
Is diabetes a deadly disease?
“Diabetes is a deadly disease, but it can oftentimes be taken for granted,” said Dr. Aurora Macaballug, Board Member and Chair of the Advocacy Committee of the Philippine Society of Endocrinology, Diabetes and Metabolism (PSEDM).
Can diabetes insipidus be as dangerous as diabetes mellitus?
There is also the fact that the dangers of diabetes mellitus are much greater than diabetes insipidus. Type I and Type II diabetes can cause severe, immediate symptoms that require immediate treatment. Lifestyle habits can even increase insulin absorption, such as taking a hot shower, which can create its own set of problems after a meal.
Is type one diabetes worse than type two diabetes?
The two types of diabetes have some important differences, but there is no clear answer regarding which one is worse. Type 1 diabetes is an autoimmune disorder. This means that your body attacks itself if you have it. The body’s immune system does not recognize the beta cells in your pancreas and attacks them.
What are the periodontal disease stages?
Periodontal disease occurs in four separate stages, and only the first stage is reversible—the rest will require advanced dental treatments. Stage 1: Gingivitis Gingivitis results from a build-up of plaque around the teeth, causing swelling and redness in the gums, bleeding when brushing or flossing, and occasional bad breath.
What is the relationship between diabetes and periodontal disease?
Overall, the increased risk of periodontitis in patients with diabetes is estimated to be between 2-3 fold – that is, it increases the risk for periodontitis by 2-3 times. Diabetes increases the prevalence of periodontitis, the extent of periodontitis (that is, number of affected teeth) and the severity of the disease.
How does periodontitis affect glycemic control?
In addition, it has been showed that periodontal disease has a devastating effect on glycemic control among type 2 diabetic patients and a significant reduction of Glycated hemoglobin(HA1c), 0.40 %, was observed after 3–4 months of periodontal therapy done on patients with both type 1 and 2 DM and periodontitis [14].
How many people with diabetes are affected by periodontal disease?
Periodontal disease is the most common dental disease affecting those living with diabetes, affecting nearly 22% of those diagnosed.
Can gum infection raise blood sugar?
On the other hand, infections from untreated periodontal disease can cause the blood sugar to rise and make it harder to control diabetes. Another factor, smoking, is harmful to oral health even for people without diabetes.
Can tooth infection affect blood sugar?
An infection such as periodontitis may also cause your blood sugar level to rise, which in turn makes your diabetes more difficult to control. Preventing and treating periodontitis with regular dental cleanings can help improve blood sugar control. Thrush.
Which toothpaste is best for diabetics?
Colgate has worked closely with Diabetes experts and Oral Health experts to develop this special daily-use toothpaste simply called Colgate for Diabetics. The formula is clinically proven and has ayurvedic ingredients like Jamun, Neem, and Amla extracts.
Does metformin cause gum problems?
Medications used by people with diabetes such as Glipizide and Metformin may cause changes to the oral cavity, such as candidiasis, burning mouth, xerostomia, and the chance of getting periodontal disease and caries.
Is chewing gum good for diabetics?
Chewing gum helps to give insulin orally for diabetic patients and tackle the degradation of insulin by digestive enzyme without adding digestive enzyme inhibitor. It can help to reduce the cost of therapy and improve the brain boost power, concentration, and smoking cessation.
Does periodontal treatment improve glycemic control in diabetic patients?
The present meta-analysis suggests that periodontal treatment leads to an improvement of glycemic control in type 2 diabetic patients for at least 3 months.
What do interventional trials on diabetic patients with periodontitis showed?
Results. After the intervention program, the intervention group demonstrated significant improvements in bleeding on probing, which was used to evaluate periodontitis status (F=7.919; P<. 01), and in clinic visit (F=11.765; P<. 01), brushing teeth (F=21.606; P<.
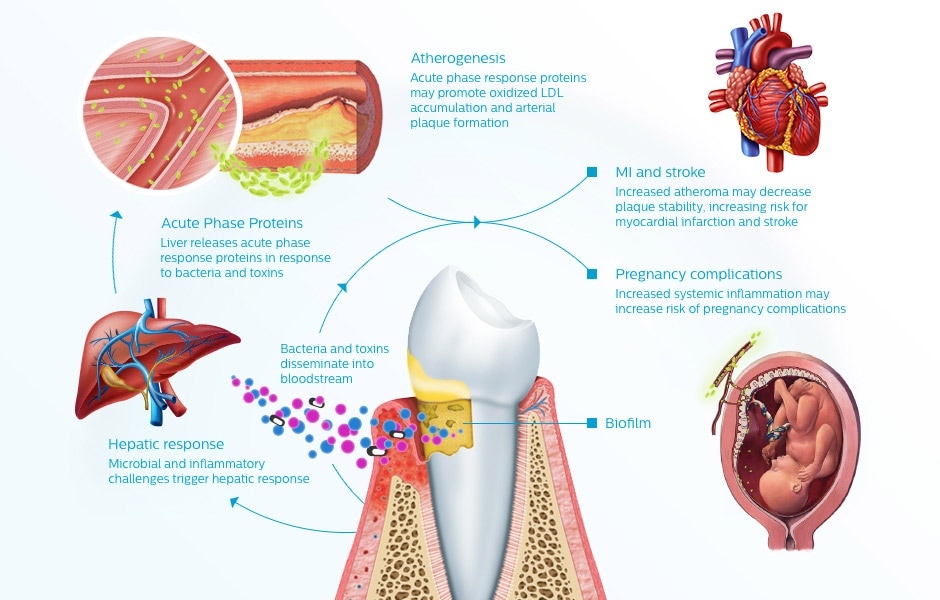
How does periodontal disease affect the cardiovascular system?
