrained position, but when insulin binds, these constraints are released. They first phosphorylate and activate each other, and then phosphorylate other proteins in the signaling network inside the cell. Since the whole receptor is so flexible, researchers have determined its structure in several pieces: the insulin-binding portion is shown here from PDB entry 3loh , the transmembrane segment from 2mfr , and the tyrosine kinase from 1irk . When Things Go Wrong Problems with insulin signaling can impair the proper management of glucose levels in the blood, leading to Continue reading >>
How does insulin work in diabetes?
It focuses on the recent discovery of how the hormone insulin actually binds to the receptor on the surface of cells, as determined by Professor Mike Lawrence's laboratory at the Walter and Eliza Hall Institute. Insulin binds to the receptor protein on the cell surface and instructs the cell to take up glucose from the blood for use as an energy source. In type 2 diabetes, we believe that insulin binds to the receptor normally, but the signal is not sent into the cell, the cells do not take up glucose and the resulting high blood glucose levels cause organ damage over time. Understanding how insulin interacts with its receptor is fundamental to the development of novel insulin for the treatment of diabetes. Maja Divjak, 2015 Continue reading >>
How does insulin affect our metabolism?
This is essential for brain function. Regardless of large fluctuations in physical activity and food intake, blood sugar levels are held within very narrow limits. The key to this is insulin, the secretion of which is closely regulated by circulating substrates of energy metabolism. Insulin signals food abundance and initiates uptake and storage of carbohydrates, fats and amino acids. Energy supply and stability of blood sugar levels postprandial is usually accorded to glucagon and the catecholamines, but the reduction in insulin signalling postprandial is almost certainly just as important. How does insulin influence our metabolism? What are the key events in its action? Control of the key enzymes of metabolism can be divided into two classes: 1. Covalent modification of enzymes, usually by phosphorylation or dephosphorylation of serine, threonine or tyrosine residues. 2. Allosteric feedback and feed-forward regulation by metabolic intermediates. Enzymes involved in metabolism can be either activated or inactivated by phosphorylation. Examples or this are glycogen phosphorylase and hormone-sensitive lipase which are activated when phosphorylated and glycogen synthetase and pyruvate dehydrogenase are inactivated through phosphorylation. The protein kinases that catalyze phosphorylation of these enzymes are subject to control through cyclic nucleotides (PKA and cyclic AMP), Ca++ and diacylglycerol (PKC) and PI (3,4,5P)P3 (PKB). The extent of enzyme phosphorylation is controlled by the balance between protein kinases and protein phosphatases. The picture becomes extremely complex when one knows that protein kinases can act Continue reading >>
What is type 2 diabetes?
According to the medical literature, type 2 diabetes is a disease characterized by chronic hyperglycemia, i.e., abnormally high concentrations of blood sugar (serum glucose), in the presence of adequate amounts of insulin. This hyperglycemia is attributed to insulin resistance, a faulty condition in which serum insulin cannot act on insulin receptors in the walls of cells. This condition prevents the receptors from allowing glucose to pass from the blood into the cells. According to the biochemical literature, an insulin receptor is a protein molecule located in the wall of a cell. The structure of the molecule is such that a smaller molecule called a ligand may attach to it. There are two kinds of ligands: an agonist, which causes the receptor to function, and an antagonist, which does nothing but prevent the agonist from attaching to the receptor. Without an attached ligand, an insulin receptor cannot allow glucose molecules to pass from the blood into a cell. An insulin molecule is an agonist, and when one becomes a ligand, an insulin receptor can allow glucose molecules to pass into a cell. But the hormone cortisol is an insulin antagonist, and when a cortisol molecule becomes a ligand, it prevents an insulin molecule from becoming a ligand, which prevents glucose from passing from the blood into the cell involved. I believe that the action of cortisol as an insulin antagonist is a reasonable explanation of the condition that we call insulin resistance, in which case there is nothing wrong with the insulin receptors or the insulin. Insulin resistance, then, would be part of the natural functioning of an insulin receptor. There are reasons to believe that the brain is responsible for the production of excess cortisol for the purpose of preventing the loss of serum gl Continue reading >>
How does insulin interact with the IR?
