What is the junctional epithelium?
The junctional epithelium is a non-keratinizing stratified squamous epithelium that sticks to the tooth, particularly the enamel via hemidesmosomes and a basal lamina.
How is the junctional epithelium separated from alveolar bone?
Around an implant with healthy peri-implant tissue, the apical portion of the junctional epithelium is consistently separated from the alveolar bone by a zone of non-inflamed, collagen-rich but cell-poor connective tissue. In the collagen-rich zone, the fibers invest in the ……………..Content available in the hard-copy of the website………………
What happens to junctional epithelium during periodontitis?
In the initiation of periodontitis, the junctional epithelium detaches from the tooth surface and converts gradually, by sprouting laterally and migrating apically, to pathological pocket epithelium.

How is junctional epithelium enamel attached?
The continuity of epithelial tissue is collapsed by tooth eruption. The junctional epithelium (JE) is attached to the tooth surface by hemidesmosomes, which constitutes the front-line defense against periodontal bacterial infection.
Is junctional epithelium attached to cementum?
Long junctional epithelium created experimentally attaches to the cementum surface by hemidesmosomes and basal lamina. The peri-implant epithelium differs in proliferation and in adhesive structure from the normal junctional epithelium.
How does long junctional epithelium form?
Connective tissue is destroyed during periodontal disease, and the junctional epithelium therefore extends until it reaches intact connective tissue that provides the signal to stop its migration, forming a long junctional epithelium.
How are gingiva attached to the enamel?
The gingival sulcus is bound to the tooth by the enamel of the crown and the sulcular epithelium. The junctional epithelium is immediately apical to the base of the pocket. The JE attaches to the surface of the tooth through the epithelial attachment (EA).
Where is the junctional epithelium attached?
tooth surfaceGenerally, the epithelium, called the junctional epithelium (JE), is directly attached to the tooth surface (enamel) and has a defensive role against continuous bacterial infection.
Where is attached gingiva?
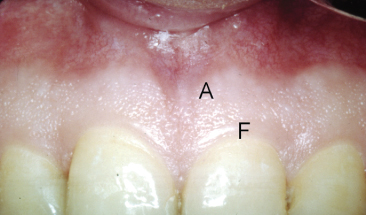
The gingiva surrounds the teeth and the marginal parts of the alveolar bone, forming a cuff around each tooth. It can be divided into the free gingiva, which is closely adapted to the tooth surface, and the attached gingiva, which is firmly attached to the underlying periosteum of the alveolar bone (Figs 4.3, 4.4).
What is junctional epithelium made of?
The junctional epithelium is found at the base of the gingival sulcus and, in a healthy sulcus, defines this base. The junctional epithelium is made up of mostly flattened epithelial cells that are layered on a basal membrane; only one layer is attached to this basal membrane, and the others adhere to one another.
What is clinical attachment level?
The clinical attachment level (CAL) and radiographically assessed bone levels are used to assess the loss of periodontal tissue support in periodontitis, a chronic, multifactorial inflammatory disease of the periodontium.
Does junctional epithelium regenerate?
The regenerating nerve fibers completely bypassed the zone of epithelial down-growth (long junctional epithelium, LJE) that was briefly present along the tooth from 1-3 weeks after injury. The LJE did not have p75-NGFR-IR and was gradually replaced by a modified thicker regenerated junctional epithelium (RJE).
What is epithelial attachment?
Epithelial attachment refers to the mechanism of attachment of the junctional epithelium to a tooth or dental implant, i.e., hemidesmosomes. The cells of the epithelium at this attachment point are non-keratinized and form a collar around the tooth around the cemento-enamel junction.
What is the difference between sulcular and junctional epithelium?
The junctional epithelium (JE) lies immediately apical to the sulcular epithelium. The sulcular epithelium lines the gingival sulcus from the base to the free gingival margin. This is where it interfaces with the epithelium of the oral cavity.
Why attached gingiva is Keratinized?
The width of keratinized gingiva is an important factor when it comes to dental implants. This is because keratinized gingival tissue can play a role in the long-term support of the implant. It may also aid in maintaining oral health, in preventing gum recession, and in overall esthetics.
What is the junctional epithelium?
The junctional epithelium, a nonkeratinized stratified squamous epithelium, lies immediately apical to the sulcular epithelium, which lines the gingival sulcus from the base to the free gingival margin, where it interfaces with the epithelium of the oral cavity. The gingival sulcus is bounded by the enamel of the crown of the tooth and the sulcular epithelium. Immediately apical to the base of the pocket, and coronal to the most coronal of the gingival fibers is the junctional epithelium. The JE attaches to the surface of the tooth by way of the EA with hemidesmosomes and is, on average, roughly 1 mm in width in the apico-coronal dimension, constituting about one half of the biologic width. The attachment of the JE to the tooth surface can occur on enamel, cementum, or dentin. The position of the EA on the tooth surface is initially on the cervical half of the anatomical crown when the tooth first becomes functional after tooth eruption.