You might think the mouth and heart don't have much in common. But increasing evidence suggests they may be closely linked. Researchers suspect that bacteria present in gum disease can travel throughout the body, triggering inflammation in the heart's vessels and infection in heart valves.
How does periodontitis occur?
The tissue destruction that we recognise clinically as periodontitis (ie, breakdown of periodontal ligament, pocketing, and alveolar bone resorption) is primarily caused by the host inflammatory response to the bacterial challenge presented by the biofilm. Treatment of periodontitis involves professional care to reduce the bacterial challenge (oral hygiene instruction and root surface debridement), together with patient education, motivation and empowerment to optimise oral hygiene and reduce or eliminate risk factors such as smoking. Similar to diabetes, the treatment approach for periodontitis requires a life-long strategy that is tailored to the clinical situation, with a focus on behaviour change, patient self-care, and regular professional monitoring and support. Again, similar to diabetes, compliance is a key factor for treatment success.
What are the complications of diabetes?
2 Hyperglycaemia leads to development of the complications associated with diabetes that arise from long-term damage, dysfunction and failure of various organs and body systems that impact on wellbeing and quality of life. Diabetes has significant effects on multiple body systems and organs, including the cardiovascular and circulatory system (cardiovascular disease), the kidneys (nephropathy), the brain and cerebral circulatory system (cerebrovascular disease, stroke, cognitive dysfunction), the lower limbs (peripheral vascular disease, diabetic foot), immune system (increased risk of infections), and eyes (retinopathy). Early symptoms can include thirst, polyuria, blurring of vision and weight loss. A diagnosis of diabetes can be made following a random venous plasma glucose test, a fasting plasma glucose test, a two-hour plasma glucose tolerance test following 75 g oral glucose, or a non-fasting glycated haemoglobin (HbA1c) measurement.
What is the goal of diabetes treatment?
The aim of diabetes treatment is to reduce the risk of microvascular and macrovascular complications by controlling blood glucose, with maintenance of HbA1c below a target value. This is specific to each individual patient, and ideally will be agreed between the person and their diabetes care team as part of their overall diabetes management. In broad terms, HbA1c values <53 mmol/mol (<7.0%) would usually indicate good control. In a non-diabetic person, HbA1c is typically around 37 mmol/mol (5.5%). Reductions in HbA1c are highly relevant, because it has been shown that each 1% reduction in HbA1c (approximately 11 mmol/mol) is associated with measureable reductions in diabetes complications (eg, 21% reduction in diabetes-related deaths, 14% reduction in myocardial infarction, and 37% reduction in microvascular complications of diabetes). 8
What is the cause of Type 1 diabetes?
Type 1 diabetes is believed to result from a combination of genetic predisposition and an environmental trigger (most probably, infection with an enterovirus). Type 1 diabetes tends to develop mainly in childhood, adolescence or in young adults and accounts for 5-10% of all cases of diabetes.
How to treat type 2 diabetes?
Treatment of type 2 diabetes involves weight loss, exercise, diet control, self-monitoring, smoking cessation, oral hypoglycaemic drugs (such as metformin) and, in some cases, insulin injections. The precise treatment strategy is tailored to the clinical situation, with the overall aim being to reduce hyperglycaemia.
What is the difference between type 1 and type 2 diabetes?
Type 1 and type 2 are the principal categories of diabetes. Type 1 diabetes (historically referred to as insulin-dependent diabetes mellitus) results from insulin deficiency due to autoimmune destruction of the β-cells of the islets of Langerhans in the pancreas. Insulin deficiency leads to an inability to control blood glucose levels, and hyperglycaemia develops. Type 1 diabetes is believed to result from a combination of genetic predisposition and an environmental trigger (most probably, infection with an enterovirus). Type 1 diabetes tends to develop mainly in childhood, adolescence or in young adults and accounts for 5-10% of all cases of diabetes.