When Insulin interacts with the , a part of the Insulin Receptor (IR), it triggers a phosphorylation cascade starting in the holoreceptor's tyrosine kinase domain. This leads to the introduction of glucose into the cell. Without Insulin, glucose is prevented from entering the cell; thus, Insulin's interaction with the IR regulates the intracellular concentration of glucose. Until recently, the Insulin-IR binding mechanism was unknown. We will uncover the newly discovered mechanisms between Insulin and its receptor by highlighting the interactions that solidify its binding. II. General Structure Turn spin on/off Insulin is stored as a zinc-coordinated hexamer. However, this hexamer dissociates into zinc-free monomers that are able to bind to the IR. A single Insulin monomer has two chains - and - that are connected by three disulfide bonds (Figure 1), one of which is an intramolecular disulfide bond on Chain A. Both of these chains are needed for Insulin to interact with its receptor. Figure 1: Disulfide Bonds in an Insulin Monomer The Insulin receptor is a heterotetramer consisting of multiple subunits. Each IR monomer includes an alpha-subunit leucine-rich repeat domain (L1 Beta Two Sheet) combined with a cysteine-rich domain (CR) , as well as an alpha-subunit C-terminal segment (alpha-CT) . These are located in the extracellular matrix and constitute the . The supplementary image shows an additional leucine-rich repeat domain (L2) and the first, second, and third fibronectin type III domains, which, combined with the microreceptor, constitute the holoreceptor. There are two isoforms of th Continue reading >>
What is the IR of insulin?
The insulin receptor (IR) is a large, disulphide-linked, glycoprotein that spans the cell membrane with its insulin binding surfaces on the outside of the cell and its tyrosine kinase domains on the inside. IR is a symmetrical homodimer that contains two identical binding pockets, each created by the juxtapositioning of two distinct binding sites involving residues from both IR monomers (IR and IR´). The two binding pockets comprise site 1/site 2´ on one side of IR and site 1´ and site 2 on the opposite side. The current model for IR activation is that two distinct surfaces of insulin engage sequentially with either the site 1/site 2´ binding pocket or the site 1´/site 2 pocket. The formation of a site 1 – insulin - site 2 high-affinity, cross-link involves structural changes in both insulin and IR resulting in the activation of the intracellular tyrosine kinase and the initiation of the phosphorylation cascades that drive insulin signaling. Understanding how insulin binding induces signal transduction requires structures of: (i) insulin and IR in their basal states, (ii) insulin bound to the IR ectodomain, (iii) the activated IR kinase domain and (iv) the domain rearrangements associated with the formation of the high affinity insulin/IR complex that initiates activation of the intracellular kinase. Continue reading >>
What is the difference between type 1 and type 2 diabetes?
In type 1 diabetes, the body's immune system destroys the cells that release insulin, eventually eliminating insulin production altogether from the body. Without insulin, cells cannot absorb sugar (glucose), which they need to produce energy. Type 2 diabetes (formerly called mature-onset or non�insulin-dependent diabetes) can develop at any age, but most commonly becomes apparent during adulthood. However, the incidence of type 2 diabetes in children is rising. Type 2 diabetes accounts for the vast majority of people with diabetes�more than 90%. In contrast to type 1 diabetes, type 2 diabetes is characterized by insulin resistance. Insulin resistance refers to the inability of the body tissues to respond properly to insulin. Insulin resistance develops because of multiple factors, including genetics, obesity, increasing age, and having high blood sugar over long periods of time. How are these diseases different? Type 1 diabetes Type 2 diabetes Symptoms usually start in childhood or young adulthood. People often seek medical help because they are seriously ill from sudden symptoms of high blood sugar. May not have symptoms before diagnosis. Usually the disease is discovered in adulthood; however, there is an increasing number of children being diagnosed with the disease. Episodes of low blood sugar level (hypoglycemia) common No episodes of low blood sugar level, unless taking insulin or certain oral diabetes medic Continue reading >>
What is the insulin receptor?
The insulin receptor is a tetramer that is stabilized by internal disulfide bonds. Upon binding insulin to the external domain, the internal tyrosine kinase domain phosphorylates tyrosine residues on insulin receptor substrate 1 (IRS-1) to transduce the insulin signal by two pathways (Fig. 5-10 ): 1. IRS-1 converts phosphatidylinositol in the ...
Where are insulin receptors located?
