How does pressure support improve ventilation? Pressure support ventilation (PSV
PSV
The Philips Sport Vereniging, abbreviated as PSV and internationally known as PSV Eindhoven is a sports club from Eindhoven, Netherlands, that plays in the Eredivisie, the top tier in Dutch football. It is best known for its professional football department, which plays in the Eredivisie since it…
What is the ventilator effect of increased pleural pressure and lung volume?
The ventilator effect of increased pleural pressure and lung volume depends on the patient’s condition. If he is dehydrated, positive pressure ventilation may reduce blood flow to the kidneys, which will trigger a further blood pressure drop.
What happens to blood pressure when a patient is on ventilator?
If he is dehydrated, positive pressure ventilation may reduce blood flow to the kidneys, which will trigger a further blood pressure drop. If lung inflation increases with ventilator breaths, this can relax the muscle tone inside the blood vessels, leading to dilation of the arteries and reduction in blood pressure.
What are the cardiovascular effects of positive pressure ventilation?
This chapter specifically addresses the cardiovascular effects which were asked about in Question 20 from the second paper of 2019. In short, positive pressure ventilation affects preload, afterload and ventricular compliance, and the effect in most situations is a decrease in cardiac output.
How does mechanical ventilation affect the cardiovascular system?
The specific effect of ventilation on the cardiovascular system varies with the patient’s kidney and heart function, as well as vascular tone. In any case, blood pressure changes related to mechanical ventilation will manifest themselves at the beginning or end of the ventilatory support.
How does pressure affect inhalation and exhalation?
Contraction and relaxation of the diaphragm and intercostals muscles (found between the ribs) cause most of the pressure changes that result in inspiration and expiration. These muscle movements and subsequent pressure changes cause air to either rush in or be forced out of the lungs.
How does pressure influence breathing?
During inhalation, the volume of the lungs increases and the pressure inside the lungs decreases below that of atmospheric pressure. This creates a pressure gradient that draws air into the lungs.
What are the 3 pressures that determine ventilation?
Pulmonary ventilation is dependent on three types of pressure: atmospheric, intra-alveolar, and interpleural.
How does pressure and volume relate to ventilation?
In general, volume control favours the control of ventilation, and pressure control favours the control of oxygenation. Volume and pressure control modes have distinct advantages and disadvantages which are mainly related to the flow and pressure patterns of gas delivery.
Does a bigger pressure difference increase or decrease the airflow?
This again creates a pressure gradient, which will push the air from the alveoli out into the atmosphere. While airflow is increased by increasing the pressure difference, it is however, decreased by increasing airway resistance. Airway resistance is influenced by three main factors.
Does pressure play an important part in breathing?
Pressure is an important function supporting respiration. A pressure gradient is required to generate respiration flow.
What is pressure limit in ventilator?
Pressure limits In pressure-controlled ventilation, a pressure limit is the control variable for the respiratory cycle. For example, in a pressure control mandatory mode of ventilation, the pressure limit may be set as 20 cmH2O, above a PEEP of 10.
What causes high peak pressures on ventilator?
Peak inspiratory and plateau pressures Elevations in airway pressure can thus be thought of being caused by increases in airway resistance and/or decreases in lung compliance.
What is the normal pressure of a ventilator?
Normal plateau pressure is below 30 cm H20, and higher pressure can generate barotrauma.
How do you use pressure control ventilation?
Set the ventilator mode to assist control, and match the f, FiO2, PEEP, and I:E ratio to the VCV settings. Set the initial inspiratory target pressure at 75% of the difference between Ppeak and PEEP while on VCV. Increase set inspiratory pressure until the desired Vt is obtained.
What is the relation between volume and pressure?
For a fixed mass of an ideal gas kept at a fixed temperature, pressure and volume are inversely proportional. Or Boyle's law is a gas law, stating that the pressure and volume of a gas have an inverse relationship. If volume increases, then pressure decreases and vice versa, when the temperature is held constant.
What happens to the pressure in your chest cavity when you inhale?
When the lungs inhale, the diaphragm contracts and pulls downward. At the same time, the muscles between the ribs contract and pull upward. This increases the size of the thoracic cavity and decreases the pressure inside.
What happens when pressure increases in lungs?
As a result of an increase in alveolar pressure within the lung due to either fluid accumulation or inflammation, there becomes a net increase in transpulmonary pressure, which prevents airflow and lung expansion during inspiration.
What is the relationship between blood pressure and breathing rate?
It has been reported that deep breathing could reduce blood pressures (BP) in general. It is also known that BP is decreased during inhalation and increased during exhalation. Therefore, the measured BPs could be potentially different during deep breathing with different lengths of inhalation and exhalation.
How does lung pressure work?
When you inhale, the diaphragm and muscles between your ribs contract, creating a negative pressure—or vacuum—inside your chest cavity. The negative pressure draws the air that you breathe into your lungs.
How does Boyle's law affect breathing?
Boyle's law explains that pressure and volume are always inversely proportional at a given temperature of a gas. It explains that when the volume of the lung increases during inspiration, the pressure in the lung will decrease. This causes air at atmospheric pressure to rush in and fill the lung.
What is positive pressure ventilation?
Positive pressure ventilation is a form of respiratory therapy that involves the delivery of air or a mixture of oxygen combined with other gases by positive pressure into the lungs. As gas enters the lungs, the interalveolar pressure increases until a change in flow or pressure are detected by the machine delivering the mixture, ...
How do invasive ventilators work?
