How does lipid emulsion therapy work? Lipid emulsion therapy is an intravenous therapy that binds lipophilic toxins and therefore reverses their toxicity. There are several brand name lipid emulsion therapies, however Intralipid
Lipid emulsion
Lipid emulsion or fat emulsion refers to an emulsion of lipid for human intravenous use. It is often referred to by the brand name of the most commonly used version, Intralipid, which is an emulsion of soy bean oil, egg phospholipids and glycerin, and is available in 10%, 20% and 30% c…
What is intravenous lipid emulsion (Ile) therapy?
Intravenous lipid emulsion (ILE) therapy (also known as lipid resuscitation therapy, LRT) is the current recommended treatment for local anesthetic systemic toxicity (LAST) by professional societies such as the American Society of Regional Anesthesia (ASRA).[1]
Can lipid emulsion be used to treat last syndrome?
For this reason and the fact that local anesthetic toxicity is rare, by the time this syndrome is identified, patients are often in cardiac arrest or peri-arrest. Thankfully, lipid emulsion such as Intralipid is a safe and effective therapy used to treat LAST. How does lipid emulsion therapy work?
What is the role of lipid emulsions in the treatment of cardiotoxicity?
Lipid emulsions are effective in treating experimental models of severe cardiotoxicity from intravenous overdose of local anaesthetic drugs such as bupivacaine.
What are lipid emulsions made of?
Lipid emulsions are iso-osmolar and contain a core made essentially of triglycerides stabilized by a layer of phospholipids. Phospholipids serve as an emulsifying agent; glycerol is used to make the emulsion isotonic. Fat emulsions are available in concentrations of 10%, 20%, and 30%.

What does lipid emulsion do?
INTRAVENOUS LIPID EMULSION is a source of fat. It is used to provide calories and necessary fatty acids when unable to get nutrition with a regular diet. This medicine may be used for other purposes; ask your health care provider or pharmacist if you have questions.
What is lipid emulsion therapy?
Lipid emulsion therapy is a medication used in the management and treatment of Local anesthetic toxicity. This activity reviews the indications, action, and contraindications for lipid emulsion therapy as a valuable agent in the management of local anesthetic toxicity.
How does lipid emulsion treat Lidocaine toxicity?
Lipid emulsion therapy such as Intralipid mitigates the toxic effects of local anesthetics and can reverse both neurologic and cardiac toxicity. LAST may manifest initially with CNS symptoms but can progress to seizure, respiratory depression, coma, and cardiovascular collapse.
What does lipid rescue do?
LipidRescue™ resuscitation refers to the intravascular infusion of 20% lipid emulsion to treat severe, systemic drug toxicity or poisoning.
What is lipid emulsion made of?
Commercial lipid emulsions in the United States are usually based on soybean oil or soybean and safflower oil. They also include egg yolk phospholipids, glycerin, and water. The presence of soybean and safflower oil means that these solutions are composed primarily of n-6 fatty acids.
Does intralipid cause weight gain?
Tell your doctor right away if any of these unlikely but serious side effects occur: signs of infection (such as sore throat that doesn't go away, fever), pain/swelling/redness at injection site, pain/swelling/redness of arms/legs, bluish skin, sudden weight gain, shortness of breath, back/chest pain.
What happens if you infuse lipids too fast?
Accidental lipid overdose due to an excessive infusion rate of ILE may result in serious complications, such as respiratory failure, metabolic acidosis and even death.
What happens if lidocaine enters the bloodstream?
If a substantial amount is ingested, enough can be absorbed into the bloodstream to affect vital organs, primarily the brain and heart. Symptoms can range from mild drowsiness and headache to confusion, seizures, coma, and cardiac arrest.
How do you get rid of lidocaine toxicity?
Patients with suspected lidocaine overdoses are treated with modified protocols, such as reducing epinephrine doses of less than 1 microgram per kilogram.
How long does intralipid infusion last?