Insulin receptors (comprising 2 α and 2 β subunits) are present on the surface of target cells such as liver, muscle and fat. Insulin binding results in tyrosine autophosphorylation of the β subunit. This then phosphorylates other substrates so that a signalling cascade is initiated and biological responses ensue. Downstream effects of stimulation of the insulin receptor include both immediate/short-term actions (for example translocation of the glucose transporter GLUT4 to the surface of target cell) and longer-term actions (for example increased expression of glucokinase and reduced expression of gluconeogenic and ketogenic enzymes in the liver).
What is the standard insulin response?
The stimulation of glucose uptake into selected target cells is the historical standard insulin response. Glucose influx into skeletal muscle, adipose, and cardiac muscle is stimulated by insulin binding to its receptor. When insulin binds to its receptor, it can result in the activation of pathway P4 (see Figure 6-6B ). Thus, the six member signaling pathway starting with CAP and ending with TCIO stimulates translocation of glucose transporter #4 (GLUT4) which is stored in intracellular membranous vesicles in the cell’s cytosol to the cell’s plasma membrane via an exocytosis process. The final outcome on completion of the exocytosis of the GLUT4 is its functioning as a sodium-independent, facilitated-diffusion glucose transporter which stimulates the uptake of extracellular glucose and delivers it into the cytosol of the host cell. The principal participant in this pathway is GLUT4, which is one of 12 sugar transporter proteins; see Table 6-7. The GLUTs are divided into three classes. CLASS I members are GLUTs 1–4 and each one is a glucose transporter. Class II GLUTs are fructose transporters and Class III GLUTs are structurally atypical members of the GLUT family and their functions are not yet well described.
What are postbinding defects in insulin action?
In patients with T2DM and overt fasting hyperglycemia, a number of postbinding defects have been demonstrated, including reduced IR tyrosine kinase activity, insulin signal transduction abnormalities, decreased glucose transport, diminished glucose phosphorylation, and impaired GS activity. The glycolytic/glucose oxidative pathway is largely intact and, when defects are observed, they appear to be acquired secondary to enhanced FFA/lipid oxidation. From the quantitative standpoint, impaired glycogen synthesis represents the major pathway responsible for the insulin resistance in T2DM and is present long before the onset of overt diabetes, that is, in normal glucose-tolerant, insulin-resistant prediabetic subjects and in individuals with IGT. The impairment in GS activation appears to result from a defect in the ability of insulin to phosphorylate IRS-1, causing a reduced association of the p85 subunit of PI3K with IRS-1 and decreased activation of the enzyme PI3K.
How does insulin imprinting affect phagocytosis?
Insulin imprinting enhances the insulin binding of the cells. Twenty-four hours after insulin imprinting, phagocytosis increased in relation to non-imprinted controls.72 Histamine did not influence the process. Insulin bound to cytodex spheres had a repellent effect on Tetrahymena in the first encounter, while in the second encounter, an attracting effect was observed. Cell movement was deeply influenced by insulin imprinting. 73 Slow movement was increased in imprinted cells, and re-exposure to insulin had a similar, but even stronger, effect.
What is the only insulin-responsive glucose transporter?
GLUT-4 is the only insulin-responsive glucose transporter, and for this reason has been studied extensively. Insulin mobilizes GLUT-4 to the membrane, thereby facilitating glucose transport into the cell. Glucose transport activity was studied in the erythrocytes of trained and untrained racehorses (Arai et al., 1994 ).
What is the role of insulin binding in the cytoplasm?
Insulin binding also activates receptors both on the plasma membrane surface and in the cytoplasm. This activation induces a variety of reactions—for example, phosphorylations—but the details and their implications are not yet known.
How are insulin receptors synthesized?
The receptors are synthesized as single chain preproreceptors that are processed by a furin-like proteolytic enzyme, glycosylated, folded and dimerized to yield the mature a2b2receptor. In cells expressing both insulin and IGF-I receptors, hybrid receptors are formed consisting of one half of each (31).
Where is the insulin receptor located?
Insulin is an anabolic peptide hormone secreted by the b cells of the pancreas acting through a receptor located in the membrane of target cells - major ones being liver (where it promotes glucose storage into glycogen and decreases glucose output), ...
How many exons are in the insulin receptor?