What is the effect of junctional epithelium damage?
Damage to the junctional epithelium results in it being irregular in texture, rather than smooth, at its surface. Most importantly is the formation of pocket epithelium within the periodontal pocket, which is a histopathological characteristic of periodontal disease, having the true apical migration of the EA.
What is the sulcus of the gingival sulcus?
The gingival sulcus is bounded by the enamel of the crown of the tooth and the sulcular epithelium. Immediately apical to the base of the pocket, and coronal to the most coronal of the gingival fibers is the junctional epithelium. The JE attaches to the surface of the tooth by way of the EA with hemidesmosomes and is, on average, ...
How to measure gingival sulcus probing depth?
The probing depth of the gingival sulcus is measured by a calibrated periodontal probe. In a healthy-case scenario, the probe is gently inserted, slides by the sulcular epithelium (SE), and is stopped by the epithelial attachment (EA). However, the probing depth of the gingival sulcus may be considerably different from the true histological ...
What happens to the enamel before the eruption?
Before the eruption of the tooth and after enamel maturation, the ameloblasts secrete a basal lamina on the tooth surface that serves as a part of the primary EA. As the tooth actively erupts, the coronal part of the fused and surrounding epithelium peels back off the crown.
What is the purpose of the superficial cells of the JE?
The superficial, or suprabasal, cells of the JE serve as part of the EA of the gingiva to the tooth surface. These superficial, or suprabasal, epithelial cells of the JE provide the hemidesmosomes and an internal basal lamina that create the EA, because this is a cell-to-noncellular type of intercellular junction.
What organelles are found in JE cells?
The JE cells have many organelles in their cytoplasm, such as rough endoplasmic reticulum, Golgi complex, and mitochondria, indicating a high metabolic activity. However, the JE cells remain immature or undifferentiated until they die and are shed or lost in the gingival sulcus. Lysosomes are also found in large numbers in JE epithelial cells; enzymes contained within these lysosomes participate in the destruction of bacteria contained in dental biofilm.
What is junctional epithelium?
The junctional epithelium is derived from the reduced enamel epithelium (REE) which occurs during the tooth development. Prior to the eruption of the tooth and after the enamel matures, the ameloblasts secrete a basal lamina on the tooth surface which serves as a part of the primary EA. As the tooth actively erupts, the coronal part of the fused and surrounding epithelium retracts off the crown. The ameloblasts also develop hemidesmosomes for the primary EA and are firmly attached to the enamel surface. The cervical part of the fused tissue, however, remains attached to the neck of the tooth through the primary EA. This fused tissue, which stays near the cementoenamel junction (CEJ), serves as the initial JE of the tooth. This creates the first tissue attached to the tooth surface. This tissue is later replaced by a definitive JE once the root is established.
What is the EA in dental?
In a healthy state, the EA is very strong and acts as a type of seal between the soft gingival tissue and the hard surface of the tooth. The deepest layer of the JE, also known as the basal layer, undergoes constant and rapid cell division.
What is the junctional epithelium?
The junctional epithelium (JE) is the epithelium that is located at the base of the gingival sulcus. A calibrated periodontal probe is used to measure the probing depth of the gingival sulcus. In healthy cases, the probe is slowly inserted, slides past the sulcular epithelium (SE), and is stopped by the epithelial attachment (EA).
Which epithelium is apical to the sulcular epithelium?
The junctional epithelium (JE) lies immediately apical to the sulcular epithelium. The sulcular epithelium lines the gingival sulcus from the base to the free gingival margin. This is where it interfaces with the epithelium of the oral cavity. The gingival sulcus is bound by the enamel on the crown of the tooth and the sulcular epithelium.
What is the sulcus of the gingival sulcus?
The gingival sulcus is bound by the enamel on the crown of the tooth and the sulcular epithelium. The junctional epithelium is immediately apical to the base of the pocket, and coronal to the most coronal of the gingival fibers. The JE is attached to the surface of the tooth with the EA. On average, the JE is roughly 1 mm wide in ...
Which epithelium is responsible for transmission of white blood cells?
Structure. Cells in the junctional epithelium typically have wide intercellular spaces and fewer desmosomal junctions. This allows the transmission of white blood cells (WBCs) from the lamina propria's blood vessels to the bottom of the gingival sulcus which helps prevent disease.
What is the fused tissue of a tooth?
The cervical part of the fused tissue, however, remains attached to the neck of the tooth through the primary EA. This fused tissue serves as the initial JE of the tooth. It also creates the first tissue that attaches to the tooth’s surface. This tissue is eventually replaced by a definitive JE once the root is formed.
How thick is the JE?