In 47 patients, the suppressive effect of the Intralipid after the normalization of NKa lasted between 6 and 9 weeks; in two patients, this benefit lasted 5 weeks; and in one patient, the effect lasted 4 weeks.
How much does intralipid cost?
Intralipid Cost Intralipids (approximately $100 per administration) are far less expensive than Intravenous Immunoglobulin (IVIG) (approximately $2000 per administration), and initial studies show comparable efficacy for deactivation of natural killer cells and pregnancy rates.
How fast can you infuse lipids?
In acutely ill patients, lipid infusion should be administered over at least 12 hours/day. With a more critical metabolic situation, slower infusion rates such as continuous infusion over approximately 24 hours are recommended.
What are the side effects of lipids?
The most common statin side effects include:Headache.Difficulty sleeping.Flushing of the skin.Muscle aches, tenderness, or weakness (myalgia)Drowsiness.Dizziness.Nausea or vomiting.Abdominal cramping or pain.More items...•
What does an intralipid infusion do?
Intralipid is used for improving implantation in patients with high natural killer cell activity. Intralipid or lipid emulsion, is an intravenous infusion that aims to provide essential fatty acids that are necessary for women who have suffered repeat miscarriages.
What is the primary component of lipid therapy?
The oil component consists of neutral long-chain triglycerides or a mixture of medium- and long-chain triglycerides.
What are the symptoms of fat overload syndrome?
Fat overload syndrome is a well-known complication of intravenous lipid emulsion therapy. It is characterized by headaches, fever, jaundice, hepatosplenomegaly, respiratory distress, and spontaneous hemorrhage. Other symptoms include anemia, leukopenia, thrombocytopenia, low fibrinogen levels, and coagulopathy.
What is lipid emulsion therapy?
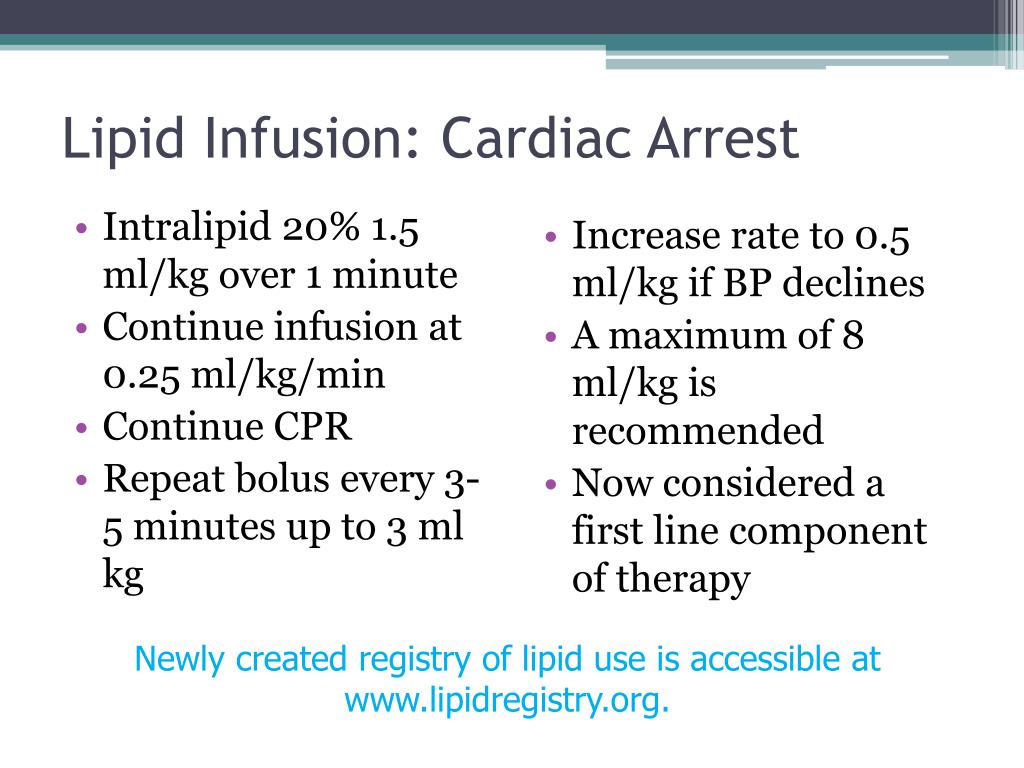
Lipid emulsion therapy is an intravenous therapy that binds lipophilic toxins and therefore reverses their toxicity. There are several brand name lipid emulsion therapies, however Intralipid, a soy-based lipid emulsion that contains long-chain triglycerides, is the most commonly used (Figure 1). [3] The ability of lipid emulsion therapy to counteract the toxic effects of local anesthetics was discovered in 1998 by Weinberg et al when it was incidentally found that lab rats pre-treated with an infusion of lipids could withstand larger doses of bupivacaine before arresting. [4] The rats were also more easily resuscitated if given lipid emulsion therapy. [1] These findings were subsequently confirmed in other laboratories and clinical systemic analyses. [5] Once studied more directly, it was found that intralipid acts as a “sink” by creating a lipid compartment within the plasma that attracts lipophilic compounds, such as local anesthetics, into the lipid sink, which is separate from the aqueous phase of the plasma. [1]