The insulin receptor has a modular structure (for review see ref. 25) encoded by a gene (located on chromosome 19) with 22 exons and 21 introns (26, Fig. 3). The short exon 11 that encodes a 12-amino acid sequence is alternatively spliced, resulting in two receptor isoforms (A and B) that differ slightly in affinity for insulin (27-29). The B isoform binds the IGFs with at least 100 times lower affinity than insulin, while the A isoform has significantly higher affinity than the B isoform for IGF-I and especially IGF-II (30) and may play a role in tumorigenesis. The IGF-I receptor binds IGF-II with a lower affinity than IGF-I and insulin with a 500-fold lower affinity. The receptors are synthesized as single chain preproreceptors that are processed by a furin-like proteolytic enzyme, glycosylated, folded and dimerized to yield the mature a 2 b 2 receptor. In cells expressing both insulin and IGF-I receptors, hybrid receptors are formed consisting of one half of each (31). Their physiological role is unknown. Comparative sequence analysis of the insulin/IGF-I receptors and the related EGF receptor (32) had led Bajaj et al. to suggest (Fig. 3) that the N-terminal half consists of two large homologous globular domains, L1 and L2, separated by a cysteine-rich region later predicted to consist of a series of disulfide-linked modules similar to those found in the tumor-necrosis factor (TNF) receptor and laminin. The C-terminal half of the receptors was predicted to consist of three fibronectin type III (FnIII) domains. The second FnIII domain contains a large insert domain (120 residues) of unknown structure containing the site of cleavage between a- and b-subunits. The disulfide bond between each a- and b- subunit involves the cysteins C647 and C860. In addition there are a-a disulfide bonds at C524 in the FnIII-1 domains and between the triplet C682-C683 and C685 in the insert domain (Fig. 3). The intracellular portion of the a-subunit contains the kinase domain flanked by two regulatory regions, a juxtamembrane region involved in docking insulin receptor substrates (IRS) 1-4 and Shc as well as in receptor internalization, and a C-terminal tail. The IGF-I receptor has a similar modular organization (33). The recent progress in the X-ray crystallographic structures of whole ectodomains or fragments of the insulin and IGF-I receptors (see below) has largely validated the structural predictions shown in Fig. 3.
What do the circles on the insulin receptors represent?
The circles marked S1 and S2 symbolize the two insulin receptor binding sites , in a symmetrical antiparallel disposition. The insulin molecule is symbolized by a black dot. a1 and a2: association rate constants for sites 1 and 2 respectively. d1 and d2: dissociation rate constants for sites 1 and 2 respectively. kcr: crosslinking constant. see text for explanations. From reference 64, used with permission.
How does insulin work?
The concept that insulin acts by promoting glucose transport across the membrane of target cells (rather than acting directly on enzymes of intermediary metabolism of glucose) was established in 1949 by the iconic experiment of Rachmiel Levine and colleagues (8), who showed that insulin markedly increased the volume of distribution of non-metabolisable galactose in eviscerated nephrectomized dogs from 45-47% of body weight to 75%, a figure close to that of total body water. From this finding they proposed the following working hypothesis: "Insulin acts upon the cell membrane of certain tissues (skeletal muscle, etc.) in such a manner that the transfer of hexoses (and perhaps other substances) from the extracellular fluid into the cell is facilitated. The intracellular fate of the hexoses depends upon the availability of metabolic systems for their transformation. In the case of glucose, dissimilation, glycogen storage, and transformation to fat are secondarily stimulated by the rapidity of its entry into the cell".
What are the pleiotropic actions of insulin?
Insulin through its receptor affects multiple physiological processes in the organism (left) by increasing (green arrows) or decreasing (red arrows) various intracellular metabolic pathways (right). Inspired by figure 2-1 of reference 1.
Where is insulin secreted?
ABSTRACT. Insulin is an anabolic peptide hormone secreted by the b cells of the pancreas acting through a receptor located in the membrane of target cells - major ones being liver (where it promotes glucose storage into glycogen and decreases glucose output), as well as skeletal muscle and fat ...
What is the insulin receptor?
The insulin receptor is a member of the ligand-activated receptor and tyrosine kinase family of transmembrane signaling proteins that collectively are fundamentally important regulators of cell differentiation, growth, and metabolism. The insulin receptor has a number of unique physiological and bio ….
What is the initial response to the ligand?
The initial response to the ligand is receptor autophosphorylation for all receptor tyrosine kinases. In most cases, this results in receptor association of effector molecules that have unique recognition domains for phosphotyrosine residues and whose binding to these results in a biological response. For the insulin receptor, this does not occur;
Does insulin phosphorylate substrate proteins?