In order to initiate invasive positive pressure ventilation, a patient must either be intubated with an endotracheal tube or ventilated through a tracheostomy tube. Once an artificial airway is acquired, a circuit is connected to a ventilator machine, and the patient’s work of breathing is either supported (by a mode of ventilation called pressure support ventilation) or completely taken over. There are about 47 different mode names and multiple ventilator models that are discussed in separate articles. However, all of these ventilators work on the same principles in that they provide oxygenation and ventilation to a patient by insufflating air or other gas mixture into the lungs. [8]
Why do people need sedation when on a ventilator?
Patients that require mechanical ventilation often need sedation due to the stimulating nature of the endotracheal tube. Likewise, the act of being on a ventilator can be a traumatic experience. Some patients that are in desynchrony with the ventilator, colloquially known as “fighting the vent,” may require paralytic medications such as rocuronium, vecuronium, or cisatracurium so that they can be safely ventilated to treat their underlying condition. However, important neurochemical changes occur within patients’ bodies, such as the depletion of bioenergetic neuron reserves, altered sodium channel activation, and increased inflammatory cytokines, which lead to changes such as atrophy of the diaphragm or critical illness myopathy. [16][17]
Why is it important to intubate a patient?
Other issues that arise include eye irritation, dry airway passages, and gastric distention.[19] Thus, if there is any concern for aspiration, it is safer to intubate a patient to protect their airway and to avoid gastric distention.
What is breath during PPV?
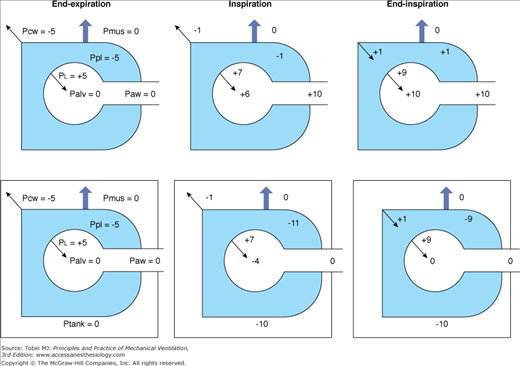
In the most technical sense, a breath during PPV can be characterized by changes in pressure, volume, and flow during inspiration and expiration. These principles can be mathematically defined by a simple equation:[4]
Is emergent endotracheal intubation contraindicated?
However, the need for emergent endotracheal intubation is a contraindication to NIPPV and may be required for conditions such as cardiac arrest, hemodynamic instability, the inability of the patient to cooperate, or maintain an open and protected by reflexes airway, as well as many others to be discussed further.
Which system of the airway affects the flow of air?
The mucosa, cartilages, neural, and lymphatic system of upper airways affect the flow and physical qualities of the air that is inhaled.[3] . Likewise, they have an impact on the delivery of positive pressure ventilation.
How does ventilator breathing affect pleural pressure?
If he is dehydrated, positive pressure ventilation may reduce blood flow to the kidneys, which will trigger a further blood pressure drop. If lung inflation increases with ventilator breaths , this can relax the muscle tone inside the blood vessels , leading to dilation of the arteries and reduction in blood pressure. Those already at risk for decreased vascular tone, including those in septic or neurogenic shock, are especially vulnerable to this process.
What is pleural pressure?
The pleural pressure refers to the pressure between the membranes surrounding each lung. With normal inspiration, that pressure decreases as a person breathes in. When the same person is on a ventilator setting that features positive end expiratory pressure (PEEP), the pleural pressure increases.
Does PEEP increase blood pressure?
The blood pressure then increases .
Does mechanical ventilation affect blood pressure?
Changes in blood pressure associated with mechanical ventilation may confound the medical observer. The specific effect of ventilation on the cardiovascular system varies with the patient’s kidney and heart function, as well as vascular tone. In any case, blood pressure changes related to mechanical ventilation will manifest themselves at ...
How does positive pressure ventilation affect preload?
In short, positive pressure ventilation affects preload, afterload and ventricular compliance, and the effect in most situations is a decrease in cardiac output. However, the effect may be beneficial in the context of decompensated heart failure, where the decreased preload and afterload result in a return to a more productive part ...
What are the physiological consequences of intermittent positive pressure ventilation?
In short, positive pressure ventilation affects preload, afterload and ventricular compliance, and the effect in most situations is a decrease in cardiac output. However, the effect may be beneficial in the context of decompensated heart failure, where the decreased preload and afterload result in a return to a more productive part of the Starling curve. In this rests the chief benefit of CPAP in the management of acute pulmonary oedema.
What is the pressure of a patient with spontaneous inspiration?
The healthy spontaneously breathing patient with good lung compliance and normal tidal volumes generates a negative pressure in the realm of 1-2 mmHg, which is miniscule compared to the pressures generated by the mighty left ventricle (given that normally one must generate a pressure of around 80 mmHg just to open the aortic valve). The effect of increased LV preload due to spontaneous inspiration is in fact far more important, and tends to increase the stroke volume. The tiny increase in the afterload is lost in the noise, and the net effect is still positive.
What causes a decrease in afterload?
Decreased afterload due to a reduction in LV end-systolic transmural pressure and an increased pressure gradient between the intrathoracic aorta and the extrathoracic systemic circuit
Why does the right ventricle fail?
Consequently, if the PEEP is too high, the right ventricle will begin to fail due to increased afterload. The fact that by this stage preload is also decreased doesn't help.
What happens when you put pressure on the aorta?
Additionally, putting positive pressure on the intrathoracic aorta causes a pressure gradient to develop between this vascular compartment and the extrathoracic circulatory system (which is under atmospheric pressure). The resulting gradient favours the flow of blood into the systemic circulation, also decreasing LV workload.
How much of the PEEP is transmitted to the central veins?
In a lung with normal compliance, no more than 25% of the PEEP is transmitted to the central veins. But however small, there is still an effect. And of course nobody in the ICU has normally compliant lungs...