How long should a lipid emulsion be given?
An initial dose of 20% lipid emulsion at 1.5 ml/kg or a 100 ml bolus can be administered over a few minutes. This can be repeated after 5 minutes for 2 or more times for persistent hemodynamic instability. The bolus (es) should immediately be followed by a continuous infusion at 0.25-0.5 ml/kg/min. [3] The infusion should run for a minimum of 10 minutes after return of hemodynamic stability, however there are documented reports of recurrent systemic toxicity even after this. For this reason, patients should be admitted for at least 12 hours for observation and additional doses of intralipid as needed for rebound symptoms or hemodynamic compromise. [3] Consultation with your facility’s poison center is also crucial to further guide management.
What is intralipid therapy?
Lipid emulsion therapy such as Intralipid mitigates the toxic effects of local anesthetics and can reverse both neurologic and cardiac toxicity. LAST may manifest initially with CNS symptoms but can progress to seizure, respiratory depression, coma, and cardiovascular collapse.
What is intralipid?
Once studied more directly, it was found that intralipid acts as a “sink” by creating a lipid compartment within the plasma that attracts lipophilic compounds, such as local anesthetics, into the lipid sink, which is separate from the aqueous phase of the plasma. [1]
When was lipid emulsion therapy discovered?
The ability of lipid emulsion therapy to counteract the toxic effects of local anesthetics was discovered in 1998 by Weinberg et al when it was incidentally found that lab rats pre-treated with an infusion of lipids could withstand larger doses of bupivacaine before arresting. [4] .
What are the symptoms of EM?
Hematologic – methemoglobinemia, cyanosis. Allergic – urticaria, rash, and rarely anaphylaxis. Local tissue response – numbness, paresthesia. The EM physician should maintain a high level of suspicion should a patient present after a same day surgery or procedure with any constellation of these symptoms.
Is lipid emulsion therapy contraindicated?
There are no absolute contraindications to intravenous lipid emulsion therapy and no clinically significant complications documented in the literature. The benefits of lipid emulsion therapy will often outweigh any potential risks in patients with LAST, especially if hemodynamically unstable or coding.
What is lipid emulsion?
Currently marketed intravenous lipid emulsions in the United States are made of long-chain triglycerides (LCT). Lipids usually provide 30% to 50% of the non-nitrogen caloric needs or about 20% to 30% of total calories. Typically, lipid emulsions in infants and children are initiated at a dose of 1 g/kg/day and advanced by 1 g/kg/day to a maximum ...
How do lipid emulsions improve the bioavailability of a drug?