For the insulin receptor, this does not occur; rather, it phosphorylates a large substrate protein that, in turn, engages effector molecules. Possible reasons for these differences are discussed in this review.
How does the cellular receptor for insulin work?
The cellular receptor for insulin helps control the utilization of glucose by cells Cells throughout the body are fueled largely by glucose that is delivered through the bloodstream . A complex signaling system is used to control the process, ensuring that glucose is delivered when needed and stored when there is a surplus. Two hormones, insulin and glucagon, are at the center of this signaling system. When blood glucose levels drop, alpha cells in the pancreas release glucagon, which then stimulates liver cells to release glucose into the circulation. When blood glucose levels rise, on the other hand, beta cells in the pancreas release insulin, which promotes uptake of glucose for metabolism and storage. Both hormones are small proteins that are recognized by receptors on the surface of cells. Signal Transduction The receptor for insulin is a large protein that binds to insulin and passes its message into the cell. It has several functional parts. Two copies of the protein chains come together on the outside of the cell to form the receptor site that binds to insulin. This is connected through the membrane to two tyrosine kinases, shown here at the bottom. When insulin is not present, they are held in a constrained position, but when insulin binds, these constraints are released. They first phosphorylate and activate each other, and then phosphorylate other proteins in the signaling network inside the cell. Since the whole receptor is so flexible, researchers have determined its structure in several pieces: the insulin-binding portion is shown here from PDB entry 3loh , the transmembrane segment from 2mfr , and the tyrosine kinase from 1irk . When Things Go Wrong Problems with insulin signaling can impair the proper management of glucose levels in the blood, leading to Continue reading >>
Where are the insulin receptors located?
Insulin Receptors are areas on the outer part of a cell that allow the cell to join or bind with insulin that is in the blood. When the cell and insulin bind together, the cell can take glucose (sugar) from the blood and use it for energy. Phe 25B is the active site of insulin. Insulin makes contact with the insulin receptor in a hydrophobic pocket. This causes the C-terminus of the B chain to separate from the N-terminus of the A chain. This allows for more binding and reactions to occur. Although insulin stimulates a vast array of responses in its target tissues skeletal muscle, adipose tissue and the liver, they all appear to be initiated by an interaction between insulin and a protein receptor located on the cell membranes of these tissues. The insulin receptor protein can only be found on these tissues, which explains the specificity of the action. When insulin binds it induces a conformational change within the receptor, known as oligomerization, which leads to autophosphorylation of specific tyrosine residues in the cytoplasmic domains of the receptors. Insulin Receptor To view the insulin receptor in cartoon form Continue reading >>
How Does Insulin Signal A Cell To Take In Glucose From The Blood?
Insulin is a hormone released by our pancreas that signals cells in a specific way in order to stimulate them to take in, use and store glucose. Function of Insulin After ingesting food, your meal is broken down and digested. As a result, glucose is released into your bloodstream. High concentrations of glucose in the blood are a signal for the beta cells of the pancreas to release insulin. This hormone works like a key to unlock the protective cell membranes and allow the passage of glucose into the cell to be used for energy. Mechanism of Insulin Insulin works to decrease the concentration of glucose in the blood and facilitate transport into the cells by binding to special receptors embedded in their membranes. Although there are some tissues such as the brain and the liver that do not require insulin for glucose uptake, most of our cells would not be able to access blood glucose without it. Glucose is the energy source for all cells and is required for their, and ultimately our, survival. The insulin signaling pathway includes an insulin receptor that is made up of two receptor subunits that are located on the outside of the cell membrane and two subunits that penetrate through the membrane. These subunits are chemically bonded together. The extracellular (outside the cell) subunits contain a binding site for insulin. When insulin binds to the extracellular subunits, it activates a chemical reaction that travels through the linked subunits into the cell. This mechanism sends chemical signals to proteins within the cell and causes them to alter their Continue reading >>
What is type 2 diabetes?