In addition, the JE is thinner than the sulcular epithelium, and ranges from only 15 to 30 cells thick at the floor of the gingival sulcus. It then tapers to a thickness of 3 to 4 cells at its apical part. The superficial cells of the JE serve as part of the EA of the gingiva to the tooth surface.
How many cells are in the junctional epithelium?
General and microscopic features of junctional epithelium: Its thickness varies from 15-18 cell s at the base of the gingival sulcus to 1-2 cells in its most apical portion. Cells are arranged in the base and the suprabasal layers only.
What are the cytokeratins in the junctional epithelium?
As already stated, junctional epithelial cells exhibit a unique set of cytokeratins including cytokeratin 5, 13, 14 and 19. Occasionally, the weak activity of cytokeratins 8, 16 and 18 is also seen 103. As compared to other epithelia, junctional epithelial cells are interconnected by a few desmosomes and occasionally by gap junctions 46, 104-106. These features account for the remarkable permeability of the junctional epithelium.
How long does it take for gingival cells to regenerate?
Epithelial cells in the attached gingiva exhibited a renewal rate of 10.4 days, whereas the corresponding rate for the epithelial cuff was 5.8 days 157. In another study, autoradiography was used to study the rate of migration of attachment epithelium. The authors observed that the rate was comparable to the rate of tooth eruption, suggesting that the location of the attachment is relatively stable 92.
How long does it take for the junctional epithelium to heal after flossing?
The results of the study revealed that detachment of cells persisted for 24 hours after cessation of flossing. New attachment of junctional epithelial cells started 3 days after cessation of flossing. After 2 weeks, the cell populations on the experimental and control surfaces were again indistinguishable from each other 150.
Why does my junctional epithelium lose?
Usually, it occurs due to accidental trauma during brushing, flossing or eating. Intentional trauma occurs during periodontal surgeries where the junctional epithelium is completely lost. Many studies have been done to investigate the renewal of junctional epithelium.
What is the innermost layer of suprabasal cells?
The innermost layer of suprabasal cells (facing the tooth surface) are called DAT cells (directly attached to the tooth) 101. Lysosomal bodies are found in large numbers in the junctional epithelial cells. The enzymes contained within these lysosomes participate in the eradication of bacteria 102.
What happens to the enamel when a tooth is erupted?
With the eruption of the tooth, the reduced enamel epithelial cells unite with proliferating oral epithelium. As a result, the epithelial cells adjacent to the enamel surface produce a cornified layer. Gottlieb called this layer as “secondary enamel cuticle”. This layer subsequently becomes separated from the tooth surface, leaving a V-shaped groove, the gingival crevice.
What is the junctional epithelium attached to?
The junctional epithelium (JE) attached to tooth (to enamel or cementum (C) as in (b) forms a structural barrier against the bacterial plaque. Polymorphonuclear leukocytes that cover the plaque (P) have migrated through the junctional epithelium into the sulcus.
What is the development of the junctional epithelium?
DEVELOPMENT OF JUNCTIONAL EPITHELIUM 1. Formation of reduced enamel epithelium 2. Union of REE and Oral epithelium 3. As the tooth erupts REE is converted into JE Changes during conversion Cuboidal cells derived from ameloblast begin to flatten and align parallel to tooth surface and take appearance of JE.
What is primary epithelial attachment?
Primary epithelial attachment refers to the epithelial attachment lamina released by the REE. It lies in direct contact with enamel and epithelial cells attached to it by hemi-desmosomes. When REE cells transform into JE cells the primary epithelial attachment becomes secondary epithelial attachment . It is made of epithelial attachment between basal lamina and hemi-desmosomes.
What is the epithelial attachment apparatus?
33. Epithelial Attachment Apparatus: The attachment of the JE to the tooth is mediated through an ultramicroscopic mechanism defined as the Epithelial Attachment Apparatus. It consists of hemidesmosomes at the plasma membrane of the cells Directly Attached to Tooth (DAT cells) and a basal lamina-like extra-cellular matrix, termed the internal basal lamina on the tooth surface.
What is the base of the sulcus?
The base of the sulcus is on the cementum, a portion of which is exposed. Proliferation of the junctional epithelium onto the root is accompanied by degeneration of gingival and periodontal ligament fibers and their detachment from the tooth. The cause of this degeneration is not understood.
What is the mucosal epithelium?
Introduction: Mucosal epithelia are composed of continuously dividing and shedding populations of keratinocytes. The junctional epithelium is attached to the tooth surface by a distinct mechanism known as the epithelial attachment apparatus. 5.
How many layers are there in the junctional epithelium?
16. What is Junctional Epithelium? It is 3 to 4 layers thick in early life, but the number of layers increases with age to 10 or even 20 years. JE tapers from its coronal end, which may be 10 to 29 cells wide to 1 or 2 cells at its apical termination, located at the cemento enamel junction in healthy tissue.