Lipid emulsions are one of them, which can improve the bioavailability of the drug by increasing the corneal permeability and/or by enhancing the retention time of the formulation in the ocular surface.
What are the roles of liposomes in lipid metabolism?
These liposomes play a significant role in abnormalities of lipid metabolism. They acquire cholesterol and apolipoproteins from HDL in exchange for phospholipids resulting in a reduction in measured HDL levels ( Ferezou and Bach, 1999 ). Additionally, the capacity of HDL to uptake phospholipid is saturable, leading to an accumulation of liposomes in plasma with excessive infusion rates ( Breckenridge, 1985; Ferezou and Bach, 1999 ). The plasma liposomes, if not metabolized by lipoprotein lipase (LPL) and hepatic lipase (HL), continue to become enriched in cholesterol until reaching a 2:1 ratio of phospholipids to cholesterol. At this point they exhibit characteristics of lipoprotein-X (LP-X) and over time lead to hypercholesterolemia ( Miyahara et al., 1979 ). The levels of LP-X are also dependent on the proportion of phospholipid to TG in the infusion. Tashiro et al. (1992) demonstrated that 10% emulsion is associated with higher levels of LP-X compared to 20% emulsions as 10% (Intralipid) emulsion has greater quantity of free liposomes and are smaller in diameter ( Garcia-de-Lorenzo et al., 2003 ). The circulating free liposomes also inhibit the action of LPL and HL on artificial chylomicrons, resulting in poor hydrolysis of TGs causing hypertriglyceridemia ( Lutz et al., 1990 ).
What is ILE in oil?
Intravenous lipid emulsion (ILE), particularly soybean oil (SO) based ILE, can be associated with changes in lipid profile including a decrease in high-density lipoprotein (HDL) and increase in low-density lipoprotein (LDL) and triglyceride (TG) levels (Meguid et al., 1989; Mundi, Salonen and Bonnes, 2016 ). ILEs are typically comprised of TGs derived from an oil source such as SO, olive oil (OO), fish oil (FO), medium chain triglyceride (MCT), or a combination of various oils. A phospholipid emulsifier derived from egg yolk serves to envelop the TG core and allows it to remain soluble in the aqueous PN mixture as a chylomicron-like particle ( Fig. 9.2) ( Ferezou and Bach, 1999; Vinnars and Hammarqvist, 2004 ). In order to ensure that the mean diameter of the chylomicron-like particles does not exceed 500 nm, excess emulsifier is added ( Ferezou and Bach, 1999 ). The excess emulsifier exists in the form of phospholipid-rich particles, which are essentially unilamellar liposomes (bilayer of phospholipid trapping trace lipid and aqueous phase).
What is ILE therapy?
ILE therapy uses intravenous administration of a 20% lipid emulsion as a polyvalent antidote to poisoning by lipophilic drugs. The emulsion, originally developed for parenteral nutrition, may act as a “sink” within the plasma for lipophilic drugs.
Why are lipid emulsions better than 10%?
The 20% lipid emulsion is favored rather than the 10% emulsion because of its better clearance as a result of its lower phospholipid content. 131,132 Because lipid emulsions are derived from vegetable oils, they are also a natural source of variable amounts of vitamin K 133 and vitamin E isomers. 134,135
Why are fat emulsions used?
Theoretically, fat emulsions are employed to prevent essential fatty acid deficiency. In reality, this condition is rare, takes several weeks to develop, and requires only 3%–4% of kilocalories as linoleic acid (or 10% of kilocalories as a standard fat emulsion). Fat emulsions are also used to provide additional kilocalories once glucose delivery exceeds 5 kcal/kg per minute. When delivered in total-nutrient-admixtures (3-in-1 solutions) lipid emulsions are stable for 24 hours. When infused as a sole nutrient, limit hang times to <12 hours to prevent bacterial growth. Avoid fat emulsions with hyperlipidemia-induced pancreatitis and when serum triglycerides are significantly elevated (e.g., >500 mg/dL). Because they are associated with increased mortality early after trauma, and increased infections in critical illness, IV fat emulsion risk outweighs benefit during the early acute-phase response.