According to the medical literature, type 2 diabetes is a disease characterized by chronic hyperglycemia, i.e., abnormally high concentrations of blood sugar (serum glucose), in the presence of adequate amounts of insulin. This hyperglycemia is attributed to insulin resistance, a faulty condition in which serum insulin cannot act on insulin receptors in the walls of cells. This condition prevents the receptors from allowing glucose to pass from the blood into the cells. According to the biochemical literature, an insulin receptor is a protein molecule located in the wall of a cell. The structure of the molecule is such that a smaller molecule called a ligand may attach to it. There are two kinds of ligands: an agonist, which causes the receptor to function, and an antagonist, which does nothing but prevent the agonist from attaching to the receptor. Without an attached ligand, an insulin receptor cannot allow glucose molecules to pass from the blood into a cell. An insulin molecule is an agonist, and when one becomes a ligand, an insulin receptor can allow glucose molecules to pass into a cell. But the hormone cortisol is an insulin antagonist, and when a cortisol molecule becomes a ligand, it prevents an insulin molecule from becoming a ligand, which prevents glucose from passing from the blood into the cell involved. I believe that the action of cortisol as an insulin antagonist is a reasonable explanation of the condition that we call insulin resistance, in which case there is nothing wrong with the insulin receptors or the insulin. Insulin resistance, then, would be part of the natural functioning of an insulin receptor. There are reasons to believe that the brain is responsible for the production of excess cortisol for the purpose of preventing the loss of serum gl Continue reading >>
What is the difference between type 1 and type 2 diabetes?
In type 1 diabetes, the body's immune system destroys the cells that release insulin, eventually eliminating insulin production altogether from the body. Without insulin, cells cannot absorb sugar (glucose), which they need to produce energy. Type 2 diabetes (formerly called mature-onset or non�insulin-dependent diabetes) can develop at any age, but most commonly becomes apparent during adulthood. However, the incidence of type 2 diabetes in children is rising. Type 2 diabetes accounts for the vast majority of people with diabetes�more than 90%. In contrast to type 1 diabetes, type 2 diabetes is characterized by insulin resistance. Insulin resistance refers to the inability of the body tissues to respond properly to insulin. Insulin resistance develops because of multiple factors, including genetics, obesity, increasing age, and having high blood sugar over long periods of time. How are these diseases different? Type 1 diabetes Type 2 diabetes Symptoms usually start in childhood or young adulthood. People often seek medical help because they are seriously ill from sudden symptoms of high blood sugar. May not have symptoms before diagnosis. Usually the disease is discovered in adulthood; however, there is an increasing number of children being diagnosed with the disease. Episodes of low blood sugar level (hypoglycemia) common No episodes of low blood sugar level, unless taking insulin or certain oral diabetes medic Continue reading >>
Where is insulin secreted?
INTRODUCTION Insulin is a peptide hormone composed of 51 amino acids that is synthesized, packaged, and secreted in pancreatic beta cells. The mechanisms of insulin secretion and measurements of beta cell function in normal subjects and patients with various diseases will be reviewed here. The function of the insulin receptor after binding insulin and the mechanisms of insulin action are discussed separately. (See "Structure and function of the insulin receptor" and "Insulin action".) ANATOMY Pancreatic beta cell s are found in the islets of Langerhans, which are of various size and contain a few hundred to a few thousand endocrine cells. Islets are anatomically and functionally separate from pancreatic exocrine tissue (which secretes pancreatic enzymes and fluid directly into ducts that drain into the duodenum). Normal subjects have approximately one million islets that, in total, weigh 1 to 2 grams and constitute 1 to 2 percent of the mass of the pancreas. Islets vary in size from 50 to 300 micrometers in diameter. They are composed of several types of cells. At least 70 percent are beta cells, which are localized in the core of the islet. These cells are surrounded by alpha cells that secrete glucagon, smaller numbers of delta cells that secrete somatostatin, and PP cells that secrete pancreatic polypeptide (figure 1). All of the cells communicate with each other through extracellular spaces and through gap junctions. This arrangement allows cellular products secreted from one cell type to influence the function of downstream cells. As an example, insulin secreted from beta cells suppresses glucagon secreted from alpha cells. A neurovascular bundle containing arterioles and sympathetic and parasympathetic nerves enters each islet through the central core of beta cells Continue reading >>
Does insulin have anything to do with blood sugar?