How does the incidence of type 2 diabetes increase with age?
The incidence of type 2 diabetes increases with age, with most cases being diagnosed after the age of 40 , though there is an increase in younger adults and children developing type 2 diabetes. It is typically associated with lifestyle factors such as overweight/obesity and lack of exercise. Prevalence of diabetes is increasing.
What is diabetes and gum (periodontal) disease?
There are 3 main types: type 1, type 2, and gestational diabetes. Periodontal diseases are infections of the gums and bone that hold the teeth in place. Gum disease is a problem that can happen if you have diabetes that isn't controlled well. Also, the body's response to gum infections can result in blood sugar problems.
What is a periodontist?
These are dentists who are experts in the diagnosis and treatment of gum disease. A periodontist will evaluate your teeth and gums and give you treatment options for your condition. The different stages of periodontal disease are often grouped by the level of inflammation and amount of breakdown. They include:
How is gum disease diagnosed?
To diagnose periodontal disease, a dentist will ask about your health history, current medicines, and any other health conditions you may have. It's very important to share your diabetes history with your dentist, especially how well your blood glucose is controlled. In addition to your health history, the dentist will:
What can I do to prevent gum disease?
Taking care of your teeth and gums correctly can help prevent mouth problems linked to diabetes. These tooth brushing and flossing tips are advised by the American Dental Association:
What is periodontal pocket?
This is when gums pull away from the teeth, causing the small space between the teeth and gums to deepen. It also causes early bone loss around the teeth. Dental care is needed right away to prevent more bone erosion and gum damage.
What are the different types of diabetes?
There are 3 main types: type 1, type 2, and gestational diabetes. Periodontal diseases are infections of the gums and bone that hold the teeth in place. Gum disease is a problem that can happen if you have diabetes that isn't controlled well. Also, the body's response to gum infections can result in blood sugar problems.
Why is dental care needed?
Dental care is needed right away to prevent more bone erosion and gum damage. Moderate to advanced periodontitis. This is the most advanced stage of gum disease. It causes serious bone and tissue loss, and deepening of periodontal pockets. There may be receding gums around the teeth, heavy bleeding, and bad breath.
Why do diabetics have increased risk of developing the condition?
Diabetics generally have a heightened risk of developing gum disease because they are more likely, as a rule, to develop bacterial infections. There are a couple of reasons for this:
Can diabetes cause gum disease?
There are certain medical conditions that can affect your gum health and make you more susceptible to gum disease. Periodontal disease and diabetes, unfortunately, often go hand in hand. Following many medical studies over several decades, the link between diabetes and gum disease has been shown time and time again.
Does diabetes increase the risk of periodontal disease?
Diabetes mellitus and periodontal diseases. Diabetes increases the risk of periodontal diseases , and biologically plausible mechanisms have been demonstrated in abundance. Less clear is the impact of periodontal diseases on glycemic control of diabetes and the mechanisms through which this occurs.
Does periodontal disease affect glycemic control?
Less clear is the impact of periodontal diseases on glycemic control of diabetes and the mechanisms through which this occurs. Inflammatory periodontal diseases may increase insulin resistance in a way similar to obesity, thereby aggravating glycemic control.
How to prevent diabetes and oral health?
Diabetes and Oral Health. Visit your dentist for regular checkups to prevent problems. A healthy mouth is important for everyone, but high blood sugar can make it harder to keep your mouth healthy. If you have diabetes, learn how you can avoid oral health problems and keep a smile on your face. Taking good care of your mouth is essential ...
Why does my mouth feel dry after diabetes?
Here’s a quick look at how diabetes can take its toll on your oral health: You may have less saliva, causing your mouth to feel dry. (Dry mouth is also caused by certain medicines.) Your gums may become inflamed and bleed often (signs of gum disease). Infections in your mouth can take longer to heal.
How to keep diabetes on track?
Follow your diabetes care schedule to help stay on track. Brush your teeth at least twice a day with fluoride toothpaste. Floss your teeth at least once a day. Tell your dentist if you have diabetes.
What happens if you smoke and your gums bleed?
Other signs include dry mouth, loose teeth, or mouth pain. If you smoke, quit. Smoking increases your risk of gum disease and can worsen your diabetes. Learn More.
Does high blood sugar affect white blood cells?
High blood sugar can weaken white blood cells . These are your body’s main way to fight infections that can occur in the mouth. Keep that smile on your face, though! By managing your diabetes, you manage more than your blood sugar—you’re helping to prevent gum disease and other infections in your mouth.
Can sugar cause tooth decay?
Bacteria in plaque, a sticky film, use sugar as food. Some of this bacteria can cause tooth decay, cavities, and gum disease. If the tooth is not treated, it can also lead to tooth loss.