How much energy is in lipid emulsion?
Intravenous lipid emulsions are a condensed source of energy and essential fatty acids, providing 9 kcal/g of energy. The caloric value of lipid emulsions varies with the lipid emulsion concentration. Lipid emulsions at 10%, 20%, and 30% concentrations yield 1.1 kcal/mL, 2 kcal/mL, and 3 kcal/mL, respectively. Currently marketed intravenous lipid emulsions in the United States are made of long-chain triglycerides (LCT). Lipids usually provide 30% to 50% of the non-nitrogen caloric needs or about 20% to 30% of total calories. Typically, lipid emulsions in infants and children are initiated at a dose of 1 g/kg/day and advanced by 1 g/kg/day to a maximum of 3 g/kg/day. Gradually increasing the daily lipid intake (0.5 or 1 g/kg/day) does not seem to improve lipid clearance. However, the lipid emulsion is cleared better 128,129 and lipid utilization is improved 130 when lipid is infused continuously over 24 hours rather than intermittently or for part of the day. Keeping the intravenous lipid infusion rate below 0.12 g/kg/hour improves lipid clearance.
Why are fat emulsions used?
Theoretically, fat emulsions are employed to prevent essential fatty acid deficiency. In reality, this condition is rare, takes several weeks to develop, and requires only 3%–4% of kilocalories as linoleic acid (or 10% of kilocalories as a standard fat emulsion). Fat emulsions are also used to provide additional kilocalories once glucose delivery exceeds 5 kcal/kg per minute. When delivered in total-nutrient-admixtures (3-in-1 solutions) lipid emulsions are stable for 24 hours. When infused as a sole nutrient, limit hang times to <12 hours to prevent bacterial growth. Avoid fat emulsions with hyperlipidemia-induced pancreatitis and when serum triglycerides are significantly elevated (e.g., >500 mg/dL). Because they are associated with increased mortality early after trauma, and increased infections in critical illness, IV fat emulsion risk outweighs benefit during the early acute-phase response.
What are fat emulsions?
Fat emulsions were once considered to be primarily a high-density source of energy in parenteral nutrition, but attention is now being increasingly focussed on fat emulsions as a source of important biological precursors with wider effects. These may become particularly important in long-term therapy, such as parenteral nutrition at home. Clinoleic® (Baxter–Clintec, Maurepas, France) is prepared from a mixture of soy bean oil 20% and olive oil 80%. Compared with other fat emulsions on the market, it contains 60% monounsaturated fatty acids, around 20% less polyunsaturated fatty acids, and no medium-chain triglycerides. In a non-randomized observational study in 14 patients (median age 50, range 35–79, years; 8 men) receiving long-term parenteral nutrition at home the new emulsion produced significantly lower plasma α-linolenic acid concentrations, but did not affect overall essential fatty acid status (11c). There were no adverse effects. In particular, some adverse effects that are commonly reported with other lipid emulsions (shivering, nausea, tachycardia, pyrexia, and hypertension) were not reported, although this is difficult to interpret as it was not stated whether any of these patients had had these symptoms during previous administration of other emulsions. However, five patients had reported migraine without aura during previous infusions; of these, three claimed to feel consistently better with the new emulsion at 3 months.
What is the purpose of ILEs?
ILEs serve primarily as a source of energy and EFAs in patients with intestinal failure. However, ILEs are also the foremost source of vitamin E (tocopherol) in PN-dependent patients. Vitamin E is the major lipid-soluble antioxidant and occurs in several isoforms, of which α-tocopherol displays the highest bioactivity in terms of reducing lipid peroxidation ( Xu et al., 2015 ). Considering the tendency for a disturbed (anti)oxidant balance in PN-dependency and the pathogenic effect of lipid peroxidation in the development and/or progression of IFALD, vitamin E deficiency has been suggested as a potential cause for IFALD. The amount and types of vitamin E homologs in commercially available ILEs vary considerably, due to the oil species used to manufacture the emulsions, and also due to the addition of exogenous α-tocopherol, which may be added to ILEs to minimize oxidation of the FAs ( Vanek et al., 2012; Xu et al., 2015 ).