Stand on a streetcorner and ask people if they know what insulin is, and many will reply, "Doesn't it have something to do with blood sugar?" Indeed, that is correct, but such a response is a bit like saying "Mozart? Wasn't he some kind of a musician?" Insulin is a key player in the control of intermediary metabolism, and the big picture is that it organizes the use of fuels for either storage or oxidation. Through these activities, insulin has profound effects on both carbohydrate and lipid metabolism, and significant influences on protein and mineral metabolism. Consequently, derangements in insulin signalling have widespread and devastating effects on many organs and tissues. The Insulin Receptor and Mechanism of Action Like the receptors for other protein hormones, the receptor for insulin is embedded in the plasma membrane. The insulin receptor is composed of two alpha subunits and two beta subunits linked by disulfide bonds. The alpha chains are entirely extracellular and house insulin binding domains, while the linked beta chains penetrate through the plasma membrane. The insulin receptor is a tyrosine kinase. In other words, it functions as an enzyme that transfers phosphate groups from ATP to tyrosine residues on intracellular target proteins. Binding of insulin to the alpha subunits causes the beta subunits to phosphorylate themselves (autophosphorylation), thus activating the catalytic activity of the receptor. The activated receptor then phosphorylates a number of intracellular proteins, which in turn alters their activity, thereby generating a biological response. Several intracellular proteins have been identified as phosphorylation substrates for the insulin receptor, the best-studied of which is insulin receptor substrate 1 or IRS-1. When IRS-1 is activa Continue reading >>
How does insulin affect gene expression?
Insulin Receptor and Gene Expression. Apr. 4, 2019 — Insulin triggers genome-wide changes in gene expression via an unexpected mechanism. The insulin receptor is transported from the cell surface to the cell nucleus, where it helps initiate the ...
What is the role of insulin in cellular metabolism?
advertisement. Insulin exerts multiple effects on cellular metabolism and growth. The biological actions of insulin are mediated by a cell-surface receptor, called insulin receptor, which is present on the surface, i.e. the plasma membrane, of virtually all mammalian cells.
What is the role of insulin in signaling cascades?
Insulin binds outside the cell to the extracellular domain of its receptor and induces a structural change that is propagated across the membrane to the intracellular kinase domains inside the cell, causing them to activate each other, thus initiating signaling cascades.
Where is insulin mediated?
In a new study, researchers based in Germany, Canada, and Finland show ...
What is the function of G-protein-coupled receptors in blood glucose control?
Blood glucose control depends heavily on proteins called G-protein-coupled receptors (GPCRs). GPCRs span cell membranes to relay signals from the outside in. Once activated by the binding of a substance, GPCRs trigger a cascade of responses inside the cell. These receptors are thus important targets for drug development.
What are the glucagon receptors?
The glucagon and GLP-1 receptors are both important drug targets for type 2 diabetes and obesity. These results may help inform the design of new drugs to regulate blood glucose levels. —by Harrison Wein, Ph.D. References: Structure of the full-length glucagon class B G-protein-coupled receptor.
What hormone is released when blood glucose levels drop?
When blood glucose levels drop, such as after an overnight fast, the pancreas releases a hormone called glucagon. Glucagon binds a GPCR on liver and muscle cells called the glucagon receptor, which then stimulates the cells to release glucose into the bloodstream. Another hormone involved in glucose control is called glucagon -like peptide-1 (GLP-1).
What is the best medication to control blood glucose?
Medications such as insulin (which lowers blood glucose) and glucagon (which elevates it in an emergency) can help maintain blood glucose in a safe range. However, glucagon in particular can be difficult to administer. Blood glucose control depends heavily on proteins called G-protein-coupled receptors (GPCRs).
How does GLP-1 work?
It works by binding to another GPCR, the GLP-1 receptor, on cells in the pancreas. After a meal, the intestine produces GLP-1, which prompts the pancreas to produce insulin. Insulin, in turn, stimulates cells to take in glucose from the blood. The glucagon and GLP-1 receptors are both class B GPCRs. The structures of several class A GPCRs have been ...
Why are class B receptors not well studied?
The structures of several class A GPCRs have been solved, but class B receptors haven’t been as well studied because of technical challenges. Four international research teams reported the structures of the glucagon and GLP-1 receptors in Nature on June 8, 2017.
Who is the scientist who discovered the structure of the human glucagon receptor?
In one of the new papers, an international team led by Dr. Beili Wu from the Shanghai Institute of Materia Medica, Chinese Academy of Sciences, described the structure of the full length human glucagon receptor.