What is ILE therapy?
ILE therapy uses intravenous administration of a 20% lipid emulsion as a polyvalent antidote to poisoning by lipophilic drugs. The emulsion, originally developed for parenteral nutrition, may act as a “sink” within the plasma for lipophilic drugs. In various animal models and human case reports, it appears that the drugs are sequestered within this lipid phase and thus prevented from acting at potential target organs, such as the brain and the heart. Other theoretical mechanisms of action include the provision of free fatty acid fuel to starving cardiac mitochondria and increasing cardiac myocyte calcium influx. A large and growing body of data demonstrates benefit of ILE for several types of cardiotoxic drugs, including sodium channel blockers, calcium channel blockers, and some β-blockers. Consider giving lipid emulsion to any poisoned patient who has ingested a highly lipid-soluble drug and has significant hemodynamic instability.
Does fat emulsion affect fibrinolysis?
Fat emulsions affect coagulation and fibrinolysis [ 63 ]. In 36 patients undergoing aortocoronary bypass operations with anesthesia based on midazolam/fentanyl or propofol/alfentanil, factor XIIa concentrations and kallikrein-like activity were about 30% higher in the propofol group. The authors suggested that there had been stronger activation of the contact phase at the start of recirculation and stronger fibrinolysis in the propofol group. They also found more hypotension in the propofol group, which they assumed to be due to release of kallikrein, resulting in release of bradykinin. Propofol has not been proven to cause increased perioperative bleeding.
What is lipid emulsion?
Lipid emulsion. Lipid emulsion or fat emulsion refers to an emulsion of lipid for human intravenous use. It is often referred to by the brand name of the most commonly used version, Intralipid, which is an emulsion of soy bean oil, egg phospholipids and glycerin, and is available in 10%, 20% and 30% concentrations.
Why is intralipid used in optical experiments?
Intralipid is also widely used in optical experiments to simulate the scattering properties of biological tissues. Solutions of appropriate concentrations of intralipid can be prepared that closely mimic the response of human or animal tissue to light at wavelengths in the red and infrared ranges where tissue is highly scattering but has a rather low absorption coefficient.
How do ROS work?
The generated ROS, which are formed from electrons leaking from the electron transport chain of the mitochondria, first act directly on mPTP to limit opening. ROS then activate signalling pathways that act on the mitochondria to decrease mPTP opening and mediate protection.
When was intralipid first used?
Intralipid was invented by the Swedish physician and nutrition researcher Arvid Wretlind, and was approved for clinical use in Sweden in 1962. In the United States, the Food and Drug Administration initially declined to approve the product due to prior experience with another fat emulsion.
Is propofol a lipid?
Propofol is dissolved in a lipid emulsion for intravenous use. Sometimes etomidate (the vehicle for etomidate is propylene glycol) is supplied using a lipid emulsion as a vehicle.
What is IV lipid emulsion?
IV lipid emulsion therapy originated from anesthesia literature that described its successful use in iatrogenic local anesthetic overdoses. Since then, the drug’s use has expanded to include many other lipophilic xenobiotics that have no antidote, such as calcium channel blockers and antipsychotics.
When should lab tests be drawn for lipid emulsion?
To account for these abnormalities, lab tests should be drawn prior to administration of the lipid emulsion, if possible.
Is lipid emulsion compatible with resuscitation?
While conclusive evidence is lacking, available research suggests that lipid emulsion is not compatible with many of the medications administered during resuscitation efforts. 3
Is IV lipid emulsion an overdose drug?
In emergency medicine pharmacy circles, there is growing awareness of intravenous (IV) lipid emulsion as a potential overdose antidote.